MRSA – Management of Recurrent Skin and Soft Tissue Infection
advertisement

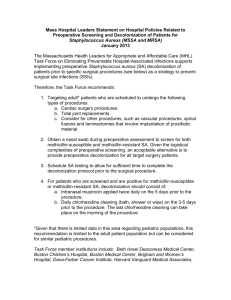
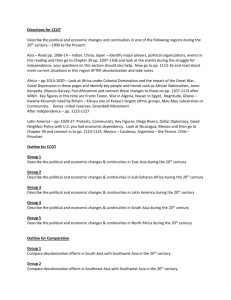
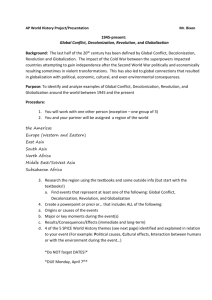
MRSA – Management of Recurrent Skin and Soft Tissue Infection Highlights Policy Statement Strategies for the management of recurrent skin and soft tissue infections (SSTI) with methicillin-resistant Staphylococcus aureus are consistent with current practice guidelines. Policy Interpretation and Implementation Contact Precautions 1. CDC recommends contact precautions when the facility (based on national or local regulations) deems MRSA to be of special clinical and epidemiologic significance. The components of contact precautions may be adapted for use, especially if the resident has draining wounds or difficulty controlling body fluids. Standard Precautions 2. Utilize standard precautions at all times for all resident care. Staff/Resident Education 3. Educate staff and residents about the need for personal hygiene and appropriate wound care, including: a. b. c. d. Environmental Cleaning Procedures 4. Enforce strict environmental cleaning procedures, including: a. b. Possible Decolonization Situations 5. b. 6. Focusing cleaning efforts on high-touch surfaces (e.g., door knobs, counters, bath tubs and showers, toilet seats, etc.); and Using CDC recommended cleaners appropriate for the surface being cleaned. Decolonization may be considered in the following situations: a. Strategies for Decolonization Keeping draining wounds covered with clean, dry bandages; Performing hand hygiene after touching infected area or any item that has been in contact with the wound; Encouraging/assisting resident with regular bathing; and Not allowing residents to share or reuse items that have come in contact with infected skin. A resident develops a recurrent SSTI despite optimizing wound care and hygiene measures; or Ongoing transmission is occurring among residents or other close contacts despite optimizing wound care and hygiene measures. Decolonization requires a physician order. Strategies may include: a. b. Nasal decolonization with mupirocin twice daily for 5–10 days; or Nasal decolonization with mupirocin twice daily for 5–10 days and topical body decolonization regimens with a skin antiseptic solution (eg, chlorhexidine) for 5–14 days or dilute bleach baths. (1) For dilute bleach baths, 1 teaspoon per gallon of water (or ¼ cup per ¼ tub or 13 gallons of water) given for 15 minutes twice weekly for 3 months. continues on next page © 2001 MED-PASS, Inc. (Revised August 2011) Interpersonal Transmission 7. In cases where interpersonal transmission is suspected: a. b. Reinforce personal and environmental hygiene strategies; and Evaluate contacts for evidence of S. aureus infection. (1) Recommend evaluation and treatment of symptomatic contacts; and (2) Recommend the possible decolonization for asymptomatic contacts. Screening Cultures 8. Screening cultures prior to decolonization are not recommended if at least one of the previous infections was due to MRSA. Surveillance Cultures 9. Surveillance cultures following decolonization are not recommended in the absence of active infection. References OBRA Regulatory Reference Numbers Survey Tag Numbers Related Documents Policy Revised 483.65(a); 483.65(b)(1); 483.65(b)(3); 483.65(c) F441 See also: Management of Multidrug-resistant Organisms in Healthcare Settings, 2006 CDC Campaign to Prevent Antimicrobial Resistance in Healthcare Settings (Appendix D) Clinical Practice Guidelines by the Infectious Disease Society of America for the Treatment of Methicillin-Resistant Staphylococcus Aureus Infections in Adults and Children (2011) (Appendix D) Isolation – Categories of Transmission-Based Precautions Date:________________ By:__________________ Date:________________ By:__________________ Date:________________ By:__________________ Date:________________ By:__________________ © 2001 MED-PASS, Inc. (Revised August 2011)