Case Study-GI/ Pain - Professional Pediatric Home Care
advertisement
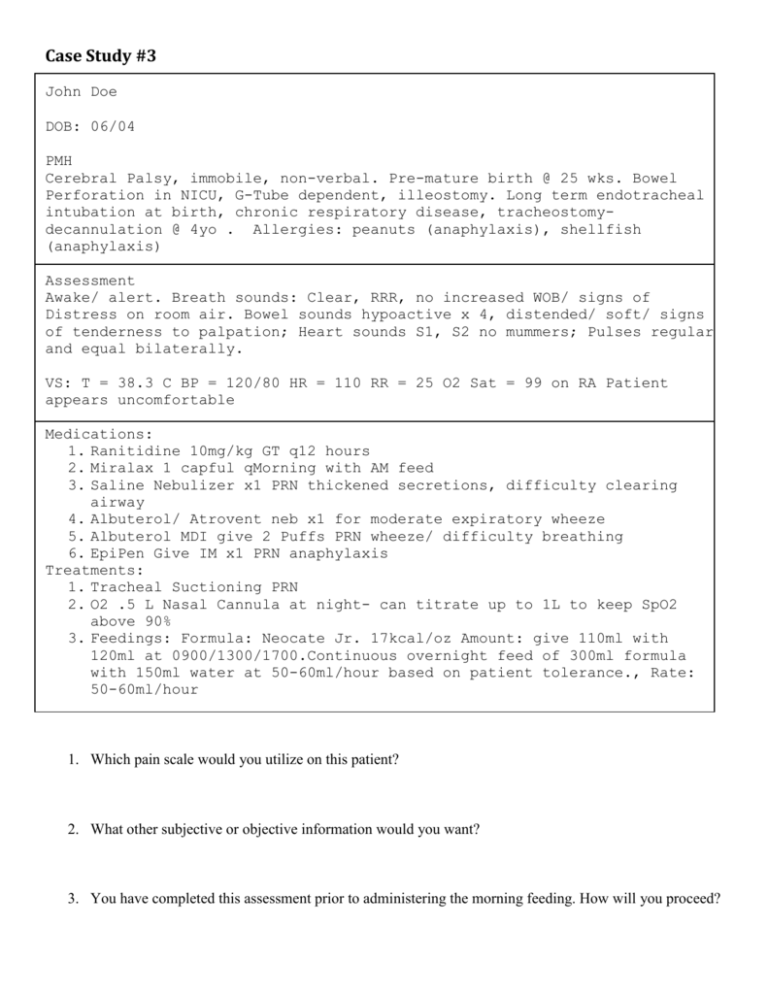
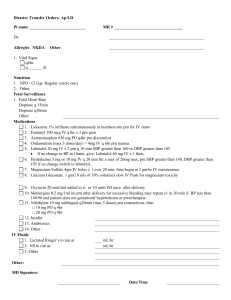
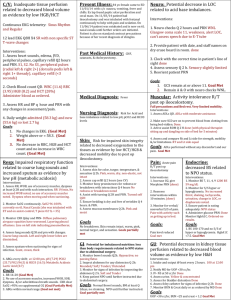
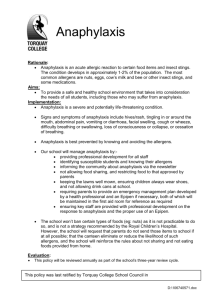
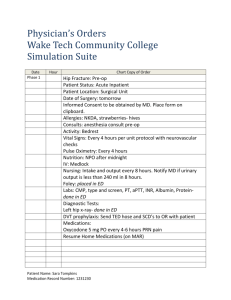
Case Study #3 John Doe DOB: 06/04 PMH Cerebral Palsy, immobile, non-verbal. Pre-mature birth @ 25 wks. Bowel Perforation in NICU, G-Tube dependent, illeostomy. Long term endotracheal intubation at birth, chronic respiratory disease, tracheostomydecannulation @ 4yo . Allergies: peanuts (anaphylaxis), shellfish (anaphylaxis) Assessment Awake/ alert. Breath sounds: Clear, RRR, no increased WOB/ signs of Distress on room air. Bowel sounds hypoactive x 4, distended/ soft/ signs of tenderness to palpation; Heart sounds S1, S2 no mummers; Pulses regular and equal bilaterally. VS: T = 38.3 C BP = 120/80 HR = 110 RR = 25 O2 Sat = 99 on RA Patient appears uncomfortable Medications: 1. Ranitidine 10mg/kg GT q12 hours 2. Miralax 1 capful qMorning with AM feed 3. Saline Nebulizer x1 PRN thickened secretions, difficulty clearing airway 4. Albuterol/ Atrovent neb x1 for moderate expiratory wheeze 5. Albuterol MDI give 2 Puffs PRN wheeze/ difficulty breathing 6. EpiPen Give IM x1 PRN anaphylaxis Treatments: 1. Tracheal Suctioning PRN 2. O2 .5 L Nasal Cannula at night- can titrate up to 1L to keep SpO2 above 90% 3. Feedings: Formula: Neocate Jr. 17kcal/oz Amount: give 110ml with 120ml at 0900/1300/1700.Continuous overnight feed of 300ml formula with 150ml water at 50-60ml/hour based on patient tolerance., Rate: 50-60ml/hour 1. Which pain scale would you utilize on this patient? 2. What other subjective or objective information would you want? 3. You have completed this assessment prior to administering the morning feeding. How will you proceed?