Which commonly used nebuliser solutions are compatible?
advertisement

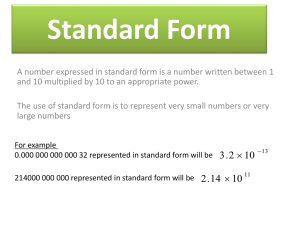
Medicines Q&As Q&A 100.6 Which commonly used nebuliser solutions are compatible? Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Before using this Q&A, read the disclaimer at www.ukmi.nhs.uk/activities/medicinesQAs/default.asp Date prepared: 31st January 2012 Background As administration of one drug by nebulisation can take 15-20 minutes, mixing nebuliser solutions might aid compliance by decreasing nebulisation time (1). Answer There is little published evidence on the compatibility of nebuliser solutions. Where available, it is preferable to use licensed combination products. The Summary of Product Characteristics for Atrovent® (ipratropium) UDVs (unit dose vials) indicates that it can be combined with a short-acting beta2-agonist in the same nebuliser chamber, for simultaneous administration where co-administration is required (2). Pulmicort (budesonide) respules® can be mixed with terbutaline, salbutamol and ipratropium (3). Unless specifically stated in the Summary of Product Characteristics, the manufacturers of nebuliser solutions do not recommend that they are mixed and as such these mixtures are unlicensed. In-house data from manufacturers and the limited published data suggest that two-way mixes of some nebuliser solutions are physically and/or chemically compatible in some cases (4-8), as the summary table below shows. Table 1. Compatibility table of commonly used nebuliser solutions Drug Budesonide Budesonide Fluticasone Ipratropium Salbutamol Terbutaline Colistimethate N/A C C C NI C C C NI C C NI N/A C† Fluticasone N/A Ipratropium C C Salbutamol C C C Terbutaline C C C N/A Colistimethate NI NI NI C† C N/A NI † NI NI Compatible Not applicable No information ensure salbutamol solution or any diluent used is preservative-free In general, drugs should not be mixed unless there is firm evidence that they are compatible (9). If mixing is necessary, 0.9% sodium chloride is usually used as a diluent (9,10). Solutions should be mixed immediately prior to use (1) and using aseptic precautions (9). To maximise nebulised drug, a minimum volume of 3 to 4mL should ideally be nebulised. This volume is required to reduce the amount of drug that may be left in a ‘dead space’ at the end of nebulisation; although this is less with newer nebulisers and no further dilution of commercial nebuliser solutions is necessary (10). If turbidity, colour changes or precipitation occur, the mixture should be discarded (1). Any unused Available through NICE Evidence Search at www.evidence.nhs.uk 1 Medicines Q&As solution should be discarded. Regardless of whether nebulised solutions are mixed, patients should be monitored to ensure that the required clinical response is being obtained (1). There is one report of chemical compatibility between budesonide and the combination product Duovent® (fenoterol and ipratropium) mixed in a 1:1 volume ratio (7). There is no information available for other three-way mixes of nebuliser solutions and therefore other mixes cannot be recommended. The mixing of nebuliser solutions should only be undertaken in the best interests of the patient and only by a person competent and willing to do so. Instructions for mixing should be in writing (11). In most cases the mixing of nebuliser solutions is unlicensed; healthcare professionals should be aware if a medicine is to be used outside its licence and take responsibility for its use in this manner. Summary Mixing of nebuliser solutions should only be undertaken in the best interests of the patient and only by a person competent and willing to do so. Instructions for mixing should be in writing. Two-way mixes of nebuliser solutions have been used for a variety of respiratory medicines. Table 1 indicates those that are deemed to be compatible. Unless specified in the Summary of Product Characteristics, the manufacturers of nebuliser solutions generally do not recommend that they are mixed and as such these mixtures are unlicensed. In most cases the mixing of nebuliser solutions is unlicensed; healthcare professionals should be aware if a medicine is to be used outside its licence and take responsibility for its use in this manner. Where available, it is preferable to use licensed combination products. Two-way mixes should be used immediately, and should be discarded if precipitation, turbidity or colour changes occur. The mixture may be diluted with 0.9% sodium chloride to a volume of between 3 and 4mL. Any unused solution should be discarded. Patients should be monitored to ensure continued clinical response to treatment. Duovent® (fenoterol and ipratropium) and budesonide admixture have been shown to be chemically compatible. Data on other three-way mixes are lacking and therefore cannot be recommended. Limitations There is little published evidence on the compatibility of nebuliser solutions (by brand or medicine class). References (1) Joseph JC. Compatibility of nebulizer solution admixtures. Ann Pharmacother 1997;31:487-8. (2) Summary of Product Characteristics - Atrovent UDVs®. Boehringer Ingelheim Ltd. Accessed via: http://www.medicines.org.uk/EMC/medicine/2797/SPC/Atrovent+UDVs/ on 26 Jan 2012 [Date of revision of text July 2011]. (3) Summary of Product Characteristics - Pulmicort Respules®. AstraZeneca UK Ltd. Accessed via: http://www.medicines.org.uk/EMC/medicine/2471/SPC/Pulmicort+Respules+0.5mg+%26+1mg +Nebuliser+Suspension/ on 26 Jan 2012 [Date of revision of text 21 July 2009] (4) Data on File, Allen & Hanbury’s (PCN102). Obtained June 2005. (5) Roberts GW and Rossi SOP. Compatibility of nebuliser solutions. Aust J Hosp Pharm 1993; 23: 35-7. (6) McKenzie JE and Cruz-Rivera M. Compatibility of budesonide inhalation suspension with four nebulizing solutions. Ann Pharmacother 2004; 38: 967-72. (7) Kamin W, Scwabe A, Krämer I. Inhalation solutions – which ones are allowed to be mixed? Physico-chemical compatibility of drug solutions in nebulizers. J Cyst Fibros 2006; 205-13. (8) Burchett DK, Darko W, Zahra J, et al. Mixing and compatibility guide for commonly used aerosolized medications. Am J Health-Syst Pharm 2010; 67: 227-30. (9) Harriman A-M, Purcell N, Fleming S, et al. Can we mix nebuliser solutions? Stability of drug admixtures in solutions for nebulisation. Pharm Prac 1996; Oct: 347-8. Available through NICE Evidence Search at www.evidence.nhs.uk 2 Medicines Q&As (10) Gibbs KP, Cripps D. Asthma. In: Walker R and Whittlesea C. Clinical Pharmacy and Therapeutics. 4th ed. Edinburgh. Churchill Livingstone. 2007; p381. (11) Department of Health. Mixing of Medicines prior to administration in clinical practice: medical and non-medical prescribing. May 2010. [cited 2012 February 24] Available from http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digi talasset/dh_116360.pdf Quality Assurance Prepared by Anna Burgess, Welsh Medicines Information Centre, University Hospital of Wales (based on earlier work by Gail Woodland) Date Prepared 31 January 2012 Checked by Gail Woodland, Welsh Medicines Information Centre, University Hospital of Wales Date of check 24 February 2012 Search strategy Embase (“[fluticasone.exp OR salbutamol.exp OR ipriatropium bromide.exp OR budesonide.exp OR terbutaline.exp OR colistin.exp] AND [drug incompatibility.exp OR drug combination.exp OR drug compatibility.mp] AND [inhalational drug administration.exp OR nebulisation.exp]” Limit: yr=2009-current, human) Medline (“[fluticasone.mp OR ipratropium.exp OR budesonide.exp OR colistin.exp OR terbutaline.exp OR albuterol.exp] AND administration, inhalation AND [drug incompatibility.exp OR drug combinations.exp OR drug compatibility.mp]” Limit yr=2009-current, human) IDIS (Drug(s): ("albuterol 12120066" ) or ("budesonide 84060022") or ("fluticasone 68040094") or ("fluticasone furoate 68040020") or ("terbutaline 12120094") or ("ipratropium bromide 12080028") or ("colistin 8122889") and Descriptors: ("incompatibility physical 33" or "incompatibility chemical 34" ) and "adm inhalation 98". Limit Years 2009-2012) In-house database (MiDatabank) Micromedex (DrugDex, Martindale) Electronic Medicines Compendium NeLM (nebulis* AND incompatibil*) BNF Available through NICE Evidence Search at www.evidence.nhs.uk 3