SOP Title - NIHR Clinical Research Network
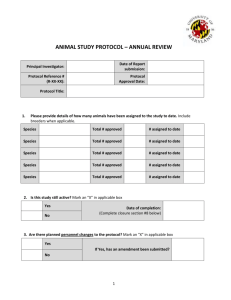
advertisement

Work Instruction Title: Serious Adverse Event Reporting Work Instruction Number: 21 Version Number: V2 Effective Date: 19 January 2011 Author Name: Heather Leishman Title: PCRN-EoE Network Co-ordinator Date: 17 February 2010 Approved by Name: Helen Macdonald Title: Research Delivery Manager Date: 8 October 2014 Review date: 8 October 2016 Review History Version No. date V1 01.07.2013 V2 24.09.14 amendments Minor change: Removal of PCT reference Change from 24 hour reporting to immediate reporting plus minor amendments HL WI 21 Serious Adverse Event Reporting Page 1 of 8 Approved V2 1. Introduction, Background and Purpose Pharmacovigilance is the continuous process of monitoring, evaluating and improving the safety of medicines, which is ongoing throughout the period of drug development, from animal testing through to post-marketing surveys. In order to assess the safety of an investigational product, and protect trial participants, it is important to: Collect baseline information on the health status of trial participants Be aware of and record all concomitant medications Ask about these, and about the subjects health status at every visit Record all untoward medical occurrences (Adverse Events, (AEs)) as specified in the protocol and report within the specified timeframes Collect all data as accurately as possible A Serious Adverse Event (SAE) is any untoward medical occurrence or effect that at any dose: results in death is life threatening requires hospitalisation or prolongation of existing inpatients’ hospitalisation results in persistent or significant disability or incapacity is a congenital abnormality or birth defect In this context, life threatening refers to an event in which the subject was at risk of death at the time of the event; it does not refer to an event which hypothetically might have caused death if it were more severe. Medical judgement should be exercised in deciding whether an adverse event/reaction is serious in other situations. Important adverse events/reactions that are not immediately life threatening or do not result in death or hospitalisation but may jeopardise the subject or may require intervention to prevent one of the other outcomes listed in the definition above, should also be considered serious. When a Serious Adverse Event is judged by the Principal Investigator or Sponsor as having a reasonable causal relationship to the investigational product, at any administered dose, it is considered to be a Serious Adverse Reaction (SAR) by the sponsor Should a study participant become pregnant whilst participating in an a Clinical Trial of an investigational medicinal product (CTIMP) or aids in the conception of a child whilst participating such a trial, the pregnancy and resulting child should be followed up for a period of no less than 18 months to verify whether a congenital anomaly or birth defect is present. Severity The term “severe” is often used to describe the intensity of a specific event. This is not the same as “serious” which is based on patient/event outcome or action criteria. A Serious Adverse Reaction (SAR) is any adverse event/reaction that is classed as serious and which is consistent with the information about the investigational medicinal product (IMP) listed in the Summary of Product Characteristics (SPC) or Investigator’s Brochure (IB) Suspected Unexpected Serious Adverse Reaction (SUSAR): Any adverse reaction that is classed as serious and is suspected to be caused by the IMP that is WI 21 Serious Adverse Event Reporting Page 2 of 8 Approved V2 NOT consistent with the information about the IMP in either the SPC or IB. The Sponsor reports SUSARS to the MHRA and also to the research ethics committee and drug safety committee who continually assess the safety of an IMP and the continuation of the trial. Each SAE should be checked for expectedness. The event should be considered a SUSAR if: it is not listed as expected, or it has occurred in a more serious form than anticipated, or the outcome is not consistent with the applicable product information. 2. Abbreviations See Reference Document: CRN Glossary of Terms and Abbreviations 3. Scope The Work Instruction (WI) applies to all staff working on NIHR adopted interventional studies. A clinical trial of an investigational medicinal product (CTIMP) is a legal definition and describes those trials which fall within the scope of the Medicines for Human Use (Clinical Trials) Regulations 2004, and subsequent amendments Non CTIMP trials, while not governed by law, are governed by the DH Research Governance Framework for Health and Social Care (2005), all studies therefore require an awareness of safety reporting requirements. This WI should be read and applied in conjunction with relevant Trust Policies and approved study protocols. 4. Responsibilities The Principal Investigator has responsibility to ensure that a system is in place to ensure accurate and timely reporting of SAEs. The PI may delegate the task of initial reporting to a delegated team member as set out in the Authorised Delegation Log (ADL). When the study team become aware of an SAE it must be reported to the study sponsor immediately. Each Adverse Event must be evaluated for seriousness, causality and expectedness. The responsibility for this evaluation can be shared between the Chief Investigator and the Principal Investigator. The study protocol should state who has responsibility for the assessment and reporting. The sponsor will also assess causality and expectedness and may decide to upgrade an Investigator decision, but may not downgrade the Investigator’s assessment of any adverse event. 5. Procedures 5.1 Planning General Practice team/service team should consider carefully how best to capture the SAEs in a timely manner when a study is accepted, particularly if there are long time periods between study visits. It is important that the PI and the study nurse/co-worker make time to examine the reporting procedures in the study protocol carefully, ensuring they have a good supply of reporting forms, patient emergency contact cards and study diaries (where applicable) before the study starts recruiting. Easy access to the Investigator’ Brochure (IB), if the product is not yet marketed, is essential for reference purposes throughout the period of the trial when patients are seen for study visits. WI 21 Serious Adverse Event Reporting Page 3 of 8 Approved V2 For initial reporting procedures to work well both the study participant and the practice/service need to be organised and ready for such events. 5.2 The Investigator’s Brochure The investigator’s brochure (if applicable) will be updated throughout a clinical trial (at least yearly). As new information emerges about the study drug/product, this information should be made known to the Principal Investigators - usually through an updated Investigator’s Brochure and regular communications from the sponsor This includes reports of SUSARs at other sites, and also SUSAR reports from other trials in which the IMP is being administered. These notifications should be filed in the Site File. 5.3 SAE / SUSAR reporting from the participant One way of ensuring good and timely reporting from the participant is to explain the reporting procedures for serious adverse events to the participant at the informed consent visit. The participant should then understand that they need to let the site study team know if they become very unwell. Ask the participant to give the PI’s contact details to a family member or friend who can make contact if anything untoward occurs so that it can be reported. The ‘Emergency contact card’ (see Appendix 1) should also be discussed with the participant at the informed consent visit although this may not be given to the participant until the randomisation visit. 5.4 Note alerts In general practice/service it is strongly recommended that the practice applies a tag or alert to the electronic clinical records of participants who have consented to take part in an interventional research project. In line with SOP 01 Informed Consent, this assists locum staff at the practice/service by providing the Participant information sheet and GP/Dr information sheet for the relevant study. By working with administration staff to ensure all tagged/alerted study participant incoming letters/discharge letters are passed to the PI or study nurse, adverse event reporting is likely to occur in a timely way. 5.5 SAE/ SUSAR reporting Serious Adverse Events should be reported in line with the study protocol. The study nurse/co-worker or PI completes the initial SAE report form. This will be supplied by the study team with clear guidance on where and to whom it should be sent, See Appendix 2. Only delegated study staff can complete the SAE form. This report should be sent immediately upon knowing about an event, including all information that is available at the time. It is better to ‘over report’ than not to report. The PI must sign the SAE form, but the initial form can be sent without the PI signature if the obtaining a signature may cause delay in reporting. In this case the form needs to be re-sent once it has been signed by the PI. Once the initial, signed SAE form has been sent to the study sponsor (usually the data monitoring team), a photocopy of the form together with a cover letter giving the full name of the study and the name of the Chief Investigator may need to be sent to the research ethics committee that approved the study and the research governance body that approved the study for the site. The practice/service team will need to check local requirements for this. In many cases the sponsor will assist with this unless this has been delegated to the site team (PI and study nurse). The SAE form may be either paper or electronic (e-CRF). SAE forms do not have participant identifiable data on them but are recognised by the study WI 21 Serious Adverse Event Reporting Page 4 of 8 Approved V2 number only. If an SAE form is completed for a participant and sent to the Sponsor and approval bodies (as described) this should be marked in the participant’s clinical record. 5.6 Fax procedures In order to submit the SAE form within 24 hours of the study team learning about the event it is usual to send the form by fax. If an administrator is faxing the form they must understand the importance of receiving confirmation that the fax has been received by the sponsor. Faxes must be sent following the secure fax reporting procedure as set out in the local Information Governance policy. Otherwise the following procedure should be used. First telephone the sponsor as set out in the site file to inform them of the report. Send the SAE form using a fax cover sheet with the practice/service details, number of pages, the fax number of the sponsor and the date. State the study number of the participant and the date of the SAE. Where possible attach the fax receipt with the fax cover sheet to the back of the SAE form that has been sent. Ensure that the fax receipt shows that the fax was sent. In some large trials the fax machine may often be busy and your fax may not get through - in this case the fax receipt shows as “busy”. In this case you must contact the team again and arrange to send the fax later. Once the fax has been sent, contact the study team to ensure that it has been received and note this on the SAE form. File the SAE from and fax related paperwork in the study site file under SAEs. 5.7 Follow up SAE reports The study protocol should stipulate when follow up SAE forms are required. The follow up forms are usually the same as the initial reporting forms, but should be identified as Follow Up. In the follow up period more available data will sent to the sponsor such as X-ray reports/scans/discharge letters. It is possible that a diagnosis may also have been made if this did not occurred initially (the initial report may read “patient collapsed - unknown cause”). The above procedures apply to the follow up forms except that the PI may now be asked on the form to give an opinion about the likely causality and expectedness of the event (i.e. does the PI think that the event was caused by the study drug?). All source data sent with follow up SAE forms as evidence of an event must be anonymised and the patients study number applied to the documentation. 5.8 Protocol deviation (1) ‘The sponsor and investigator may take appropriate urgent safety measures in order to protect the subjects of a clinical trial against immediate hazard to their health or safety’ (2) ‘If measures are taken pursuant to paragraph (1) the sponsor shall immediately, in any event not later than 3 days from the date the measures were taken, give written notice to the licensing authority and the relevant ethics committee of the measures taken and the circumstances giving rise to those measures’ SI 2004/1031 Medicines for Human Use (Clinical trials_ regulations 2004: Part 4, Section 30) 5.9 Incident reporting If the PI is of the opinion that the event was caused by the study drug (even if this has not been proven), the PI should contact the local RM&G department to WI 21 Serious Adverse Event Reporting Page 5 of 8 Approved V2 discuss whether the event should be reported under local incident reporting procedures. 5.11 Audit During an audit or inspection the SAE reporting procedures will be examined along with each adverse event report that has been reported and filed. It is good practice therefore to ensure that the events in the site file are properly grouped by study participant and followed up appropriately. Evidence that the SAE reports and follow up reports were sent to the Research Ethics and Research Governance organisations will be examined. See WI 16 Audit and Inspection. 6. Related SOPs, Work Instructions and Reference Documents 6.1 SOPs SOP 01 Informed Consent SOP 05 Safety Reporting 6.2 Work Instructions WI 16 Audit and Inspection WI 20 Adverse Event reporting 6.3 Reference Documents ICH Good Clinical Practice (GCP) EU Clinical Trials Directive (EUCTD) CRN Glossary of terms and Abbreviations 7. Appendices Appendix 1: Example of wording on Emergency Contact Card: Appendix 2: Example of SAE Reporting Form WI 21 Serious Adverse Event Reporting Page 6 of 8 Approved V2 Appendix 1: Example of wording on Emergency Contact Card: Patient Name: …………………… Patient Number:………………….. GP Name:………………………………. GP Number………………………….. WARNING This patient is taking part in a clinical trial, and may be on xxx (name of drug) To discuss obtaining a code-break, treating doctors should contact: Tel no: xxx (needs to be 24/7) WI 21 Serious Adverse Event Reporting Page 7 of 8 Approved V2 Appendix 2: Example of Serious Adverse Event Reporting Form SERIOUS ADVERSE EVENT FORM Date of Report Study Name Patient ID Centre Type of Report: 1. Patient initials (first, last) Initial 1a Country Date: / / Final Month Date : / / EVENT INFORMATION 2a. Age 3. Sex 4-6. Reaction Onset Years Day Month Year 2. Date of Birth Day Year Patient died Hospitalisation or prolonged inpatient hospitalisation Involved persistence or significant disability or incapacity Life threatening Congenital Anomaly/Birth defect Medical intervention to prevent the above 7-13. Summary of Event (include severity level (1=mild, 2=moderate, 3=severe,4=life threatening) Date event became serious _____/_____/_____ End date of event 8-12. Check all appropriate to adverse reaction _____/_____/_____ (If ongoing please complete follow form STUDY DRUG INFORMATION 14. Study Drug(s) (include generic name) 20. Did reaction abate after stopping drug? Yes 15. Daily Dose(s) 16. Route(s) of Administration No N/A 21. Did reaction reappear after reintroduction? Yes 17. Indication(s) for Use 18. Therapy Dates (from/to) No 19. Therapy Duration CAUSALITY OF OVERALL DIAGNOSIS TO STUDY DRUG 1. Almost certainly related 2. Probably related 3. Possibly related 4. Unlikely to be related 5. Unrelated CONCOMITANT DRUG(S) AND HISTORY 22. CONCOMITANT DRUG(S) AND DATES OF ADMINISTRATION (exclude those used to treat reaction 23. OTHER RELEVANT HISTORY (e.g. diagnostics, allergies, pregnancy with last month of period, etc) Batch No. of Study Drug Administered Form completed by: Signature of Doctor: Reporting GP: Contact No. Position (PI): PLEASE RETURN TO: CLINICAL TRIALS UNIT FAX NO: WI 21 Serious Adverse Event Reporting Page 8 of 8 Approved V2 N/A