The Integumentary System
advertisement

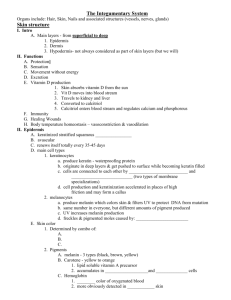
The Integumentary System I. Skin (Cutaneous membrane) A. Epidermis 1. Epidermal Layers a. Stratum Germinativum (basale) b. Stratum Spinosum c. Stratum Granulosum d. Stratum Lucidum e. Stratum Corneum 2. Nourishment of the Skin and Receptors in the Skin 3. Skin Color (Pigmentation) B Dermis (Corium) 1. Papillary Layer 2. Reticular Layer C. Hypodermis (Subcutaneous or Superficial Fascia) II. Glands of the Skin A. Sweat or Sudoriferous Glands 1. Eccrine Sweat Glands 2. Apocrine Sweat B. Sebaceous (Oil) Glands C. Ceruminous Glands III. Hair and Hair Follicle A. Sheaths of the Follicle 1. Epidermal Root Sheath a. External Root Sheath b. Internal Root Sheath B. Dermal (Hair) Papilla C. Sebaceous Gland D. Hair 1. Root of the Hair 2. Shaft of the Hair 3. Three concentric layers of the hair Shaft a. Cuticle b. Cortex c. Medulla E. Arrector Pili Muscle F. Hair Root Plexus IV. Nails V. Functions of the Integumentary System 1 The Integumentary System The skin and the skin derivatives-glands, hair, nails comprise the integumentary system. I. Skin (Cutaneous Membrane) The skin is an organ consisting of keratinized stratified squamous (epidermis) firmly attached to a thick layer of dense irregular arranged collagenous connective tissue (dermis). The skin is the largest organ of the body (10-15% of body weight). It forms the entire external covering of the body. It is continuous with the mucous membrane linings. (Mucous membranes line body passageways that open to the outside of the body.) The skin is composed of two types of tissue, epithelial and connective tissue. The epidermis of the skin is the surface layer. It is many cell layers thick of closely packed epithelial cells held by intercellular membrane junctions, such as the desmosomes. The dermis is a deeper layer is composed mainly of dense irregularly arranged collagenous connective tissue, with elastic fibers. The hypodermis (subcutaneous) layer or superficial fascia is below the dermis. It is a layer of loose connective tissue and adipose tissue. The hypodermis loosely connects the skin to the connective tissue covering (deep fascia) of the muscle. This arrangement allows the muscles to contract without pulling on the skin. A. Epidermis There are two types of epidermis - thin skin over most of the body; thick skin found in those parts of the body subjected to friction and pressure, such as palm of the hands and soles of the feet. 1. Epidermal Layers There are 5 epidermal layers or strata in thick skin. Starting from the base toward the free surface: a. Stratum Germinativum or Basale - this is the deepest layer of the epidermis. It is a single layer composed of cuboidal to columnar shaped cells lying on the basement membrane above the dermis. These cells are held together to each other by desmosomes. Within this layer mitosis occurs to replace cells lost from the free surface by desquamation. The cells in this layer are called keratinocytes. In the upper layers these cells undergo the process of keratinization. The keratinocytes will form and accumulate keratin while the cell's organelles and nucleus disappears. The cells die as they are pushed to the free surface. This genetically programmed cell death is called apoptosis.Eventually, the cell remnants are shed or desquamated. The cytoskeleton of the keratinocytes contains intermediate filaments (tonofilaments) composed of a protein that will form keratin. In the stratum germinativum the intermediate filaments are scattered not in bundles. The other cells in this layer are the melanocytes, which produce the melanin, a brown-black pigment. The long, slender projections of the melanocytes extend between the keratinocytes. The melanocytes transfer the melanin granules to the keratinocytes. The melanin gives the skin its color and absorbs UV light to protect the genetic material. Once inside the keratinocytes the melanin granules form a protective veil over the nucleus on the side toward the skin’s surface to shield the nuclear DNA from the UV light rays of the sun. 2 Langerhans cells (epidermal dendritic cells) are phagocytic macrophage cells. These cells arise from the red bone marrow and migrate to the epidermis. Merkel cells (tactile cells) contact the sensory neuron and function for touch sensation. b. Stratum Spinosum. - this layer is above the basal layer. It consists of 8-10 rows of flatter polyhedral or irregular shaped cells. Since the cells shrink during histological preparation, the cells appear with spine-like cytoplasmic projections as adjacent cells are held tightly by their desmosomes. In the spine-like projections the bundles of intermediate filaments of the cytoskeleton insert into the desmosomes that tightly join the cells to one another. Because of these projections, the cells have a. spiny or prickly appearance. In the stratum spinosum the keratinocytes phagocytose the melanin from the melanocytes and the process of keratinization begins. The keratinization is regulated by a hormone-like protein, epidermal growth factor (EGF). c. Stratum Granulosum - this stratum consists of 3-5 layer of flat cells. In the cytoplasm the intermediate filament bundles become more apparent and there are granules of keratohyalin, an intermediate substance in keratin synthesis. The keratohyalin granules gives this layer its name. Keratohyalin granules surround and organize the intermediate filaments into thicker bundles and convert the intermediate filaments into keratin.. As the keratohyalin granules accumulate and the intermediate filament bundles thicken the cells are in various stages of degeneration and by the top of this layer the cells die. Also present in the keratinocytes are membrane enclosed lamellar granules, which release by exocytosis lipid-rich secretions. This material fills the spaces between the cells of the upper epidermal layers. The lipid-rich secretion functions as water repellent sealant that retards loss of body fluids and entry of foreign substances. The stratum granlosum marks the transition between metabolically active cells and dead cells. d. Stratum Lucidum - this is a translucent or clear band. It consists of 3-5 rows of clear flat closely packed dead cells. The cells are indistinct. In the cytoplasm, the transparent substance, eleidin is present, which is a further development of the bundling the intermediate filaments of the keratin. The eleidin is transformed into keratin as the cells move into the stratum corneum layer. The stratum lucidum is absent from thin skin. It is only found in thick skin. e. Stratum Corneum - this is the uppermost layer on the free surface. It is composed of 25-30 parallel rows of flat closely packed dead cell remnants held by their desmosomes. Keratin a protein, consists of densely packed intermediate filaments and keratinohyalin granules that completely fill the dead cells. Due to the keratin, the lipid-rich secretion of the lamellar granules and secretions from the sebaceous and sweat glands, the stratum corneum protects against microbial invasion, injury and abrasion. Also keratin and lipid from the lamellar granules makes the skin water resistant, as water can slowly evaporate to or be taken in from the external environment. It takes 15-30 days (average 4 weeks) for a cell to move from stratum germinativum to the stratum corneum. The dead cells remain in the stratum corneum for another 2 weeks before they are shed. The outermost layers of the stratum corneum are then shed or desquamated. The lost cells are constantly being replaced by cells from the stratum germinatiuvm by mitosis. 3 2. Nourishment of the Skin and Receptors in the Skin There are no blood vessels in the epidermis, the dermis is well vascularized. The cells of the epidermis obtain nourishment by diffusion from capillaries in the dermis. Diffusion is sufficient for those cells closest to the dermis, as the cells are forced to the surface, they are cut off from nourishment and they die as their cytoplasm accumulates keratin. Most sensory receptors are in the dermis - pressure, heat, and cold. Touch and pain receptors extend into the epidermis. For light touch Merkel cells make contact with the sensory neuron. 3. Skin Color - Pigmentation The presence and distribution of the melanin determine skin color. Melanin is produced by melanocytes in the stratum basale. The melanin is then transferred to the keratinocytes and cells of the dermis by phagocytosis. The number of melanocytes among the races of man is the same. The difference in skin color is due to the amount of melanin produced by the melanocytes and the distribution in the keratinocytes. Dark-skinned people have appreciable amounts of melanin in all layers of the epidermis. Light-skinned people have relatively little melanin distributed among the epidermal layers as the melanin breaks down and disappears. Melanin serves a protective function of the genetic material against UV radiation of the sun. Skin color is also influenced by the yellow-orange pigment, carotene in the stratum corneum, dermis and hypodermis. Hemoglobin in the red blood cells in the blood vessels of the dermis gives the skin a pink to red color, as this pigment is red. Epidermal Differences between Thick and Thin Skin Thick vs Thin Skin - this refers to the number of strata and relative thickness plus other features. Thin skin is located in all parts of the body, except the palms of hands and soles of the feet. Thin skin has hair, hair follicles, arrector pili muscles and sebaceous glands. In the thin skin stratum lucidum is absent, stratum granulosum, and stratum corneum are thin. The thin skin has fewer sweat glands and sparser distribution of sensory receptors than thick skin. Thick skin is only located on the palms of the hands and soles of the feet. Thick skin has well-formed strata spinosum, lucidum and corneum. Thick skin lacks hair, hair follicles and attached structures. It has more sweat glands and the sensory receptors are more densely clustered than in thin skin. Pressure or abrasion increases the rate of mitosis to thicken the skin to form a callus. B. Dermis or Corium Below the stratum germinativum and the basement membrane is the dermis. The dermis is mainly composed of dense and irregular arranged thick bundles of collagenous and elastic fibers that interlace in a net-like arrangement. Between the fibers and a few adipose cells there are also fibroblasts (cytes), macrophages all suspended in a small amount of ground substance. In the dermis between the fibers there are blood vessels, nerves, sense organs, sebaceous glands, sweat glands, and hair follicles. 4 The dermis has two indistinct layers: 1. Papillary layer - this layer fits closely against the stratum basale under the basement membrane. The layer is so named, because it has dermal papillae or projections that protrude up into the epidermis. Pushing down into the dermis are epidermal ridges that conform to the contours of the dermal papillae. The dermal papillae help to anchor the epidermis to the dermis. The connective tissue is looser arranged than in the reticular layer (see 2. below). Dermal Differences between Thick and Thin Skin Thick Skin - On the palms of the hand, soles of the feet the papillae are very numerous, high and narrow to form parallel ridges that cause the overlying epidermis to form epidermal ridges, which form the fingerprint and footprint patterns. The epidermal ridges increase surface area for gripping. In the papillae there are capillaries, sense organs for temperature and pressure and pain. Thin skin – The dermal papillae are lower, broader and fewer and there are no epidermal ridges. 2. Reticular layer - this is the deep layer of the dermis. It consists of dense irregular arranged collagenous fiber bundles and elastic fibers. Due to the arrangement of the collagenous and elastic fibers, the reticular layer can be stretched and returned to its original shape after stretching. The reticular layer has extensibility and elasticity. In reticular layer between the bundles of collagenous fibers are hair follicles, nerves, sebaceous glands and sweat glands. The connective tissue fibers continue into the hypodermis. C. Hypodermis This layer is below the dermis but not considered part of the skin. It attaches the skin to the underlying structures. The hypodermis is loose connective tissue with groups of fat cells (adipose tissue) among the fibers. This tissue is also called the subcutaneous tissue or superficial fascia. Accessory Structures of the Skin These structures are derived from the epidermis during embryogensis. II. Glands of the Skin Glands are derivatives of the epidermis but are located in the dermis and are connected to the epidermal surface by way of ducts (exocrine glands). The glands are classified according to how the product produced by the gland cells leaves the cells (i.e. secreted). A. Sweat or Sudoriferous Glands Sweat glands are distributed over most of the body surface. They are most numerous in the palms of the hands and soles of the feet. 1. Eccrine Sweat Glands - These glands are simple tubular shaped glands and are merocrine glands, as the cells of these glands do not lose any of their cytoplasm when they secrete. The gland cell synthesizes the secretion and discharges it by exocytosis. The glands are simple tubular structures, highly coiled at their base. The long straight secretory duct penetrates the surface as the sweat pore. The secretion is mainly a 5 hypotonic watery solution of NaCl, urea and other salts. The amount of sweat secreted depends on the temperature, humidity, muscle activity and stress. The main function of the eccrine sweat gland is to regulate body temperature through evaporation of the sweat as large quantities of heat energy leaves the body surface. These glands play a small role in the elimination of N waste products – urea, uric acid and ammonia. 2. Apocrine Sweat Glands - these glands are apocrine glands. The apical part of the cytoplasm of the gland cell accumulates the product . Then this portion of the cell is pinched off as the secretion. The remaining part of the cell regenerates and repeats the process. Apocrine sweat glands produce a viscous secretion of organic substances (eccrine secretion + lipid and protein). This secretion is thicker than true sweat and has an odor. Apocrine sweat glands are located in the axilla of the body (armpits), pubic area, around anus, on the scrotum and external genitalia of the female, around the nipples of the breast and the bearded regions of the face of adult males. The apocrine sweat glands are large simple tubular glands. They extend into the dermis and hypodermis. They secrete onto the surface of the skin or into a hair follicle. To help move the secretion out of the gland contractions of smooth muscle cells (myoepithelial cells) around the gland and its duct forces the secretion out. Mammary glands are modified apocrine sweat glands. They produce a white organic substance, milk. The mammary glands are alveolar (flask) shaped glands, rather than coiled tubular glands. Eccrine sweat glands function soon after birth, while apocrine sweat glands function at puberty and afterward. The apocrine sweat glands function during emotional stress and sexual activity. B. Sebaceous (Oil) Glands These glands are holocrine. The entire cell and its secretion contribute to the secretion. The secretion is called sebum an oily, white lipid substance. The sebaceous glands lie in the dermis and empty the sebum into the hair follicle to keep the hair and skin from drying out. The sebum keeps the skin and hair soft and pliable. Sebum also has waterproofing and antibacterial action. The shape of the sebaceous glands is alveolar or acinar (flask) shape and the ducts open into the hair follicles. Sebaceous glands are not usually found in hairless regions of the body. The palms and soles lack sebaceous glands. C. Ceruminous Glands Ceruminous glands are modified sweat glands. The ceruminous glands are located in the external auditory canal and produce cerumen (earwax). The cerumen provides a sticky barrier to prevent entrance of foreign bodies into the ear. Cerumen is a combination of sebaceous and ceruminous gland secretion. III. Hair and Hair Follicle Hair (pili) covers most of the body, it is heavily distributed over scalp, eyebrows, around external genitalia (pubic hair). There are few hairless regions such as lips, eyelids, and palms of hands and soles of the feet. The hair and its hair follicle grow as a result of mitosis of epidermal cells of the stratum germinatiuvm at the bottom of the hair follicle. This region is known as the hair bulb. In the hair bulb there is a mass of undifferentiated cells, the hair matrix, which produces the hair and hair follicle. The hair matrix cells arise from the stratum basale or germinativum. This stratum is responsible for the growth of existing hair and new hair in the hair follicle. The follicle is epidermis that extends from the epidermis into the dermis. 6 A. Sheaths of the Follicle The sheaths are downward continuation of the epidermis into the dermis. 1. Epidermal Root Sheaths The follicle has 2 epidermal sublayers: a. External Root Sheath - it consists of the strata germinativum and granulosum. b. Internal Root Sheath - it consists of the stratum corneum. This sheath is between the hair and the external root sheath. 2. Dermal Root Sheath Surrounding the epidermal root sheath is an outer layer of connective tissue, the dermal root sheath. B. Dermal (Hair) Papilla Areolar connective tissue of the dermis protrudes into the hair bulb as the dermal or hair papilla. The papilla contains blood vessels to nourish overlying living hair matrix follicle cells, from which the hair grows. C. Sebaceous Gland The sebaceous gland empties into the hair follicle. D. Hair The hair has two main parts. 1. Root of the hair - the root of the hair is in the hair bulb region. This is a region of mitotic active cells from which the hair grows. 2. Shaft of the hair - the hair shaft consists of dead keratinized cells that develop from the root. The root of the hair and hair bulb are below the surface. The shaft of the hair extends above the surface of the skin. 3. Concentric layers of the hair shaft and root - there are 3 concentric layers to the hair from outer to inner. a. Cuticle - the cuticle on the surface is a single layer of cells with hard keratin. The cells overlap like shingles on the side of a house, with the free edges pointing toward the top of the hair. b. Cortex - the cortex contains hard keratin that gives the hair its stiffness and the melanin that colors the hair. c. Medulla - the medulla is in the central axis of the hair. It contains soft keratin and melanin. Gray hair is due to a lack of pigment and air spaces between the cells of the hair in the medulla and cortex. E. Arrector Pili Muscle The arrector pili muscle runs diagonally from the papillary layer of the dermis (origin) to the dermal root sheath (insertion). It is a bundle of smooth muscle. Contraction of the arrector pili muscle pulls the hair follicle, so the follicle and hair stands up perpendicular (vertical) to the skin surface. The contraction of the arrector pili muscle causes the skin to bulge. It’s contraction also squeezes the sebaceous gland to force secretion to the surface as the sebaceous gland lies in the angle between the hair follicle and the arrector pili muscle. 7 F. Hair Root Plexus Around each hair follicle are sensory nerve endings (dendrites) sensitive to touch. The nerve endings perceive touch if the hair is moved. G. Hair Growth and Hair Loss Hair grows in a hair growth cycle of 3 stages: 1. Anagen In anagen stage, the undifferentiated cells in the hair follicle multiply pushing the dermal papilla deeper into the dermis. The cells above the dermal papilla differentiate into mature hair cells which synthesize keratin. 2. Catagen In catagen stage, the mature hair cells die (undergo apoptosis) as they are pushed upward away from the dermal papilla. The hair follicle shrinks as the dermal papilla regresses upward and the hair losses its anchorage. 3. Telogen In telogen, the hair goes into a resting stage and the hair falls out. The hair loss may occur during catagen or telogen. The hair cycle repeats itself again with anagen. In young adults, scalp hair follicles are in anagen between 6-8 years, 2-3 weeks in catagen and 1-3 months in telogen. 90% of scalp hair follicles are in anagen. Scalp hairs in anagen grow at a rate of 10-18 cm/year. Hair grows fastest from adolescence (from 10 years old to about 20 years old) until 40 years old. After that an increased percentage of the hair follicles is in categen or telogen rather than in anagen. IV. Nails On the dorsal surface of the distal phalanges of the fingers and toes, the strata corneum and lucidum are heavily keratinized forming nails. A. Nail Plate or Body - is the visible part of the nail. B. Nail Root - is the part of the nail buried in the fold of skin. C. Nail Bed - is the epidermis below the nail; the nail plate rests on the nail bed. D. Lunula - proximal end of the nail forming the whitish area, due to thickening of the stratum germinativum. E. Nail Matrix - the proximal end of the nail plate. It is a region of thick stratum germinativum from which the nail grows by mitosis. F. Eponychium (Cuticle) - at the proximal end of the nail there is a narrow fold of epidermis on the upper surface. It consists of stratum corneum. G. Hyponychium - thickened stratum corneum below the free edge of the nail. 8 Nails have a pink coloration due to the capillary network visible through the nail body. V. Functions of the Integumentary System A. Protection (First line of defense from external environmental factors) The skin forms a physical, chemical and biological barrier that prevents any foreign matter from invading the body and also protects against mechanical injury. Physical barrier – The continuity of the skin and the hardness of the keratin allows the skin to protect against loss of body water to the environment as keratin is a tough, water-resistant substance along with the lipid secretion of the lamellar granules. When the skin is subjected to friction repeatedly it becomes thickened and if severe forms calluses. Chemical barrier - The surface of the skin is acidic (pH 4-6.8) due to sweat. The sweat and the sebum act as an antiseptic to retard microorganism growth. The skin protects against ultraviolet radiation through the melanin pigment, as melanin absorbs UV radiation. Biological barier – The Langerhans’ cells in the epidermis and the macrophages in the dermis phagocytose microorganisms. Hair and nail functions are mainly protective. 1. Hair Functions Head hair – Protects scalp from UV light, cushions a blow to the head, and insulates the skull. Body hair – It is too sparse to have an insulating benefit. Hair guarding nostrils, external ear canal, and eyelashes prevent entry of foreign particles and insects. Hair root plexus – Sensory nerves surrounding base of the hair follicles to perceive light touch. 2. Nail Functions Nails protect exposed tips of fingers and toes and limit their distortion when subjected to pressure. They help grasp and manipulate small objects and allow for scratching of the body. B. Body Temperature Regulation Thermoregulation by the homeostatic negative feedback system maintains a constant body temperature (37O C). C. Excretion Secretion of sweat causes elimination small quantities of N-waste product (urea, uric acid, ammonia) and NaCl. D. Absorption Absorption of lipid soluble molecules as in transdermal (transcutaneous) drug administration. E. Sensation Within the papillary layer of the dermis nerve endings and sense receptors provide the body with information concerning changes in the external environment, such as temperature changes (heat and cold), touch, pressure and pain. F. Vitamin D Synthesis In presence of a small amount of sunlight or UV light a sterol (a fatty material) in the skin is changed to a precursor molecule that is then converted to the active form of vitamin D, calcitrol. Calcitrol is a hormone and is essential for absorption of Ca and PO4 from the digestive system. Ca and PO4 are needed for growth of bones and teeth. Ca is also required for normal nerve and muscle function and blood clotting. G. Blood Reservoir The dermal blood vessels hold large volumes of blood. When body organs need blood these blood vessels 9 constrict and shunt blood to the organs that need it. H. Immunity The Langerhans' cells of the epidermis and macrophages in the dermis are involved in immunity against invading microorganisms by phagocytosis and digestion. Because the skin plays a role in all the functions listed, the skin plays a major role in maintaining homeostasis of the body. 10 Some stimulus (stress) disrupts homeostasis by causing an increase in Controlled condition Body Temperature Receptors Thermoreceptors (temperature-sensitive receptors) in skin and brain Input Nerve impulses Return to homeostasis when response brings body temperature (controlled condition) back to normal Control center in brain Output Nerve impulses Efffectors Increased sweating from Sudoriferous (sweat) glands causes increased heat loss by evaporation Response Decrease in body temperature 11