COGNITIVE REHABILITATION
advertisement
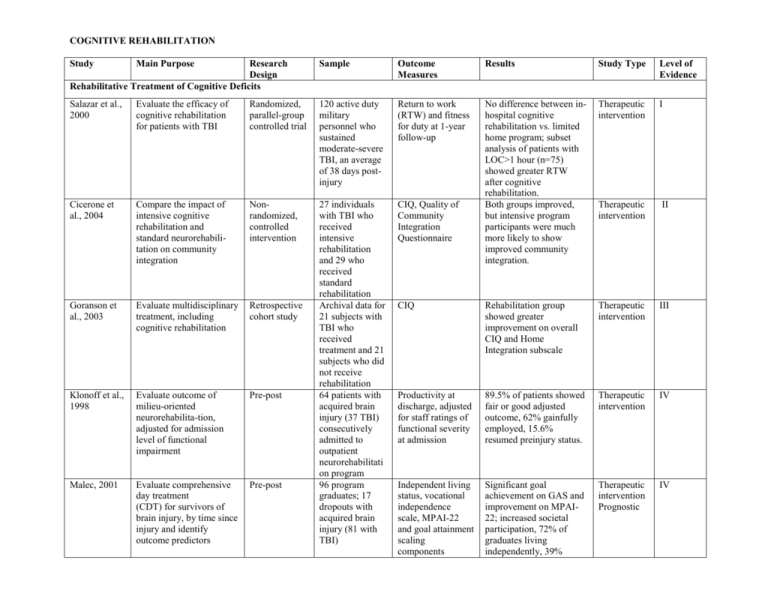
COGNITIVE REHABILITATION Study Main Purpose Research Design Rehabilitative Treatment of Cognitive Deficits Sample Outcome Measures Results Study Type Level of Evidence Salazar et al., 2000 Evaluate the efficacy of cognitive rehabilitation for patients with TBI Randomized, parallel-group controlled trial 120 active duty military personnel who sustained moderate-severe TBI, an average of 38 days postinjury Return to work (RTW) and fitness for duty at 1-year follow-up Therapeutic intervention I Cicerone et al., 2004 Compare the impact of intensive cognitive rehabilitation and standard neurorehabilitation on community integration Nonrandomized, controlled intervention CIQ, Quality of Community Integration Questionnaire Therapeutic intervention II Goranson et al., 2003 Evaluate multidisciplinary treatment, including cognitive rehabilitation Retrospective cohort study CIQ Rehabilitation group showed greater improvement on overall CIQ and Home Integration subscale Therapeutic intervention III Klonoff et al., 1998 Evaluate outcome of milieu-oriented neurorehabilita-tion, adjusted for admission level of functional impairment Pre-post Productivity at discharge, adjusted for staff ratings of functional severity at admission 89.5% of patients showed fair or good adjusted outcome, 62% gainfully employed, 15.6% resumed preinjury status. Therapeutic intervention IV Malec, 2001 Evaluate comprehensive day treatment (CDT) for survivors of brain injury, by time since injury and identify outcome predictors Pre-post 27 individuals with TBI who received intensive rehabilitation and 29 who received standard rehabilitation Archival data for 21 subjects with TBI who received treatment and 21 subjects who did not receive rehabilitation 64 patients with acquired brain injury (37 TBI) consecutively admitted to outpatient neurorehabilitati on program 96 program graduates; 17 dropouts with acquired brain injury (81 with TBI) No difference between inhospital cognitive rehabilitation vs. limited home program; subset analysis of patients with LOC>1 hour (n=75) showed greater RTW after cognitive rehabilitation. Both groups improved, but intensive program participants were much more likely to show improved community integration. Independent living status, vocational independence scale, MPAI-22 and goal attainment scaling components Significant goal achievement on GAS and improvement on MPAI22; increased societal participation, 72% of graduates living independently, 39% Therapeutic intervention Prognostic IV Seale et al., 2002 Evaluate changes in community integration for survivors of TBI who participated in post-acute rehabilitation Pre-post Sohlberg et al., 2000 Evaluate Attention Process Training (APT), compared with a brain injury education “placebo” Randomized, crossover design with parallel-group analyses Fasotti et al., 2000 Evaluate Time Pressure Management (TPM) to compensate for slowed processing, compared with generic concentration instructions Randomized, parallel-group controlled trial Berg et al., 1991 Evaluate the efficacy of memory strategy training, compared with ‘pseudotreat-ment’ (drill and practice) and notreatment conditions Evaluate visual imagery for remediation of memory deficits, compared with ‘pragmatic’ memory training Randomized, parallel-group controlled trial Evaluate memory notebook training, compared with supportive Randomized, parallel-group controlled trial Kaschel et al., 2002 SchmitterEdgecombe et al., 1995 Randomized, parallel-group controlled trial 71 subjects with TBI who participated in a postacute rehabilitation program 14 subjects with acquired brain injury (12 TBI), more than 1 year post injury 22 subjects with severe to very severe TBI, at least 3 months post-injury, referred to one rehabilitation center 39 subjects with mild memory impairment, most at least 1 year post TBI 21 subjects with acquired brain injury (12 TBI) with mild memory impairments, at least 6 months post injury 8 subjects with TBI, with mild memory CIQ Standardized questionnaires, data from structured interviews, standardized and non-standardized neuropsychological tests Standardized behavioral observations of strategy use, standardized neuropsychological tests Standardized memory testing, subjective report of memory functioning Observed and selfreported memory failures Standardized neuropsychological tests of working independently, 10% in transitional placements, 18% in supported or volunteer work. Significant improvement on CIQ and all subscales. Clinically significant improvement on CIQ total for 46% of subjects; 49% no change; 4% got worse APT related to significantly greater improvement on 3 of 5 neuropsychological tests; significantly more changes reported in memory and attention. Therapeutic intervention IV Therapeutic intervention I TPM produced significant increase in use of management strategy and summary measure of cognitive function. Therapeutic intervention I Both treatment groups reported subjective improvement; objective improvement of memory function apparent only after strategy training. Visual imagery produced domain-specific benefits on retention of verbal information. Therapeutic intervention I Therapeutic intervention I Notebook training related to fewer self-reported everyday memory failures Therapeutic intervention I therapy Levine et al., 2000 Evaluate problem-solving training, compared with motor skills training Rath et al., 2003 Compare an “innovative” group treatment of problem-solving deficits with “conventional” neuropsycho-logical treatment impairment, more than 2 years post injury attention and memory; selfreported everyday memory failures Standardized and non-standardized neuropsychological tests after treatment; difference between groups no longer apparent at 6-month follow-up. Problem solving training related to specific improvements on nonstandardized tests. Randomized, parallel-group controlled trial (no masked outcome assessment) Randomized, parallel-group controlled trial (no direct comparison of treatment conditions) 30 subjects with mild-to-severe TBI, 3 to 4 years post injury Therapeutic intervention III 46 subjects with mild-to-severe TBI, at least 1 year post injury, drawn from a large outpatient treatment program Standardized and non-standardized neuropsychological tests Both groups improved on various measures; innovative problemsolving treatment related to improvement on problem-solving measures. Therapeutic intervention III Randomized, double-blind, parallel-group controlled trial comparing phenytoin for 1 week, VPA for 1 month or VPA for 6 months Single case study 279 consecutive medical center admissions, randomized at 1month postinjury Battery of neuropsychological measures administered at 1 ,6 and 12 months post-injury No significant adverse or beneficial effects of VPA. Therapeutic intervention I 38-year-old man in MCS five months after sustaining a severe TBI 35 adults with moderate or severe TBI recruited within 6 months of injury Coma-Near Coma (CNC) Scale Therapeutic intervention IV Therapeutic intervention III 74 patients with severe TBI admitted to an ICU in coma Glasgow Coma Scale (GCS) and mortality rates Dose-dependent improvement of CNC scores was found after treatment with amantadine. No detrimental effects of amantadine on laboratory studies. Improvement on DRS and FIM-Cog, with no difference between drug and placebo treatments at 12 weeks or 6 months. Higher GCS on discharge from ICR and lower case mortality rates with standard therapy plus Therapeutic intervention II Drug Treatment of Cognitive Deficits Dikmen et al., 2000 Evaluate neuropsychological effects of valproate (VPA) given to prevent post-traumatic seizures Zafonte et al., 1998 Evaluate amantadine in treatment of prolonged minimally conscious state (MCS) Meythaler et al., 2002 Evaluate the safety and efficacy of amantadine in TBI Randomized, double- blind placebocontrolled cross-over design Saniova et al., 2004 Investigate the therapeutic effects of standard therapy alone versus standard therapy plus Retrospective cohort study Disability Rating Scale (DRS), MiniMental Status, GOS, GOAT, FIMCog score amantadine amantadine. Meythaler et al., 2001 Evaluate impact of an SSRI (sertraline) in improving arousal and alertness after TBI Prospective, placebocontrolled, parallel-group design Whyte et al., 2004 Evaluate the effects of methylphenidate on attention deficits after TBI Randomized, double-blind, placebocontrolled, repeatedmeasures cross-over design; withinsubjects analyses only Whyte et al., 1997 Evaluate the effects of methylphenidate on attention deficits after TBI Zhang et al., 2004 Examine effects of donepezil on short-term memory and sustained attention Randomized, double-blind, placebocontrolled, repeatedmeasures cross-over design; withinsubjects analyses only Randomized, double-blind, placebocontrolled cross-over design Taverni et al., 1998 Evaluate the impact of donepezil in acute TBI rehabilitation Case series Masanic et al., 2001 Evaluate the impact of donepezil in chronic TBI Open label, uncontrolled study 11 patients with severe TBI admitted to inpatient rehabilitation within 2 weeks of injury 34 adults with moderate to severe TBI with attention complaints, in postacute phase of recovery (4 months to 34 years postinjury) Orientation Log, GOAT, Agitated Behavior Scale No differences in rates of recovery between groups. Therapeutic intervention III Various experimental attention measures, including computerized and paper-pencil tests, videotape and observational scoring, caregiver and clinician rating scales 5 experimental measures of attention Significant effects of methylphenidate on 3 of 13 composite attention factors: processing speed, attentiveness during individual work tasks and caregiver ratings. Therapeutic intervention III Significant benefits of methylphenidate on processing speed. Therapeutic intervention III 18 subjects with cognitive impairment enrolled from out-patient neurorehabilitati on clinics, 2 to 24 months postTBI 2 persons with TBI admitted to acute inpatient rehabilitation Standardized neuropsychological tests of immediate memory (WMS-III) and attention (PASAT) Significant benefits of donepezil on immediate memory and attention. Therapeutic intervention I Family interviews, memory testing Therapeutic intervention IV 4 outpatients with chronic TBI symptoms Verbal learning, short-term and long-term recall Improvement of memory, both subjectively and objectively assessed, within 3 weeks of start of medication. Significant improvement in tests of verbal learning and short-term and long- Therapeutic intervention IV 19 adults with perceived attention problems after TBI term recall. Morey et al., 2003 Investigate the effectiveness of donepezil in treating memory deficits after TBI ABAC drug trial 7 persons who had sustained TBI at least 1.5 years prior Horsfield et al., 2002 Evaluate the role of fluoxetine in the outpatient TBI setting Evaluate the impact of bromocriptine in experimental chronic TBI Open label, uncontrolled study Controlled animal trial 5 outpatients with TBI Powell et al., 1996 Evaluate the effects of bromocriptine on deficits in clinical motivation and frontal cognitive function Repeatedmeasures open trial Schneider et al., 1999 Evaluate the efficacy of amantadine in improving cognitive and behavioral performance after TBI Randomized, double-blind, placebocontrolled cross-over design 10 adults with TBI receiving acute brain injury rehabilitation Examine the utility of neuropsycho-logical measures of executive functioning as predictors of functional ability and social integration Prospective, descriptive study 90 consecutive admissions to TBI (45), orthopedic (13) and spinal cord (32) inpatient rehabilitation units Kline et al., 2002 Male rats, given cortical impact injury and, in experimental group, daily bromocriptine 24 h later 11 patients (8 TBI, 3 subarachnoid hemorrhage) receiving rehabilitation Hopkins Verbal Learning, Wechsler Adult Intelligence Scale, Controlled Oral Word Association Test (COWAT) Working memory tasks, assessment of mood Cellular studies, animal memory tests Significant improvement in tests of immediate and delayed memory, at doses of 10 mg/day. Therapeutic intervention III Improved mood and performance on working memory tasks. Bromocriptine improved working memory and spatial acquisition skills; experimental group had improved preservation of CA3 neurons. Therapeutic intervention IV Therapeutic intervention (animal model) NA Experimental measures of therapy participation and responsiveness to reward, standardized neuropsychological tests of cognitive function and mood Standardized neuropsychological tests Improved scores on all measures except mood; improvement remained even after bromocriptine withdrawal in 8 of 11 patients. Therapeutic intervention IV No significant difference between amantadine and placebo. Therapeutic intervention I CIQ, DRS, SF-36 Neuropsychological measures of memory and executive function were significant predictors of CIQ and DRS at 6 months after inpatient rehabilitation. Prognostic II Prognosis Hanks et al., 1999 Millis et al., 2001 Describe neuropsychological outcome 5 years after injury in persons with TBI who received inpatient rehabilitation Longitudinal cohort study, using TBI Model System data 182 subjects with complicated mild-to-severe TBI Standardized neuropsychological measures, administered 1 and 5 years after injury Ezrachi et al., 1991 Identify factors that predict who will benefit vocationally from a neuropsycho-logical rehabilitation program Prospective, descriptive study 59 people with moderate-tosevere TBI who participated in a holistic neuropsychologi cal rehabilitation program Employability ratings at discharge, actual vocational status 6 months later Tenovuo, 2005 Examine the clinical experience of persons given ACE in the treatment of TBI Open label, multiple-arm trial of donepezil, galantamine and rivastigmine 111 outpatients with chronic TBI and persistent attention, memory, fatigue or initiation complaints Fatigue measures, general memory and attention Age and length of PTA significant predictors of Trail B performance at 5 years postinjury; memory function (RAVLT) at 1 year predicted improvement at Year 5. Neurologic (length of coma), neuropsychological (verbal memory, visual processing, verbal aptitude) and group process (regulation of affect, self-appraisal, acceptance of program) measures all contributed to predicting outcome. Prognostic III Prognostic III 61% with a significant positive response to medications, 39% with modest improvement. No differences between the three ACE drugs Therapeutic intervention III