The Clinical Challenges of Treating Catatonia in Pregnancy
advertisement

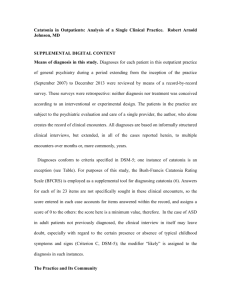
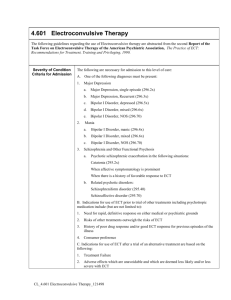
UNIVERSITY OF ILLINOIS AT CHICAGO Department of Psychiatry Fifth Annual Research Forum – Extravaganza 2014 POSTER TITLE The Clinical Challenges of Treating Catatonia in Pregnancy DISEASE/KEY WORDS: Catatonia, Pregnancy AUTHORS: Dr. Amber May, Dr. Marcela Almeida MENTEE CATEGORY: BACKGROUND: RESEARCH MENTOR: There are sparse guidelines for physicians treating pregnant patients with catatonia. This is one of the few reported cases of a pregnant patient with bipolar disorder exhibiting symptoms of psychosis and catatonia which developed after initiating antipsychotics (Haldol). Most of our knowledge of treating catatonia in pregnancy comes from the few published case reports available. METHODS: RESULTS: (Case History) The patient initially presented as an 18 year old African American female G2P1001 at 33.8 wga with a past psychiatric history of bipolar disorder who was admitted to inpatient psychiatry unit for suicidal ideation. The patient exhibited mood lability and bizarre behaviors, including mutism, fixed gaze, poor social boundaries, and sexual preoccupation. After receiving multiple PRNs of Benadryl and Haldol for behavioral management, the patient’s exam was notable for waxy flexibility, abnormal posturing, echopraxia, and utilization behaviors. As catatonia was suspected, PRN Haldol was discontinued and CK levels were ordered. CK returned > 2200, and the patient was treated with IVFs and Ativan PO for emergent treatment of catatonia. The patient intermittently manifested psychotic symptoms, including delusions and paranoia. With continued Ativan treatment, her symptoms improved and the CK trended down; but when an Ativan taper was attempted, the catatonic symptoms worsened along with elevation of CK. ECT was proposed as a treatment option, but the patient and family were uncooperative. After delivery, the patient remained catatonic and psychotic. After a prolonged battle, the mental health court ruled in favor of ECT treatment. The patient improved drastically with symptom resolution after 8 treatments of ECT. She was to be discharged home on Lithium 600 mg qhs with a plan for maintenance ECT as an outpatient. UNIVERSITY OF ILLINOIS AT CHICAGO Department of Psychiatry CONCLUSIONS: This case raised many interesting questions: how to fully assess for catatonic features prior to antipsychotic use, whether or not to treat with ECT during pregnancy, obtaining consent for ECT in patients with catatonia, and approaching families resistant to ECT when it results in prolonged duration of untreated psychosis. In catatonia, antipsychotics are generally avoided. The patient’s catatonia could likely have been due to her psychosis and Haldol PRN exacerbated the symptoms, rather than induced the catatonia. Haldol had been withdrawn for over a month and patient’s symptoms did not resolve completely, despite aggressive treatment with Ativan. After ECT, the patient’s symptoms resolved. Electroconvulsive therapy (ECT) may be the preferred treatment in pregnancy since there are not any known adverse fetal effects. As medication and maternal illness can have adverse effects on the fetus, the clinician-patient dyad try to weigh the risks and benefits of symptoms versus treatment. ECT typically works more quickly and efficaciously than pharmacotherapy. Benzodiazopines have been associated with cleft palate/lip, hypoglycemia, preterm birth, low birth weight, floppy infant syndrome, and neonatal withdrawal symptoms. It would be helpful to establish a protocol for the safest approach to treatment for the pregnant patient and the fetus.