Medical Education Ann. Report
advertisement

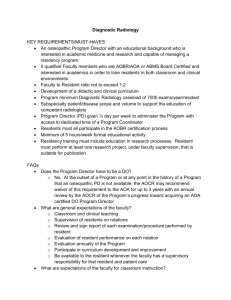
Mount Auburn Hospital Medical Education Annual Report June 28, 2011 Charles J. Hatem, MD Director of Medical Education/Designated Institutional Official Accreditation Council for Graduate Medical Education Institutional Organization and Responsibilities (Section I.B.4.b) “The Designated Institutional Official (DIO)… must present an annual report to the Organized Medical Staff…and the governing body of the Sponsoring Institution…This annual report will review the activities of the Graduate Medical Education Committee (GMEC) during the past year with attention to, at a minimum, resident supervision, resident responsibilities, resident evaluation, compliance with duty-hour standards, and resident participation in patient safety and quality of care education.” The Graduate Medical Education Committee (at Mt. Auburn the GMEC= the Medical Staff Education Committee/members listed in Appendix 1) meets monthly to review the spectrum of medical education issues within Mt. Auburn Hospital. Typically, issues pertaining to undergraduate, graduate and continuing medical education are discussed, but this report will focus on the training of interns and residents (=housestaff) at MAH. The previous Medical Education Annual Report to the Mt. Auburn Board of Trustees was presented on March 23, 2010. Overview: 1. The Committee is well acquainted with ACGME residency requirements: “Minimum Program Requirements Language Approved by the ACGME, September 28, 1999 Educational Program: The residency program must require its residents to obtain competencies in the 6 areas below to the level expected of a new practitioner. Toward this end, programs must define the specific knowledge, skills, and attitudes required and provide educational experiences as needed in order for their residents to demonstrate: a. Patient Care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health b. Medical Knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care c. Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care d. Interpersonal and Communication Skills that result in effective information exchange and teaming with patients, their families, and other health professionals e. Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population f. Systems-Based Practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value.” 2. Current background information dealing with MAH Graduate Medical Education (GME) follows: There are 68.74 FTE residents who are/will train at MAH this current academic year. These include residents in Medicine, Radiology, Surgery, Emergency Medicine, OB/Gyn, Pediatrics, and Podiatry (A MAH-base Podiatry Residency is slated to begin in the Fall, 2011). Within the Internal Medicine training program there are 50 residents and 2 chief residents, and within the Diagnostic Radiology program there are 13 residents. The Internal Medicine and Diagnostic Radiology Programs are MAH-based residencies for which we are reviewed by separate program and institutional mechanisms on a regular basis. Regarding Accreditation Status by the Resident Review Committees: o Medicine: Program Director/Dr. Eric Flint; Associate Program Directors: Drs. Cherie Noe and Patrick Gordan. effective 5/15/10 – Next site visit – 5/1/15 – Cycle length – 5 years. Last internal review – 8/3/09 – next internal review due – 11/6/12 o Radiology: Program Director/Dr. Pierre Sasson; Associate Program Director: Dr. Edward Marianacci. Effective 4/7/2010 – next site visit 4/1/15 – Cycle length 5 years. o Last internal review – 9/20/07 – next internal review due 10/3/12. 2 Report Details: Resident Supervision Supervision with the MAH graduate training programs is the responsibility of all the faculty who practice within inpatient and outpatient arenas of the institution. The basic process issue within medical education here and elsewhere is the graduated assumption of responsibility, under supervision, as the key element in the development of professional independence. Within the Department of Medicine there is broad matrix of supervision beginning with close assessment by the hierarchy within the resident training program. As well, the MAH hospitalist program as well as the Intensivists/Critical Care physicians provide 24/7 on-site supervision of the housestaff in the provision of care. Similarly, the availability of 24/7 Emergency Medicine Faculty and access to the full complement of subspecialists are essential resources for the care of patients as well as being crucial to our training programs. Programmatically, the Internal Medicine (IM) Residency program meets regularly as the Educational Council , a construct within the Department of Medicine devoted to weekly reviews of the Internal Medicine Residency. This Council is comprised of the Chair of Medicine, Program and Associate Program Directors of the IM Residency, Chair of the Clinical Competence Committee, Head of the MAH Hospitalist Program, Chair of Cardiology, Intensivist/Critical Care physician, Community Primary Care practitioner and the Chief Residents in Medicine. The sole purpose of this Council is the ongoing surveillance of the IM Residency program and assuring that residents are being trained properly and progressing on an individual basis as required. There is also a weekly conference of the Program Director of Internal Medicine and Associate Program Directors along with the Chief Residents in Medicine devoted to a review of housestaff functioning and program operations. Within the Diagnostic Radiology Program there are also substantial efforts directed at the supervision of residents. The key elements of that supervision are: Faculty supervision is available at all sites of training. All radiologic studies performed and interpreted by radiology residents between 7am and 9pm on weekdays and between 6am and 6pm on weekends are checked by a staff radiologist within one hour. All studies performed after hours while the resident is on-duty are checked by the staff radiologist within 14 hours. Residents must have a minimum of 12 months of training in diagnostic radiology prior to independent in-house responsibilities. Faculty back up by phone is immediately available to the night float resident. All faculty have online access to the department PACS (Picture Archiving and Communications System) system from home. On-call faculty are available to come into the hospital, generally within 15 minutes if needed. Faculty call assignments with home phone and pager numbers are available to the 3 residents. Available on-call faculty includes one staff member on-call for general radiology, one on-call for interventional radiology and one on-call for MRI and acute stroke. All percutaneous interventional invasive procedures performed by residents are done so with direct faculty supervision. Resident clinical training provides for progressive, supervised responsibility for patient care. The responsibility or independence given to an individual resident depends on that residents’ skill, experience and knowledge base. Residents begin taking in-house independent call after they have successfully completed 12 months of training in diagnostic radiology and have passed the on-call certification examination. All radiologic images are reviewed and all reports are signed by faculty within 14 hours. Programmatically, within Radiology, the Radiology Education Committee meets quarterly to discuss active residency issues. This Committee is comprised of the Chair of Radiology, Program Director and Assistant Director, Program Coordinator, Administration Representative and all of the Radiology Residents; Additional programmatic oversight is secured by: Quarterly meetings among the Program Directors and the DIO to review challenges and strategies the have evolved within each program that might be applied in a different residency. As noted, there are annual meetings between the Program Director of the Diagnostic Radiology Program and his counterparts at Participating Institutions (Massachusetts General Hospital and Boston Children’s Hospital), and lastly, the Medical Staff Educational Committee monthly meetings reviews the gamut of medical education offerings at the hospital, which includes specific reporting by the Program Directors of the Medical and Radiology Residency programs, as well as input from residents in attendance; Resident Responsibilities The educational objectives for the various training rotations within the Internal Medicine and Diagnostic Radiology Programs are listed on the CareGroup Portal under the heading ‘New Innovations’. This site contains various administrative details pertaining to the housestaff as well as detailed curriculum definitions for the various residency rotations. On line evaluation instruments are here as well as the mechanism for logging duty hours, which will be discussed below. Here the educational responsibilities are well outlined and joined with those clearly articulated at orientation and throughout the year pertaining to pertinent infectious disease recommendations (notably hospital policies on handwashing), confidentiality and record keeping. Issues of responsibilities for self, significant others 4 and patients are reviewed with emphasis at orientation. Annual copies of the document, Compact Between Resident Physicians and Their Teachers, are distributed and further defined the mutual responsibilities between residents and faculty. The Internal Medicine Residency program sponsors a yearly retreat for all medical housestaff. Each of the last 6 annual retreats has been devoted to the exploration of a different ACGME competency domain. These programs are conducted under the sponsorship of the competency committee of the Internal Medicine residency and directly under the leadership of the Chair of the Competency Committee and the Director of Faculty Development at MAH. These programs have utilized a variety of techniques to meet the different educational goals presented by the exposition of each ACGME competency domain. Resident Evaluation As oft said, assessment drives the system, and a variety of approaches are used for the evaluation of housestaff at MAH. After monthly rotations in the IM residency, input by faculty about the housestaff along with input by the housestaff about the faculty are reviewed by the Program Director. Housestaff receive as copy of their evaluations as does their faculty advisor (assigned to all IM housestaff and with whom they meet every 3 months.) Housestaff performance is monitored regularly throughout the year in weekly meetings of Drs. Flint, Noe and Gordan along with the chief residents. Housestaff also meet with the Program Director(s) every 6 months. At year’s end, the Clinical Competence Committee evaluates each houseofficer to judge their ability to advance/graduate. Similarly, with the Radiology training program, evaluation forms are distributed at rotations’ end and copies of completed evaluation are sent to the resident directly and to the Program Director (PD) for review. The PD meets with each resident every 6 months to review the evaluations. An additional project that was undertaken in academic year 2010-2011 was the development of a resident evaluation form to be used for clinical care assessment at the bedside. This form was designed for use by the MAH hospitalists as they concomitantly care for patients with the housestaff. Required external in-training written exams give to the residents and the programs an additional sense of accomplishment of training objectives and an ability to advise modification of an educational plan for each resident. Compliance with Duty-Hour Standards The Internal Medicine and Diagnostic Radiology Residencies consistently average 50-60 hours/week for each resident, well within the 80 hour maximum. Internal Medicine tracks duty hours on the New Innovations web-site noted above, and Radiology uses ‘GoogleDocs’. In both instances, duty hours are monitored by the chief residents and Program Directors. 5 Resident Participation in Patient Safety and Quality Two of the defined ACGME competency domains are those of Practice-based Learning and Improvement and that of Systems-based Practice: Practice-based Learning and Improvement Residents must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and life-long learning. Systems-based Practice Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on other resources in the system to provide optimal health care. With these requirements in mind, residents have been able to participate in a number of the robust initiatives with the MAH Department of Quality and Safety as well as their respective Departments. Efforts in the past year have led to a variety of initiatives that have positively impacted practice. Examples of projects by Medical residents that have emerged include: safer protocols for the management of deep venous thromboses, the safer use of anticoagulants and contributing to the development of a more efficient discharge process. The Radiology training program requires all of its residents to participate in a quality improvement project during their training. Residents are supported by the Program Director and faculty in the design and implementation of these projects. Examples of such initiatives include: a. reduction in the turn around time of abdominal CT examinations that are ordered from the Emergency Department; b. the use of metallic marker placement over the region of pain for all x-rays; c. the development of a consent form for pregnant females in need of Chest CT angiography; d. development of a teaching file folder on the PACS (picture archiving and communication systems) system to facilitate morning teaching and review conference; e. algorithms for the management of ovarian cystic lesions; f. the reporting and follow up of small pulmonary nodules. 6 Other developments of note: Interpersonal/Communication Skills and Professionalism Projects 1. Diagnostic Radiology Training Program A series of workshops have been conducted directed at radiology resident skill development in how to obtain informed consent; how to communicate fetal demise in the ultrasound suite; how to disclose medical error and how to communicate bad news in the mammography suite. This latter domain has been the focus of extensive work by Dr. J. Pierre Sasson, Program Director, Diagnostic Radiology, and Dr. Beth Lown, Director of the Mount Auburn Faculty Fellowship in Medical Education and MAH Director of Faculty Development. Data about communication training for Radiology residents was gathered from a national survey of Radiology training programs. (Sasson J, Zand T, Lown B. Communication in the Diagnostic Mammography Suite: Implications for Practice and Training. Acad Radiol 2008;15:417-424). Subsequently, an innovative program was designed and implemented that included patients as teachers and raters of interpersonal and communication skills. A series of Objective Structured Clinical Examinations (OSCE) were conducted, for both trainees and staff radiologists, which enhanced skill development in this challenging domain of delivering ‘bad’ news, particularly to patients undergoing diagnostic mammography with whom there typically is no prior relationship. (Lown B, Sasson J, Hinrichs P. Patients as Partners in Radiology Education: An Innovative Approach to Teaching and Assessing Patient-Centered Communication. Acad Radiol. 2008;15:425-432.) 2. Internal Medicine Residency Program For the past 25 years, we have conducted a weekly special version of bedside rounds. These rounds are directed at the residents and involve the Chief of Medicine, Director of Medical Education, Director of Faculty Development and a staff psychiatrist. A patient has been selected by one of the residents and permission sought to participate in these rounds. The patient is thus unknown to the rounding team and faculty. A resident is allowed 10-15 minutes to elicit the reason as to why the patient has been hospitalized, identify relevant psychosocial information, and if an emotional matter surfaces, to pursue it. A pertinent limited exam follows. In the subsequent discussion, the team uses the elicited primary data as the basis for discussion, and the identification of unanswered questions. Residents subsequently provide a follow-up on the patients seen as well as a brief literature review of any unanswered questions. These sessions permit direct observation of interviewing, physical examination and diagnostic skills. They also focus the discussion on the relevant psychosocial issues and are a stimulus for literature review. (Hatem C. Teaching Approaches That Reflect and Promote Professionalism. Acad Med. 2003;78:709-713.) In the past year, Drs. Lown and Carmody have completed a study of communication skill development within the Ambulatory Care Center. Phase One of an IRB-approved study sponsored by the Gold Foundation and the Department of Medicine (The Caring and 7 Communication Initiative) has been completed. The goals of the study were to evaluate an intervention designed to enhance the interpersonal and communication skills of Mt. Auburn Housestaff and to explore the concept of concordance in healthcare communication among patients and physicians. With appropriate approvals in place, resident-patient communication was videotaped and reviewed with the houseofficer, their advisor and the senior clinicians conducting the study. Most recently, Dr. Lown has conducted a study dealing with communication and shared decision-making in family meetings. The goals of this curriculum are to: Enhance residents’ abilities to support family members’ emotions, information needs and capacity during meetings in which a patient’s critical or terminal illness is discussed Recognize and utilize the expertise of team caregivers Engage families in shared decision making to integrate the patient’s values with best medical practice Teaching Skill Development Year-long programs aimed at enhancing the teaching skills of medical residents remain in place with an additional program for radiology residents being developed for implementation in the new academic year. The Mt. Auburn Fellowship in Medical Education has now graduated 42 faculty who have completed the year long program. These faculty provide an important resource in the teaching of residents as well as educational leadership within MAH. Examples of Scholarly Work Done by MAH Housestaff Medicine Bhargavi Yalamarti, M.D. – Engraftment Syndrome in allogenic hematopoietic stem cell transplants. Laila Khalid, M.D. – Bridging Anticoagulation for Perioperative Patients Sravan Jasti, M.D. – Racial disparities in Mortality of ESRD on Hemodialysis patients from USRDS Robert Spencer, M.D. – Circulating Levels of Soluble Endoglin Predict Presence of Pulmonary Arterial Hypertension Jeena Sandeep, M.D. – Iodine Content in Multivitamins Weihong Yang, M.D. – ANA, PBC and Autoantigenomics Smita Kohli, M.D. – Bleeding complications with PCI: Comparison of bivalirudin and eptifibatide Swetha Kommareddy – Drop in intraoperative PTM during minimally invasive parathyroid surgery is predictor of post op Calcium and PTH in one year. 8 Donald Misquitta, M.D. – Hypothyroidism and High Sensitivity CRP Bibek Koirala – Pneumocystis Pneumonia: A Ten Year Retrospective Review of Mount Auburn Hospital Cases Examples of Scholarly Work Done by MAH Housestaff Radiology In addition to the projects noted previously, the following papers involving MAH radiology resident authorship were published: Lastly, the academic year culminated in the first MAH Scholarship Day during which time various posters were presented that represented scholarly work done by the Medical and Radiology Housestaff. A compendium of important cases seen on the medical service was also compiled by Drs. Reitschuler-Cross and Nagaraja the medical chief residents. 9 Future Directions MAH Housestaff Medicine Dr. Fatima Afridi Curriculum Editor InfectiousDiseases.org Dr. Azadeh Assarpour Geriatrics Fellowship Beth Israel Deaconess Medical Center Dr. Sravan Jasti Nephrology Fellowship Hospital of U. Penn. Dr. Laila Khalid Chief Medical Resident Mount Auburn Hospital Dr. Smita Kohli Hospitalist North Shore Medical Center Dr. Bibek Koirala Infectious Disease Fellowship U. Mass. Memorial Medical Center Dr. Swetha Kommareddy Hospitalist Mount Auburn Hospital Dr. Donald Misquitta Informatics Research Fellowship Harvard Medical School/BMC Dr. Jeena Sandeep Hospitalist Mount Auburn Hospital Dr. Robert Spencer Chief Medical Resident Mount Auburn Hospital Dr. Bhargavi Yalamarti Hospitalist Mount Auburn Hospital Dr. Weihong Yang Rheumatology Fellowship Massachusetts General Hospital Chief Medical Residents: Dr. Archana Nagaraja Endocrine Fellowship U. Mass. Memorial Medical Center Dr. Eva Reitschuler-Cross Palliative Medicine Fellowship Harvard Medical School 10 Future Directions MAH Housestaff Radiology The graduating senior residents all passed the American Board of Radiology Oral Examination and are board certified as of June 2011. Dr. Christine Coolely Abdominal Imaging/Massachusetts General Hosp.l Dr. Nidhi Kacholiya MRI/Baylor University Medical Center (Dallas) Dr. Amy Oliveira Musculoskeletal Imaging/Massachusetts General Hosp. Primary Care Training At MAH In the Residency Matching Program for AY 2011-2012, three additional primary care interns were matched with MAH. This was made possible because of an earlier initiative on the part of Department of Medicine and Medical Residency Leadership to secure approval by the ACGME to approval the expansion of the MAH Medical Resident Program to 56 housestaff. Subsequently, in response to an RFP for the training of primary care residents (again Drs. Zinner, Flint and Mr. DiIeso were pivotal in securing the grant) the MAH was successful in securing funding for these residents (3/year to a total of 9; the extra residents will be funded by this grand and won’t be included in our Medicare cap numbers.) Information about the grant: Affordable Care Act: Primary Care Residency Expansion AGENCY: Department of Health and Human Services Health Resources and Services Administration (HRSA) AMOUNT: $2,879.998.00; GRANTEE NAME: PROJECT PERIOD: 09/30/2010 -09/29/2015 Mount Auburn Hospital; DIRECTOR: PROGRAM DIRECTOR/PRINCIPAL INVESTIGATOR: Eric Flint, M.D. Podiatry Program Historically, senior podiatry residents from Cambridge Health Alliance have gained surgical experience at MAH, but new opportunities have lead to the initiation of a new residency in Podiatric Medicine and Surgery at MAH. Thanks to the efforts of Drs. Basile, Nauta, Cook and Mr. DiIeso new program application has been submitted and the MAH was site-visited on 6/17/2011 by the Council on Podiatric Medical Education. Final approval is pending review by their internal committee, but the preliminary assessment of the MAH proposal and resources was extremely positive. The new Residency Director will be Dr.Emily A. Cook, DPM, MPH, CPH, who will bring extensive training and a passion for educational to this role. It is anticipated that the 3 year program when at full size will train 6 residents (2 at each level). The expectation is to recruit the initial class of residents for a September 2011 start. 11 Appendix 1: Medical Staff Education Committee Abookire, Susan, M.D, MPH Carmody, Matthew, M.D. Clough Jeanette D’Afflitti, Joseph, M.D. DiIeso, Nick Evans, Jeffrey, M.D. Flint, Eric, M.D. Goldsmith, Gary, M.D. Hatem, Charles, M.D. – (Chair) Kamat, Brinda, M.D. Khalid, Laila, M.D. Kohli, Smita, M.D. Lown, Beth, M.D. Mackenzie, Malcolm, M.D. McCaffrey, Anne, M.D. Nagaraja, Archana, M.D. Nauta, Russell, M.D. Noe, Cherie, M.D. Park, Brian, M.D. Pronio-Stelluto, Valerie, M.D. Sasson, Pierre, M.D. Schuler, John, M.D. Sehra, Shiv Tej, M.D. Shortsleeve, Michael, M.D. Walker, Xaviour, M.D. Zinner, Stephen, M.D. Chair, Quality and Safety Primary Care Center President and Chief Executive Officer Chair, Department of Psychiatry Chief Operating Officer Department of Emergency Medicine Program Director, Int. Med. Assistant Chair of Medicine Department of OBGYN Director of Medical Education Chair, Department of Pathology Internal Med. Resident (was PGY3, now Chief Res) Internal Med. Resident (was PGY 3) Director of Faculty Development, Dept. of Med. Dept. of OBGYN Medical Director, The Marino Center for Integrative Health Chief Resident Chair, Department of Surgery Associate Program Director, Int. Med. Res. Prog. Radiology Resident (was PGY4) Director of Med. Student Ed. – Dept. of Med. Program Director, Dept. of Radiology Director of Surgical Education Internal Med. Res. (Was PGY 2) Chair, Dept. of Radiology Internal Medicine Resident (was PGY 2) Chair, Dept. of Medicine 12