Learning DIsabilities Fact Pack - Gloucestershire Hospitals NHS Trust
advertisement
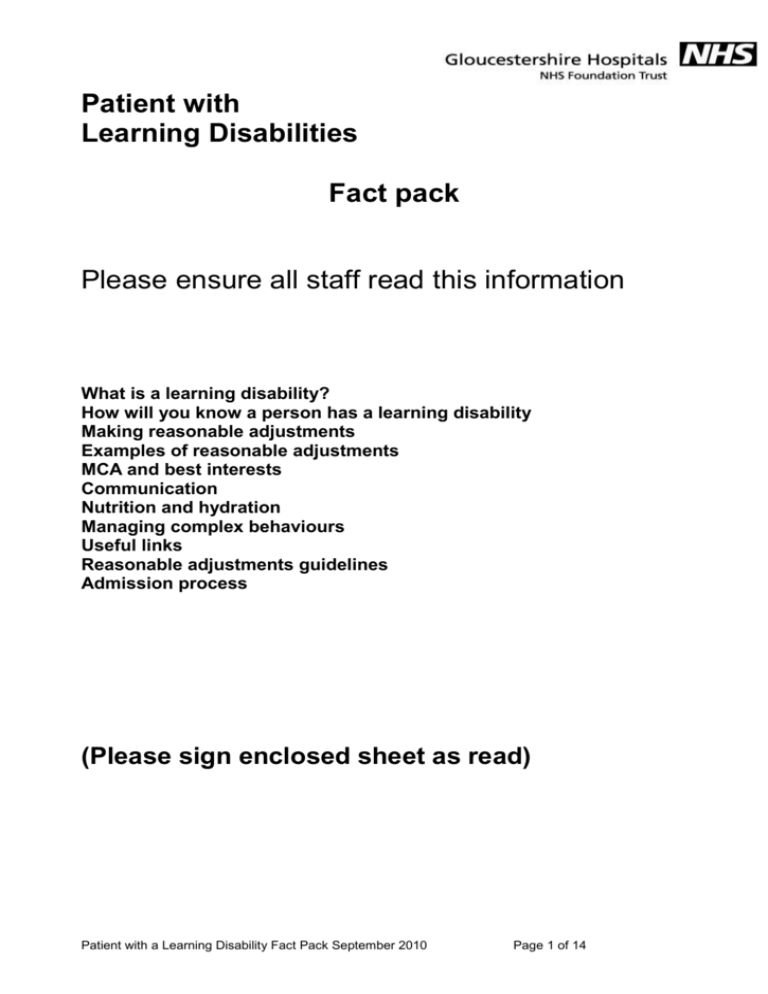
Patient with Learning Disabilities Fact pack Please ensure all staff read this information What is a learning disability? How will you know a person has a learning disability Making reasonable adjustments Examples of reasonable adjustments MCA and best interests Communication Nutrition and hydration Managing complex behaviours Useful links Reasonable adjustments guidelines Admission process (Please sign enclosed sheet as read) Patient with a Learning Disability Fact Pack September 2010 Page 1 of 14 Learning Disabilities Fact Pack - Please sign when you have read this pack Ward/Dept …………………………………………… Signature NAME - Please print Patient with a Learning Disability Fact Pack September 2010 Page 2 of 14 Date Learning Disabilities Fact Pack - Please sign when you have read this pack Ward/Dept …………………………………………… Signature NAME - Please print Patient with a Learning Disability Fact Pack September 2010 Page 3 of 14 Date What is a learning disability? • Being less able to cope without support (social impairment) • Being less able to understand new or complicated information (mental impairment) • Starting before adulthood and has long term effect on development A learning disability is not a mental illness and does not come under Mental Health Some people with a learning disability also have a mental illness (this is called a dual diagnosis) People with Learning Disabilities have greater health needs They are at a greater risk of all the following: • Respiratory disease • Epilepsy • Sensory Impairments • Helicobacter Pylori Infection (bacterium in the stomach) • Gastrointestinal disease • Heart Disease • Thyroid dysfunction (particularly people with Down’s Syndrome) • Mental ill health • Cancer; oesophageal, stomach, gall bladder & leukaemia. How will you know if a patient has a Learning Disability? • Documented that the patient has a learning disability (eg. in medical notes, on reports etc) • Requires significant assistance with activities of daily living / social adjustment • Difficulties identified from a range of information not explainable by a specific condition • Known to Learning Disability consultant or Community Learning Disability Team • Many people with Learning disabilities will have a relative/carer supporting them. – discuss with relative/carer • If unsure – contact Learning Disability Liaison Nurse Team. Patient with a Learning Disability Fact Pack September 2010 Page 4 of 14 Making reasonable adjustments The Disability Discrimination Act makes it a duty for health services (and all service providers) to make reasonable adjustments in order to; eliminate discrimination that is unlawful under the Act. To promote equality of opportunity between disabled persons and other persons To take steps to take account of a person’s disabilities, even where that involves treating the disabled person more favourably than other persons The duty to make reasonable adjustments applies to all of us in the health service; the porter, hotel service staff, doctor, nurse, HCA, phlebotomist, physio, OT, SLT, dietician, caterer, administrative staff, managers…… YOU! Failure to make reasonable adjustments • When the effect of the failure is to make it impossible or 'unreasonably difficult' for the disabled person to make use of services … and the failure is not justified it is unlawful. Examples of Reasonable Adjustments for people with learning disabilities. • Booking double appointments • Getting patient seen quickly, avoiding queuing/waiting • Providing a side-room • Hi-low bed • Providing the first appointment of the day • Funding for a carer to stay with the patient • Enabling a carer to support patient (for an investigation, going to theatre) • Adapting treatment • Providing easy read information • Meet individual needs Patient with a Learning Disability Fact Pack September 2010 Page 5 of 14 Consent and the Mental Capacity Act • Have you considered consent issues? No one can give consent on behalf of another adult. • Have you assessed if the person has capacity to consent? Can they; - understand what they are making a decision about - retain & use the information in order to make a decision, - weigh-up the benefits and risks - communicate their decision in any way • All consent decisions need to be clearly documented Check the intranet A-Z Safeguarding Adults for information on the mental capacity act. If in doubt contact the Hospital Liaison Nurse Learning Disability. Best interests Where a person lacks capacity to consent all acts done or decisions made on their behalf must be in their best interest. Best interest decisions should include the views of the patient relatives, carers, other professionals involved etc. & be documented When decisions have to be made in an emergency they are the responsibility of the decision-maker eg. doctor/consultant and relatives/carers informed. With serious decisions if the patient has no one unpaid to consult about best interests involve an Independent Mental Capacity Advocate (IMCA). For more information See Mental Capacity Act page on intranet Patient with a Learning Disability Fact Pack September 2010 Page 6 of 14 How does the person communicate? A person with a learning disability will often have communication difficulties. To find out how someone communicates; • Interact with the person • Ask to see the traffic light hospital assessment • Talk to family and carers; ask about their behaviour and what it means (if they have complex behaviour) • Look for additional information such as speech and language therapy reports. Additional ways of communicating Objects of reference eg. use a cup to ask “ would you like a drink?” Pictures / photos Body language (what is it telling you, what is yours telling them?) Expression Gestures / miming Speak slowly and clearly Give the person time to process the information & respond. Check understanding, if necessary repeat the information or say it in a different way. • Look at expressions and body language • Sign language - makaton • Utilise the hospital communication book. • • • • • • • • Assessing pain / discomfort • • • • Can the person describe the pain or point to where it is? Adapt communication eg. “pain” “hurt” “ouch” “sore” Can person use a pain scale ; 1 - 5 or sad - smiley faces Utilise hospital communication book If patient unable to formally communicate pain look for other indicators; • Colour, breathing, • Behaviour; restless, aggressive, vocal or withdrawn • Discuss with relatives/carers how patient usually indicates pain and document this. Patient with a Learning Disability Fact Pack September 2010 Page 7 of 14 Nutrition and hydration Have you got information about the patient’s nutritional needs/support; from the patient, relatives or carers, notes, assessments etc? Does the patient need specialised equipment to maintain independence? Incorporate above into care-plan as required If a procedure such as inserting an NG tube is necessary – consider psychological support/reassurance from carers/family Patients who have a learning disability should have their food / fluid intake monitored in a way that is informative, accurate and up-to-date. The patient may need support to choose food from menu or may need this done for them. Managing Complex / challenging behaviour • How does the patient usually behave - (carers, hosp traffic light assessment, guidelines) and how is it managed? • Has the patient shown these behaviours before: when, cause, duration, how managed? • Underlying health needs: ill health, pain, hot, cold, hungry, thirsty, nausea, constipated, epilepsy etc. • Medications – new medicines – side effects. Daily medications given on time (mental health, epilepsy etc.) • Environment – too noisy, quiet, over/under-stimulating, boredom (what is home environment like) • Complete patient risk assessment • Communicate in a way they understand (carers, hosp assessment, capacity). Patient with a Learning Disability Fact Pack September 2010 Page 8 of 14 • What do they find calming. • Slow down, go at their pace. • Awareness of preferences eg touch. • Procedures that hurt, cause anxiety, consider sedative, pain relief, emla cream etc. • Familiarise with equipment – desensitisation. • Additional support, specialist support (inform lead nurse) Supporting carers • The carers role is to assist where necessary, to promote familiarity to reduce fear and anxiety that the patient may be feeling • The carer may also be key to communication with the patient. • It is the responsibility of the nurse in charge to ensure that all planned care and treatment is delivered appropriately and that…… The carer receives a rest break The carer is kept informed of progress on a need to know basis Refer to policy ‘Supporting Carers of Patients Requiring Extra Physical or Emotional Support’ (policy number A0059) Patient with a Learning Disability Fact Pack September 2010 Page 9 of 14 Reasonable adjustments guidelines – Outpatients / emergency department DDA – Disability Discrimination Act 2005 It is the duty of all public bodies to promote equal opportunity for disabled people Eliminate unlawful discrimination Promote positive attitudes Encourage full participation in public life To undertake ‘reasonable adjustments’ If known learning disability inform learning disability liaison nurse 08454 224985/53 – If out of office hours, please leave a message How does the person communicate? Adapt communication style to meet individual needs. Requires aids/support – utilise hospital communication book, objects of reference Talk to family and carers Ask for traffic light assessment – if patient does not have one provide one for the patient / carer to complete. (copies held in outpatients, Emergency Department and Acute Care Units) Provide double appointments Capacity and consent – MCA 2005 Can the person understand, retain, weigh up and communicate their decisions If capacity is lacking – best interest decisions may be made in consultation with those involved with the person. Serious decisions will need IMCA involvement if family or unpaid carers are not involved. Follow trust Mental Capacity Policy Refer to learning disabilities liaison nurse Managing patients anxiety / behaviours Consider patient safety Is the patient safe on a hospital trolley? Are there hazards close by? (medical equipment?) Complete trust patient specific risk assessment Enable additional support Provide a quiet area to wait in Reduce waiting time Allow the person and their carer to leave the area and return at a given time or by mobile phone contact Adjust future appointment times to beginning or end of clinic Provide double appointments Provide easy read information to assist understanding Is the agitation a result of pain / discomfort? Consider mild sedative for anxiety Pain assessment Find out how the person express pain Document how the person expresses pain Talk to carers Refer to liaison nurse / pain team for provision of pain assessment tool. Refer to traffic light assessment Carers Listen to information provided by carers If there is a long waiting time – periodically check that the patient and carer are ok Offer help and support as required Keep patient and carers informed. Refer to carer policy number A0059 Patient with a Learning Disability Fact Pack September 2010 Page 10 of 14 Reasonable Adjustments Guidance checklist for a patient with a Learning Disability or a patient with Dementia Please use this checklist to consider if any reasonable adjustments are needed for your patient – Remember it is a legal requirement to make reasonable adjustments where these are indicated. You must document in the patients Health Record if: no Reasonable Adjustments are required Or If Reasonable Adjustments are required document these in the patients Health Record or care plan For the patient with a Learning Disability: Refer all patients and at each time of presenting, to the Learning Disability Liaison Team: 08454 224985 or 08454 224953 Check - Does the patient have a Hospital Traffic Light Assessment Document - If not provide patient/carer with this document and ask for this to be completed - (Document available on wards / Emergency Department / Acute Care Units and Learning Disabilities Liaison Nurse) For the patient with Dementia: Consider referral to Mental Health Liaison Team for further advice and support: Contact number - GRH ext: 5490 - Does the patient have a ‘This is Me’ Document - - Does the patient have the ‘Living Well Hand’ handbook – if yes view this with the patient and carer, use information to plan care Check communication needs Adapt communication style to meet individual needs. Slow down and allow more time for patient to process information Include carers in communication Gestures, objects of reference, pictures, hospital communication book Increase observations to spot signs of deterioration Is there a hospital traffic light assessment (patients with Learning Disability) If not provide patient/carer with this document and ask for it to be completed (available on wards / Emergency Department / Acute Care Units and Learning Disabilities Liaison Nurse) Is there a ‘This is me’ document (dementia) If not provide patient/carer with this document and ask for it to be completed Capacity to Consent Consider is it appropriate to assess capacity? Follow Trust Mental Capacity Act Policy Can the patient understand, retain, weigh up and communicate decisions– use Trust Assessment of Capacity document GHNHSFT – Y0711-01-10 or Consent Form 4 If care is in patients best interests consult with those who know the patient well and document decisions. Pain management Check how the person communicates pain Record indicators eg; facial expression, guarding, behaviours, Consider words used to express pain Pain tools eg; Abbey Tool, communication book, pain scales Managing risks Clinical care risks: eg. epilepsy, needs personalised equipment, care-plans, assessment. Environmental risks: eg. sharps, medical equipment, creams, medications Behaviour risks: eg could harm self or others. Safety: Increased level of support, side room behaviour management guidelines Managing anxiety, agitation Offer reassurance, tone of voice, body language Is additional support required? Adjust the environment eg; side room Complete risk assessment / inform lead nurse Management guidelines around behaviours? PRN medication to reduce anxiety. Work with relatives/carers if appropriate View page 2 You must document in the patients Health Record if no Reasonable Adjustments are required Patient with a Learning Disability Fact Pack September 2010 Page 11 of 14 Or if Reasonable Adjustments are required document these in the patients Health Record or care plan Managing mental health needs Consider referral to Mental Health Liaison Team for further advice and support: Contact number - GRH ext: 5490 Check timing of medications If patient known to have a Consultant Psychiatrist involve them in decisions about medications Document signs of deterioration Medication management Sensitive to timing of medications Check branded medication Tablets or syrups Specific way of taking medication Explain clearly any changes to medication – check understanding Accessing other departments eg. OPD, X-ray Needs carer / family support Difficulty with waiting – if yes - inform senior staff within the dept to needs and requirement to fast track Anxious – quiet area provided Understanding information – easy read leaflets, written information to take away Contact number provided for advice Extra time allowed for appointment 1:1 support at mealtimes. Consider regular prompts/assistance to ensure sufficient fluids/food Cut up food/soft diet/risk of choking - red tray Special equipment – own cup/cutlery SALT guidelines in place Accurate recording – fluids, food input/output Current PEG feeding regime Weight o Managing nutritional needs Managing personal care needs Level of carer support required (ward staff remain responsible for all aspects of care). Continence – prompting, toileting, pads, bowel charts Additional support – from hospital? Supporting carers Refer to carers policy (A0059) Carers badges, parking permits Use of staff toilet Establish role of carer & work in partnership Consider funding implications Managing discharge Always provide a written discharge summary for patient/relatives or carers to include diagnosis, treatment, medication changes and follow-up If needs are complex consider discharge planning meeting Training needs of carers Equipment/dressings for the home OT assessment Referral to specialist services Detailed written discharge summary If patient with a Learning Disability – Inform CLDT if required If patient with Dementia – Inform Managing Memory Together if required Patient with a Learning Disability Fact Pack September 2010 Page 12 of 14 Patient with a learning disability Refer all patients and at each presentation to the Hospital Learning Disabilities Liaison Nurse Team (HLDLNT) 08454 224953 / 85 Patient presents to: Pre-admission Out Patients Department Assess patient needs. Ask Family member or Carer for the traffic light assessment. Document - Refer to Trust Reasonable Adjustments Checklist Are the patients’ needs complex? Assess patient and Carer needs. Ask Family member or Carer for the traffic light assessment. Document - If If aware before presentation to hospital setting HLDLNT liaise with Health Care Team, patient, family and Carers within the Community setting and liaise with Trust Health Care Team If not available, provide one for patient / family/ carer to complete (Copies held in E/Dept and ACU) Patient presents to Un-scheduled Care not available, provide one for patient / family/ carer to complete (Copies held in E/Dept and ACU) HLDLNT complete specialist assessments liaise with health care team place Trust ALERT sticker on patients Health Refer to Trust Reasonable Adjustments Checklist Enter on Triage Screen Refer to individual support plan Record and document on inner cover Liaises to ensure Clinical ALERT on ‘Patient First’ Liaises to ensure Clinical ALERT on ‘PAS’ Is patient to be admitted? No Refer to Trust Reasonable Adjustments Checklist Admission to ward Yes Refer to HLDLNT Assess patient and Carer needs Ask Family member or Carer for the traffic light assessment. Document Complete Reasonable Adjustments Checklist Documents if adju Liaise with HLDLNT throughout admission and discharge planning plans Patient with a Learning Disability Fact Pack September 2010 Complete care Page 13and of 14risk assessments, include reasonable adjustments identified If patient to be admitted inform ward that patient has a known learning disability and reasonable adjustments identified No support plan If yes -inform ward patient has a known learning disability reasonable adjustments identified and copy the Support plan No Provide information regarding treatment and follow up in format that patient understands Useful links Hospital intranet site – learning disabilities Hospital intranet site – Health Facilitation Team 2gether South West NHS – shared easy read resources ‘A picture of health’ see link below. www.apictureofhealth.southwest.nhs.uk Learning disability liaison nurses ; Carol Forbes 08454 224985 / 07825927912 Bev Farrar 08454 224953 / 07825928091 Patient with a Learning Disability Fact Pack September 2010 Page 14 of 14