Standardized assessments for TBI-Turstra companion article on
advertisement
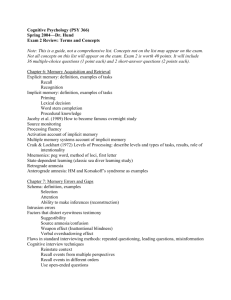
Standardized assessments for TBI-Turstra companion article on nonstandardized assessment is also included in this issue of Seminars in Speech and Language. VOLUME 26, NUMBER 4 2005 This is particularly true in cognitive-communication disorders, in which the core feature is that impairments in underlying cognitive processes such as working memory, self-regulation, and divided attention are manifest in difficulties in listening, speaking, reading, and writing. Thus, a critical requirement of a standardized test for individuals with TBI is that it considers the relation of cognition to communication in its construction and that it measures what the test authors claim to measure. American Speech Language Hearing Asso- ciation Functional Assessment of Commu- nication Skills in Adults (ASHA-FACS14) Behavior Rating Inventory of Executive Function (BRIEF15) Communication Activities of Daily Living, Second Edition (CADL-27) Functional Independence Measure (FIM; Uniform Data System for Medical Rehabil- itation16)* Repeatable Battery for the Assessment of Neuropsychological Status (RBANS 17) Test of Language Competence–Extended (TLC-E18) Western Aphasia Battery (WAB19) * * * * * * A promising development in this regard is the recent publication of the Functional Assessment of Verbal Reasoning and Executive Strategies,20 which was designed specifically for the assessment of cognitive- communication skills in activities that require reading, writing, and reasoning. The general consensus of these experts was that standardized tests should be viewed as only one component of an evaluative process that in- cludes multiple sources of information. Appendix A. Standardized Tests Reviewed American Speech Language Hearing Association—Functional Assessment of Communication Skills Aphasia Diagnostic Profiles Behavior Rating Inventory of Executive Function (Parent Report Form) Behavioral Assessment of the Dysexecutive Syndrome Brief Test of Head Injury California Verbal Learning Test–Second Edition California Verbal Learning Test for Children Children’s Orientation and Amnesia Test Clinical Evaluation of Language Fundamentals (Third Edition) Cognitive Linguistic Quick Test Communication Activities of Daily Living (Second Edition) Comprehensive Assessment of Spoken Language Controlled Oral Word Association Subtest Discourse Comprehension Test Functional Independence Measure Galveston Orientation and Amnesia Test LaTrobe Communication Questionnaire Measure of Cognitive-Linguistic Abilities Mount Wilga High Level Language Test Multilingual Aphasia Examination Paced Auditory Serial Addition Test Rancho Los Amigos Levels of Cognitive Functioning Repeatable Battery for the Assessment of Neuropsychological Status Rivermead Behavioral Memory Test Ross Information Processing Assessment (Second Edition) Scales of Cognitive Ability for Traumatic Brain Injury (Normed Edition) The Speed and Capacity of Language Processing Test The Token Test (Shortened Form) he Awareness of Social Inference Test Test of Everyday Attention for Children Test of Language Competence–Extended Western Aphasia Battery Evidence for Cog. Rehab. article methylphenidate improves processing speed after TBI. Direct attention training was defined as the repeated stimulation of attention via graded exercises to improve the underlying neurocognitive system and attention functioning. The authors recommended use of direct attention training in conjunction with metacognitive training (feedback, self-monitoring, strategy use) for postacute or mildly impaired clients with intact vigilance. The authors concluded that treat- ment to establish the use of external aids for memory compensation might be considered a Practice Guideline as a means of improving day-to-day functioning for people with brain injury. Finally, the ANCDS6 conducted a systematic review and meta- analysis of 15 studies addressing interventions for executive functions after TBI. Ten of the studies (including 5 RCTs) utilized metacognitive strategy instructions (eg, for self-monitoring and control of cognitive processes). These studies sup- ported metacognitive strategy training to improve problem solving for personally relevant activities, based on significant effect sizes for activity and participation outcomes compared with control treatments. The review led to the recommendation of a practice standard for the use of metacognitive strategy training with young to middle-age adults with TBI in chronic stages of disability for difficulties with problem solving, planning, and organization. There were several high-quality studies that supported the effectiveness of interventions for attention, communication skills, executive functioning, and comprehen- sive-holistic rehabilitation after TBI, including improvements on participation outcomes. This analysis also noted the value of non-RCTs in providing evidence for the effectiveness of cog- nitive rehabilitation for people with TBI.