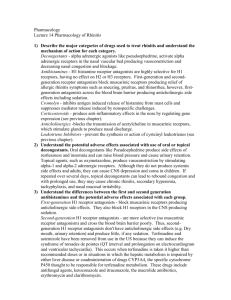
Pharmacology
advertisement

Pharmacology: Units 1-5 Unit 1: Introduction to Pharmacology Targeted Drug Discovery: The researcher knows that target molecule that they want to affect, and then finds or creates a compound that would work on that target molecule. Phonotypical Drug Discovery: The target molecule is not known however, the researchers know what the final effect should be. FDA: Food and Drug Administration approves all new prescription drugs. 15 years for a drug to reach the market. First tested on cells inn cultures, then on animals, then phase one on humans (given to healthy individuals-acute affects/toxicity are tested here), phase two the drug is given to individuals with the target disease (small sample size), phase three the drug is given to a large sample size of individuals with the targeted disease. Chronic care model: treats symptoms only, unable to cure the actual cause Unit 2: Pharmacokinetics Pharmacokinetics: The study of factors that are involved in getting the drug to its target body Pharmacodynamics: The study of mechanism of the action of the drug, the therapeutic and toxicological effects, and the chemical structure-activity relationship. Absorption: The ability of the drug to enter the blood stream (usually from the GI tract ENTERAL) (Parenteral administration –non alimentary routes such as IV or through respiratory system) o Influence in the rate of absorption by: route of administration, dosage forms, circulation at the site of absorption, and concentration of the drug. o Most common way drugs pass through the GI and enter blood stream is through simple diffusion (rate of transfer is directly proportional to the concentration gradient across the membrane) o More lipid soluble the faster the drug will pass through the membrane o Active transport: solute crosses the membrane against the concentration gradient and requires ATP to pass across the membrane. (Small percentage occurs this way) o Distribution: the movement of the drug throughout the body to various tissues. o Vd= amount of drug administered/concentration of drug in plasma, if the Vd is low then the drug is being retained in the bloodstream, if the Vd is high then the drug is being concentrated in the tissues o Rate of blood flow severely limits the distribution of the drug Biotransformation: the chemical alteration of the drug. o Mostly occurs in the liver o Chemical alterations that take place in the liver which are responsible for biotransformation: oxidation, reduction, hydrolysis, conjugation Excretion or Elimination: the ability of the body to remove the drug and its products. o Liver is the primary site for drug excretion o o GI tract and lungs may act as sites for drug elimination If the drug is administered faster than it is eliminated, the drug will accumulate in the body and reach toxic levels o Clearance and half life are used to indicate the rate at which a drug is eliminated Drug concentrations are usually measured by the plasma levels. Drug storage sites: Adipose tissue-primary site for storage, Bone- stores heavy metals and toxins, Muscles- muscle cells in particular, Organs- The liver and kidney Albumin is the principal circulating protein that binds drugs non-specifically (Albumin levels decline with age thus more free active drugs in the blood stream as one ages) Changes noted in distribution of a drug as a person ages: decrease in lean muscle mass, increase in total body fat, decrease on body water, changes in albumin concentrations Clearance is the ability of organs, specifically the kidneys to eliminate drugs Creatinine clearance rates are used to determine if a patient has a renal problem of Half life of a drug is defined as the amount of time required for 50% of the drug remaining in the body to be eliminated or inactivated Module 3: Pharmacodynamics The cellular endpoint is the final effect that the drug was intended to have Efficacy: the ability of a drug to initiate a response subsequent to binding to its target When comparing two drugs, the drug that reached the greatest magnitude, on the Y axis of the dose response curve is the drug that is considered the most efficacious Potency- is the dose of the drug that produces a given response ( lowest value for a given effect on the X axis) ED50 or TD50= the dose of the drug at which 50% of the people resort that they had a positive response to the drug LD50= lethal dose of a drug also known as the toxic dose , this the known as the level and or the dose of the drug in which 50% of the animals tested die Therapeutic index(TI)= The ratio of LD 50/ED50 this is calculated as the dose required to produce toxic effects divided by the dose required to achieve the desired therapeutic effects. The attraction and binding of a drug to a receptor is called the association while the removal is called the disassociation A drug with high affinity binds readily to the receptor, even if the concentration of a drug is low Ka and Kd are not good indicators of drug efficacy Selectivity= how much affinity an agonist has on one receptor versus another Nonselective binding- a drug will bind to any receptor Ligand- compound that binds to a receptor Ligand that is an angonist will bind to a receptor and activate it while a ligand that is an antagonist will bind to a receptor and deactivate it (inhibit it form becoming active) Whooping cough and cholera are disease of G proteins---- don’t need to remember G protein pathway Tyrosine Kinase Receptor- plasma membrane receptor that transmits the signal into the membrane of the cell (can cross multiple times) Channel receptors- FAST no signaling cascade, this is typical in the nervous system Intracellular Receptors- hormones induce a slow response, in order for a drug to bind to an intracellular receptor it must either be lipid soluble so that it can diffuse through the membrane, or it must have a specific transporter within the plasma membrane that carries the drug molecule into the cell Nuclear Receptors- targeted specifically to the nucleus, slower and graded response (hormones usually use this receptors) Desensitization- rapid decrease in responsiveness of a cell to a drug Down regulation – slower process and involves reduction of a number of receptors on the membrane Module 4: Neurological Pharmacology Neurotransmitters: o Acetylcholine: Important in the basal ganglia which controls movement and is implicated in Alzheimer’s disease o Monoamines: Dopamine, histamine, nor epinephrine, serotonin, loss of dopamine is associated with Parkinson’s disease; serotonin may be involved in temperature regulation, sensory perception, sleep control, and mood changes. o Nitric Oxide: transmitter of the GI tract smooth muscle cells and the neurotransmitter in the central nervous system. o Peptides: Substance P, Neurotensin, Endorphin, Bradykinin, Vasopression, Dynorphin, Neuropeptides may act as neurotransmitters or hormones. Neurpeptodes are usually inactive until they are cleaved, their actions are long lasting. Peptides modulate pain perception, regulate temperature, and stimulate contraction of the smooth muscle cells of the gut. o Amino Acids: Glycine, Aminobutyric Acids, GABA, Glutamate, Asparate, Glycine is the simplest amino acid and is an inhibitory neurotransmitter released by interneurons in the spinal cord, GABA is produced from glutamate and is the most common transmitter of the brain, it is an inhibitory transmitter, Glutamate and Aspartate strongly excite the neurons in the brain. Cholinesterase Inhibitors (Aricept, Exelon, Reminyl) – Used for treatment of Alzheimer’s disease, prevents the breakdown of acetylcholine, memory and reasoning Memantine- used for Alzheimer’s disease , binds to neurotransmitter glutamate, antagonist of the NMDA receptor on post synaptic neurons , may be neuro- protective Betaseron-Multiple Sclerosis, inhibits the immune system from attacking itself, sloes progression of the disease and decreases silent lesions Novantrone: immunosupressor, blocks immune system from attacking itself, can only take this drug for three years Leva-Dopa /Carbidopa –Parkinson’s Disease, chemically modified molecule of dopamine which can cross the blood brain barrier where it is then converted into dopamine, given in very high doses , usually given together to decrease the amount of breakdown that might occur Sinemet-Parkinsons Disease, combined drug of Leva-Dopa and Carbidopa, allows more dopamine to reach the brain Amantadine- Parkinsons Disease , facilitates the endogenous release of dopamine Rasagiline- Parkinsons Disease, antioxidant drug which prevents the breakdown of dopamine by inhibiting monoamine oxidase Seligiline- Parkinson’s Disease, antioxidant drug which prevents the breakdown of dopamine Lithium- Bipolar Disorder, an ion that directly decreases the release of amine neurotransmitters and increases their reuptake Depakote-Bipolar disorder, anticonvulsant, most helpful during manic phases Thioxanthenes, Phenothiazines, Butyrophenones(Haldol)- Anti-psychotic drugs, block the central dopamine receptors Serotonine reuptake inhibitors ( Luvox, Prozac, Zoloft)- block the reuptake of the neurotransmitter serotonin Trycyclic Antidepressants: effect the concentration of both serotonin and nor epinephrine Nonbenzodiazepines (Ambien, Estorra, Indiplon)- Insomnia, effects the benzodiazepines receptor MOI Inhibitors- Antidepressants , cause the receptors to become down regulated, acts on enzymes that normally degrade the amine neurotransmitter Paxil- Antidepressant, serotonin reuptake inhibitor Carbamazepine- Epilepsy Vigabatrin- Epilepsy, enhances the effects of GABA Valporic Acid – Epilepsy, blocks high frequency brain activity Ethosuximide- Epilepdy, acts on calcium, sodium, and potassium channels Barbiturates (Lyrica)- Epilepsy, decreases GABA function Benzodiazepines (Diazepam, Valium, Klonopin)- Epilepsy, works on GABA, hyperpolarizes the neuronal membrane Dilantin- Epilepsy, interferes with the movement of sodium across the membrane, stabilizes the membrane of the neuron , decreases the potassium and calcium movement Unit 5: Cardiovascular Parasympathetic- rest digest, Sympathetic- fight or flight Beta Blockers( Labetolol, Corgard, Inderal, Zebeta) –treats angina, hypertension, cardiac arythmias, slows heart rate and decreases force of contraction, binds to the beta andregenic receptors THIS DRUG HAS NEGETIVE EFFECTS ON GLUOSE/INSULIN STATINS(Lipitor, Crestor, Zocor, Lovastatin, Cauduet)-inhibits cholesterol biosynthesis, decreases LDL and increases HDL Asprin( Anti Platelet Drug)- Works through the arachodonic pathway to clock production of thromboxine, blood thinning effects last for 1 week Heparin (Anti-coagulant)- inhibits clot formation, binds all free calcium in blood Nitroglycerin- treats angina pectoris, dilates coronary arteries, prevents ischemia, minimize left ventricle remolding, reduces mortality in patients with acute heart attacks Diuretics- LOOP=BUMEX AND LASIX works on ascending limb of the loop of henle, THIAZIDE=DIURIL, K+ SPARING= ALDACTONE both thiazides and K+ work on distal tubule – all treat hypertension due to a decrease in blood volume then a decrease in peripheral resistance Angiotension-Converting enzyme inhibitor ACE( Lotensin, Vasotec, Altace, Avapro)antihypertensive drugs, they decrease blood pressure, decreases pheriperal resistance and indirectly allows an increase in cardiac output Thrombolytic Agents ( Activase, TPA, Streptokinase)-facilitates the breakdown of clots, usually given 3-6 hours after incident Digitalis(Digoxin)- used to treat heart failure patients, increases myocardial contractility by inhibiting the NA/K+ pump in cardiac cells, thus increasing calcium and increasing contractility, given a very low dose because it can become toxic. Alpha 1 blocker( Cardura)- decrease blood pressure and increases blood flow, very potent and dramatically decreases blood pressure, decreases insulin resistance and improves glucose tolerance, decrease serum triglycerides Bile Acid Sequestrants (Questran)- promotes the excretion of bile acid, lowers LDL, has no effect on HDL Fibric Acid Derivatives- treats high triglycerides levels, decreases LDL and triglycerides as well as raises HDL Nicotonic Acid ( Niacin B3,Niaspan) – Lowers LDL and increases HDL, increases plasma glucose levels and decreases glucose tolerance Anti-Dysarhthymia Drugs ( Sodium Channel Blockers= Norpace, Tambocor, Quinidine) ( Potassium Channel Blockers= Cordarone, Amidarone) ( Calcium Channel Blockers) These drugs treat dysrthymias, these drugs alter membrane potentials of cells, decrease membranes automatically, slow impulse conduction through myocardium thus prolonging refractory periods Calcium Channel Blockers ( Cardizeum, Procardia, Verapamil, Diltiazem)- treats moderate hypertension, decreases resting and contraction concentration, decreases tone of artery, prevents and resolves remodeling of arteries, inhibits plaque formation, decreases contractility of the heart, can cause severe hypotension Module 6: GI Pharmacology The primary function of the GI tract is the absorption and elimination of fluids and nutrients from the diet, separating useful nutritional factors from potential toxins. Many different disease processes act upon the gut, but the symptoms and clinical effects are often similar and not specific to any disorder o Antacids (Maalox, Mylanta, Phillips, Rolaids, Tums) Antacids attempt to neutralize excess stomach acid in the case of heartburn or acid reflux. They are taken by mouth. These drugs typically contain a base such as carbonate with aluminum, magnesium, or calcium. Some types of antacids also contain additional drugs to relieve excess gas. Antacids are frequently used to treat minor GI discomfort after overeating or eating foods that are not appropriate for the person. A common problem with the antacids is feedback to the body that acid in the stomach is too low, thus the body produces more acid to accommodate. This situation does not present a problem while the antacid is in the body, but will create a negative environment when the antacid is passed from the GI tract. o H2 Receptor Antagonists (Tagament, Pepcid AC, Zantac) Works to decrease the amount of acid in the stomach. Histamine is a major regulator of acid secretion in the stomach. The binding of histamine to its receptor activates a cellular proton pump that releases HCl into the stomach. The exact subtype of histamine receptor in the stomach is the H2 receptor. Thus, an H2 antagonist will prevent the histamine-activated release of acid under resting conditions and during stimulation with food. o Proton-Pump Inhibitors (Prilosec, Prevacid, Nexium) They block the hydrogen pump producing stomach acid. PPIs are more effective in reducing acid (up to 90% reduction) than H2 blockers, but they are also more expensive. Possess antibacterial effects against helicobacter pylori infection. o Antibiotics The most common antibiotics prescribed for peptic ulcers are metronidazole, tetracycline, clarithromycin, amoxicillin. In general, antibiotics are only known by their generic name. o Acetylcholine M1 Receptor Antagonists (Pirenzepine/ Gastrozepin) They work by blocking the M1 subtype of muscarinic receptors. Laxatives o Laxatives are prescribed to promote elimination from the bowel and defecation Bulk Forming Laxatives (Methylcellulose/Citrucell, Metamucil) These drugs absorb water and swell within the lower GI tract. The increased size of the compounds stretches the bowel, and stimulates peristalsis. Stimulant Laxatives (Ex-Lax, Dulcolax) They increase fluid accumulation in the small intestines. They should be taken if the bowel is full, but the person feels that they can’t empty it. Also, these drugs should be prescribed when a bulk-forming laxative is inappropriate. Hyperosmotic Laxatives (Epsom Salt, Phillips Milk of Magnesia) Osmotically active substances produce a gradient that draws water into the bowel and small intestines. This gradient increases fluid content and stimulates excretion. Lubricants and Stool Softeners (Colace, Doxidan) Products like mineral oil bring water into the fecal mass, thus softening the stool and permitting easier elimination. They are used on a shortterm basis to relieve constipation. A stool softener is usually taken before bedtime, with the anticipated result occurring in the morning. They work best if the person drinks a lot of water. Side effects are uncommon, but include stomach cramps. Antidiarrheal Agents o Stool Thickeners (Kaplin, Pectin) Prolonged use will be dangerous, as the bacteria that are inhibited by stool thickeners are also necessary for normal digestion. Thus, they should not be taken for more than 2 days. o Bulking Drugs Bulking agents thicken the stool. They tend to be made of natural fibers from seed that form a gelatin when inside the GI tract. Bulking agents are just high doses of fiber, which you would normally get in the diet, so they are relatively safe, even for children. Metamucil is a common example of a bulking agent. o Anti-Spasmodic Drug (Imodium) They are thought to produce a local effect directly on the gut wall. By slowing down the speed at which the bowel travels through the intestines, more water can be absorbed from the stool producing fewer and firmer stools. These medications should not be taken for more than 3 days and should relieve all diarrhea by that time. These drugs should not be given to children. Side effects include nausea, abdominal pain and distention, dry mouth, constipation, drowsiness, fatigue and dizziness. Module 7: Musculoskeletal Pharmacology Analgesics – pain relief o Opioids Provided euphoria and depress respiration (rate) Enkephalins and endorphins also bind to opiate receptors Opioid peptides are widely distributed throughout the CNS and GI tract Synthesized and stored in neurons Tolerance = effectiveness of drug decreases overtime if taken for an extended period of time Classic problem when taking opioids Develops in first dose with opioids but is not clinical until after 2-3 weeks Cross-tolerance – May develop tolerance to other opoids even if you are taking a different one Theories: o Down-regulation (less receptors) – need to take more drug for the same effect (should switch to a different drug instead of increase the amount taken of the current drug) Physical dependence = will have withdrawal syndrome if they suddenly stop taking the drug (lacrimation, rhinorrhea, yawning, sweating, gooseflesh, chills, diarrhea, nausea) Accompanies tolerance As early as 8 hours after last dose and may last 7 days Short-acting opiates have more severe withdrawal syndrome Hypothesis: opioids inhibit release of some neurotransmitters and thus receptors for these neurotransmitters are up-regulated (more receptors). If opiates are discontinued then normal neurotransmitter release will occur with more receptors present and thus more binding to those receptors. This leads to negative effects and withdrawal syndrome o Have tried blocking neurotransmitters to reduce symptoms o Non-Steroidal Anti-Inflammatory Drugs (NSAID) Anti-inflammatory, anti-pyretic (reduces temp), analgesic, anti-coagulating (decreases blood clotting) o COX-2 Inhibitors COX = cycloxygenase enzyme Subclass of NSAID These drugs are only specific to the COX-2 subtype of the enzyme so don’t block action of the entire enzyme Pain relief o Local Anesthetics Can block MS pain although site of action is not the muscles Block Na+ channel and thus action potentials of neurons If sensory neuron block this results in pain relief Applications include: topical (skin), transdermal (IOP – electrical potential across skin), infiltration (injection into selected tissue), peripheral nerve block (injection close to nerve trunk), central neural blockade (injection within membranes surrounding SC) Analgesics can be given for long period of time and are for broader level of pain but anesthetics are given for sensation block in a specific area Anti-Inflammatory Drugs o Solely bock inflammation o Corticosteroids o o o o o o Skeletal Muscle Relaxants Spasticity = increased tone due to exaggerated muscle stretch reflexes Muscle spasm = increased tone usually after skeletal muscle injury Goal = decrease tone without decreasing function Helpful if injury is in muscle or nerve Baclofen Barbiturates Low TI May directly inhibit transmitter release from presynaptic terminals (independent of GABA effect) and may have antagonistic effect on postsynaptic receptors Benzodiazepines Enhance effect of GABA but do not replace the effect Safer than barbiturates but still cause tolerance and physical dependence Diazepam (Valium) Dantrolene Botunlinum Toxin (Botox) Module 8: Endocrine Pharmacology Based around hormones – exogenous hormones given as drugs if endogenous deficiency is present Adrenocorticosteroids o Glucocorticoids o Mineralcorticoids Thyroid Pharmacology o A lot of innervations from SNS o Synthesizes thyroxin (T4) and tri-iodothyronin (T3) o TSH from anterior pituitary stimulations T3 and T4 production o T3 and T4 provide negative feedback for their own production (like glucocorticoids) o Physiological effects: temperature regulation (increase heat production by increasing BMR), growth and development (stimulate GH release), CV effects (increase HR and contractility), metabolic effets (enhances lipolysis and increase response of fat cells to other liplytic hormones) o Long-term administration of thyroid hormones for hypothyroidism may lead to overdosage if the correct dosage is not used Parathyroid Gland o Produces PTH o Most important job = control Ca2+ concentrations o Released when plasma Ca2+ levels decrease o Raises blood Ca2+ level by affecting bone, kidneys, and GI o When levels increase PTH stops being released (negative feedback) o Increase PTH = bone breakdown; decrease PTH = bone synthesis and remodeling o Vit D increases serum Ca2+ and phosphate levels o Calcitonin Pancreatic Hormones o Pancreas = endocrine (insulin and glucagon regulation) and exocrine (digestive enzymes through pancreatic duct) gland; primarily responsible for glucose control! o DM = due to insufficient insulin secretion (Type I – beta cell function loss) or decrease in peripheral effects (Type II – lack of insulin sensitivity) o Action of drugs for DM Improved glycemic control – focuses on the hormone GLP-1 which stimulated insulin production Reduce insulin resistance in type 2 diabetes – target skeletal muscles Lower CV risk factors of both types of DM Treat peripheral neuropathy o Hypoglycemia Initial symptoms = headache, fatigue, hunger, tachycardia, sweating, anxiety, confusion Severe symptoms = loss of consciousness, convulsions, death o Oral Hypoglycemic Drugs Module 9: Pulmonary Pharmacology Goals of these drugs: bronchodilation, facilitate removal of secretion from lungs, improve alveolar ventilation or oxygenation, optimize breathing pattern Pulmonary Physiology o Airway obstruction occurs with asthma, chronic bronchitis, lung infections, CA, or emphysema Some charachteristics = bronchospasms, mucous in airways, airway inflammation Asthma = imbalance of ANS, PNS is predominant, increased bronchomotor tone leading to narrow airways o Bronchodilators = most common treatment o Bronchoconstriction can be caused by inflammation, abnormal bronchomotor tone, mechanical obstruction (ex: mucous) o Smooth muscle in airways have adrenergic beta-2 receptors that cause smooth muscle relaxation Receptors activated adenylcyclase which produces AMO which causes the relaxation and inhibits degranulation of mast cells using a G protein (amplifies the downstream action) Myosin is phosphorylated and inhibited from interacting with actin thus the muscle relaxes Asthma o Inflammed airways o Airways overly sensitive which leads to allergic reactions and narrowing o Main symptoms = wheezing, coughing, tightening in chest, trouble breathing (esp. night and early morning) o Goal with drugs = reduce frequency and severity of attacks o Attacks and triggers unique to individual o Quick acting drugs: take at first sign of asthma attack, relieve symptoms within minutes o Long acting drugs: taken daily, long-term control of attacks to help decrease frequency o Bronchodilators For asthma, COPD, infections Inhalers Prime by spraying in air twice Breath out slowly to the end of a normal breath Spray so it does not hit roof of mouth or tongue Breath in slowly Allows drug to be administered directly to the lungs and allows higher dosage to reach lungs Few side effects o Glucocorticoids o Methylxanthine o Mediator-release inhibitors Allergies o Caused by overactive immune system o No cure o During allergy attack histamine is released from mast cells causing local inflammation and swelling followed by leakage on the wall o Antihistamines o Decongestants o Corticosteroids – decrease inflammation, need to be taken daily to have an effect o Bronchodilators – o Leukotriene blockers o Mediator release inhibitors o Immunotherapy – allergy shots – gradually increase level of allergen to prevent allergy attacks Other Obstructive Lung Diseases o Expectorant o Mucolytics o Antitussives Module 10: Oncological Pharmacology Chemotherapy = chemical given as therapy o Goal is to selectively kill the cancerous cells while leaving the healthy cells intact o Currently not overly specific o Severe side effects Common side effects include: Myelosuppression (bone marrow depression) – decreased production of all blood components; low WBC and susceptible to infections; know pt’s blood count and wash hands; take proper precautions if you are sick; may have increased pulse and RR if anemic Cardiac toxicity – Adriamycin or daunomycin ay cause irreversible cardiac damage; check vitals frequently, monitor for SOB, chest pain and increased pulse with little activity Pulmonary fibrosis – Bleomycin, methotrexate, or cisplatin may cause this and result in restrictive lung disease Peripheral neuropathy – Vincrisine can cause weakness and paresthesias distally, tumor invasion can cause neuropathy, weakness such as foot drop should subside after chemo treatment Fibrosis – hard edema and fribrotic tissue that can limit joint movement, AROM ex to prevent contractures GI toxicity – nausea, vomiting, diarrhea, and ulcerations of mucosal lining can occur Alopecia (hair loss) – temporary side effect of certain drugs, re-growth may begin during or after all chemotherapy Oncological drugs = drugs to treat cancer Tyrosine kinase receptor is important in transformation of normal cells to cancerous cells o Phosphorylate other intracellular proteins when activated o Receptor normally involved in the cellular growth and division, but when altered somehow it can induce cancerous changes in the cell Module 11: Immunological Pharmacology Usually inhibit bacterial or fungal cell wall synthesis, leaving organism with damaged outer membrane May target ribosome’s involved in protein synthesis or enzymes involved in DNA replication Overuse and inappropriate use has led to drug resistance organisms Antibacterial Agents o Penicillin Penicillins are the most widely prescribed and effective classes of antibiotics. They are used to treat gram positive bacteria including streptococci, meningococci, enterococci, o Vancomycin o o o o Vancomycin resistance has become a major clinical problem in recent years. Vancomycin-resistant enterococi are frequently resistant to all other antibiotics, leaving no pharmacological tool for treating the infections. These resistant bacteria are clear examples of Darwin's natural selection at work. Tetracyclines They inhibit gram-positive and negative bacteria, including chlamydiae, mycoplasmas, rickettsiae, and some protozoa and amebas. These drugs are no longer prescribed for gonococcal disease, because of wide-spread resistance to them. Active against both gram negative and gram positive organisms. Chloramphenicol It is taken orally, and is taken up by cells quickly. It is a fairly toxic drug so its is prescribed sparingly for serious rickettsial infections, such as typhus and Rocky Mountain spotted fever. It can cause GI problems with diarrhea and vomiting. It is toxic for infants with the drug accumulating resulting in the "gray baby syndrome" in which the baby actually takes on a gray color and is accompanied with vomiting, flaccidity and shock. Sulfonamides Sulfonamides are given to treat bacterial infections and are also used for diabetes mellitus, and edema and gout. These drugs inhibit bacterial folic acid synthesis Isoniozid Isoniozid drugs are the first line of defense to treat active tuberculosis in combination with other agents. Antiviral Agents o These drugs have been most important in the intervention for HIV. o Acyclovir Is used to treat herpes simplex virus and vericell-zoster virus o AZT Azidothymidine, also known as AZT or Zidovudine, was one of the first drugs designed to fight HIV infections. o Indinavir Indinavir is an inhibitor of a protease specific to HIV-1. It is typically given to HIV positive patients in combination with reverse transcriptase inhibitors. Combination of the two is more effective and greatly reduces the risk of the virus mutating to become resistant to one line of drug. o Interferons Interferons are endogenous proteins that are inserted into the membrane of a cell after viral infection. This blocks subsequent viral infection by other particles. By artificially giving interferon to a person, it inserts itself into the membrane and fools the invading virus leaving the impression that the cell has already been infected. Antifungal Agents o Amphotercin Amphotericin attacks the unique lipids in fungi compromising the stability of the fungus. It can be taken orally, topically and by IV. o Azoles These drugs are particularly important in fighting fungal infections on a systemic level or topically They may cause minor GI problems but side effects are few and minor