DEATH
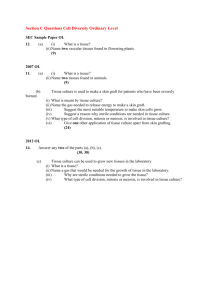
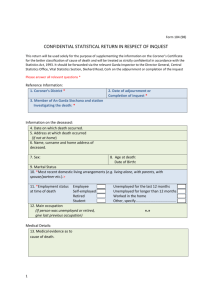
advertisement

DEATH CESSATION OF LIFE IN A PREVIOUSLY VIABLE ORGANISM A DOCTOR must declare DEATH SOMATIC DEATH The failure of the body as an integrated system associated with loss of – circulation respiration and innervation For such a period of time that, under the specific circumstances, it is impossible for life to return Irreversible unconsciousness MOLECULAR DEATH Different tissues/organs die at different rates Depends on susceptibility to oxygen deprivation Connective tissues less vulnerable Skin remain viable for several days Muscles respond to stimuli for hours WBCs motile for 12hours Cortical neurones die after 3-7mins BRAIN DEATH Cortical brain death Deep coma + functioning Brain Stem PERSISTANT VEGETATIVE STATE Brain stem damage Failure of the respiratory motor system Cannot breath unassisted Damage to ascending reticular activating systems Loss of consciousness Cortical brain death + brain stem damage WHOLE BRAIN DEATH Artificial ventilation keeps the ‘corpse’ alive Prevents heart from failing, until ventilation withdrawn The ‘beating heart cadaver’ Persistent vegetative state Functioning brain stem but non functioning higher centres, do not require permanent assisted ventilation, since introduction of modern artificial ventilation techniques, heart protected from hypoxic damage and survives may live for years as long as fed, often directly into stomach. May die if withhold nutrition. Ethical dilema Require Court Order, otherwise Dr. may be held responsible for the death. One successful case in Ireland Brain stem death tests 1. Absent pupillary response to light 2. Absent corneal reflex 3. No motor response within the cranial nerve distribution to adequate nerve stimulation of either trigeminal areas or limbs 4. Absent gag reflex or response to tracheal or bronchial stimulation 5. No oculo-cephalic (Doll’s eye phenomenon) 6. No vestibulo-ocular reflexes (cold-water on tympanic membrane) 7. Demonstration of persistent apnoea: a.Normal blood gases while on ventilator b.Disconnect ventilator c.Deliver oxygen into trachea @ 6L/min d.Check blood gases after 10mins. If CO2 has risen to 55mmHg and no effort is made to breathe, the test is positive and apnoea is present. ORGAN DONATION Living donor – if possibly successful and not detrimental to the donor blood, bone marrow, paired organs e.g.kidneys, part of liver(regeneration within weeks) minors!!!, ethical considerations Cadaveric donor – Legal rules vary from country to country, Human Tissue Act UK and NI 1.Death due to natural causes – consent – a. deceased carried a donor card (some countries absolute right, opt in or out of schemes), next of kin no objection b. if not, from next of kin, if deceased not known to have objected in life c. if no next of kin, hospital authority 2.Death not due to natural causes consent – as above, but Coroner (or equivalent) must be informed, he or she will make decision Consent must be written Postmortem examination will be performed to exclude systemic infection or disease Where possible, blood will be tested beforehand to exclude viral infections Donor excluded if over 75years, malignant disease except brain tumour, major systematic sepsis, Hep B or HIV positive DONOR ORGANS CORNEA Enucleation can be carried out up to 24hours after death Does not have to come from brain stem dead patient on life support No age limit for donor KIDNEY 85% successful in first year LIVER For congenital malformations, end stage chronic liver disease, fulminant hepatic failure, inborn errors of metabolism and primary carcinomas 75% success rate in adults and 85% in children in first year HEART Survival rate 80% in first year HEART/LUNG Lung disease secondary to heart disease or end stage primary lung disease 75% success in first year HEART VALVES May be removed up to 72hours after death PANCREAS +/- KIDNEY in diabetics graft survival rate 45% in first year DEATH CERTIFICATION Births and Deaths Registration Act (Ireland) 1880 Medical Certificate of the Cause of Death ‘ No medical practitioner should give a medical certificate of the cause of death unless he has been personally in attendance upon the deceased during the last illness and no other person or practitioner may sign the certificate on his behalf ’ ‘A registered medical practitioner who was in attendance upon the deceased during his or her last illness is required to give a medical certificate on the prescribed form in every case’ DEATH CERTIFICATION Section 18 (4) of the CoronersAct, 1962 ‘Every medical practitioner, registrar of deaths or funeral undertaker and every occupier of a house or mobile dwelling, and every person in charge of any institution or premises, in which a deceased person was residing at the time of his death who has reason to believe that the deceased person died, either directly or indirectly, as a result of violence or misadventure or by unfair means, or as a result of negligence or misconduct or malpractice on the part of others, or from any cause other than natural illness or disease for which he had been see and treated by a registered medical practitioner within one month before his death, or in such circumstances as may require investigation (including death as a result of the administration of an anaesthetic) shall immediately notify the Coroner within whose district the body of the deceased person is lying of the facts and the circumstances relating to the death’ DEATH CERTIFICATION G.P. or Hospital doctor Before issuing a death certificate think 1. Am I satisfied regarding not only the mode but also the underlying cause of death? 2. Does the death fall into any of the categories which require reporting to the Coroner (or equivalent)? 3. Is a postmortem dissection desirable for any reason? 4. Has the family any complaint about the medical care preceding death? If in doubt call the Coroner CHANGES AFTER DEATH Immediate signs of death Cardio-respiratory failure Absent heart beat, no pulse No chest movement, no breath sounds Pupils do not react to light Retinal vessels show ‘trucking’ Loss of corneal reflexes Muscle flaccidity Check for pulse, listen with stethoscope for 4 to 5 minutes, and continue resuscitation until sure the person is clinically dead, especially in cases of electrocution and bodies removed from water. Initially body feels warm and the limbs are flaccid (primary). Early postmortem changes Rigor mortis Chemical reaction in muscle due to breakdown of ATP, and increase in ADP, lactates and phosphates. Anoxia causes anaerobic glycolysis resulting in an increase in pyruvic and lactic acids. The muscle glycogen decreases, the pH drops, ATP drops affecting the linkages between actin and myosin. Temperature dependent, more rapid onset in high temperatures, after exercise or if fever i.e. if the muscle glycogen levels are already low. Therefore more rapid onset in children elderly and in wasting diseases. Delayed in asphyxial deaths and if severe haemorrhage. Muscles not shortened. Starts 1 – 4 hours in face Limbs stiffen 4 – 6 hours, small muscles of jaw and arms first Maximal 6 – 12 hours Secondary flaccidity within 24 – 50 hours May be instantaneous, cadaveric spasm or rigidity, in violent deaths, drownings. Hypostasis / lividity/livor mortis Gravitational pooling of blood in veins and capillary beds. Begins immediately as blood is liquid due to fibrinolysis. Patchy within 20-30mins Visible in 2 – 3 hours, gravitational – blanching – contact pallor where body in contact with surface, floor or bed or even clothing. Fixed after several hours (10-12hrs). More useful in determining if body position altered within few hours after death, than in determining the time of death. Even if body moved within 24hrs may be obvious change of pattern Bronze – Cl. Perfringens Pink – carbon monoxide poisoning, Cold e.g. body in water, hypothermia, Refrigeration Deeper pink – cyanide poisoning Chocolate brown – methaemoglobin in potassium chlorate, nitrate or aniline poisoning. DD. bruise – incise tissues as blood in vessels if hypostasis but blood in tissues if bruise. However may be rupture of small vessels in the legs in dependent lividity in hanging. Cooling of the body/Algor mortis Occurs in cool and temperate climates. Not immediate, onset when cell death occurs, body temperature will then begin to drop from 37degreesC. Remember temperature at time of death may be less than 37degreesC if hypothermic, in deaths in congestive cardiac failure, haemorrhage or shock, or greater than 37C in deaths due to asphyxia, other causes of hyperpyrexia e.g. intra cerebral haemorrhage, heat stroke or infections. After slow start due to a temperature plateau when the body temperature is maintained for anything up to 3hrs, there is a rapid drop, followed by more gradual decrease when the body is nearing the ambient/environmental temperature. Body feels cold after about 12hours. More rapid in cold temperatures, if wet or in water(2or3x), if thin (surface area>weight), if naked.(lower trunk) or if air movement. Take internal/rectal temperature with low reading thermometer, not a clinical thermometer. Newton’s Law of Cooling – rate of cooling is proportional to the difference in temperature between the body and its surroundings - Exponential graph. Henssge’s Normogram. Unknowns – temperature at time of death, length of plateau. Late postmortem changes Decomposition – due to initial chemical/enzyme reaction, autolysis, followed by bacteria, fungi, insects and animal activity. Putrefaction Liquefaction of the tissues. Change in colour, evolution of gases and liquefaction. More rapid if infection, high temperatures, summer. First presents as green discoloration of the skin of the anterior abdominal wall 36 to 72hrs after death, due to intestinal bacteria. Conditions favour growth of anaerobic organisms eg Cl. Welchii. Followed by gaseous distention of the abdominal cavity and the soft tissues, marbling of the skin, due to haemolysis in the vessels, and formation of fluid filled blisters – skin slippage. Face and eyelids swollen, face discoloured and crepitant, nails and hair become loose. Gas formation causes bloody fluid from the decomposing lungs to be purged from the nose and mouth but also the vagina and rectum. Generalised swelling, abdominal distension. Continues until tissues all liquefy and body skeletalised, within weeks to years, depending on the local conditions. Accelerated in hot conditions and if ‘attacked’ by flies and other predators. Also if obese, oedematous or have injury which is infected. Retarded if body immersed in water or buried. Body smells due to gases (H. Sulphide, methane, ammonia) and mercaptans. Commences in intestines, stomach, liver blood, heart blood and blood in vessels, thereafter air passages, lung and liver (honeycomb), spleen soft Followed by brain and cord, Kidneys, bladder and testis Voluntary muscles and lastly uterus and prostate. Modified changes Mummification Dessication/dehydration or drying of the soft tissues. Occurs in dry conditions, especially if there are air currents. Prevents bacterial decomposition and therefore putrefaction. May only be partial e.g. fingertips or face. Skin and soft tissues leathery and hardened. Occurs in stillbirths and deaths of newborns as bodies sterile. Adipocere Saponification or hydrolysis of the body fats, chemical change. Hydrogenation of Oleic acid to opaque Stearic acid. Acids inhibit bacteria. Occurs in damp or wet conditions e.g. bodies in water or buried in wet ground after many weeks. Causes stiffening and swelling of body fats and preserves the body fats which remain adherent to bones after the skin has rotted away. Therefore the shape and outline of the body is retained for years. Skeletalisation Loss of soft tissues over a period of time (see previous). Tendons, ligaments, uterus, prostate hair and nails survive longest. Bones disarticulate after a few years. At first bones heavy, surface greasy, marrow in cavities and bones smell. After 40-50 years bones dry and brittle and may erode. Depends on local environment. If bones older than 70years of archaeological rather than forensic interest. Carbon dating useful only in ancient archaeological remains. For recent bones can use other markers. Maceration Aseptic autolysis of foetus. Dead in utero for several days. After delivery there are rapid changes due to secondary bacterial overgrowth. Entomology The use of insects as an indicator of the time since death. Inthis country Necrophagous species are the first wave of succession, including blue and green bottles and flesh flies. Depends on temperature. Blow flies willnot lay eggs in temperatures less than 6degreesC and do not lay eggs at night. Eggs layed within 24hours of death. Develop into 1st. instar maggots within 24hours, 2nd. Instar within the next 24hours and to 3rd. instar stage within the next 24 – 36hours. These develop into pupae and eventually into the fly. Burial Rate of body decomposition depends on the depth, type of soil, drainage and coffin. Well drained – skeletonised in about 10years. Child takes about 5years. 1 week in air = 2 weeks in water = 8 months of burial. Rule of thumb Warm and flaccid – dead few hours Warm and rigid – dead 2-9hours Cold and rigid – dead more than 9hours.