- Royal College of Paediatrics and Child Health
advertisement

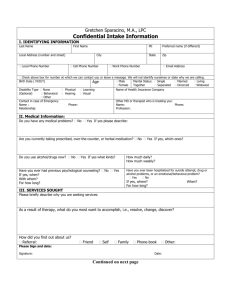
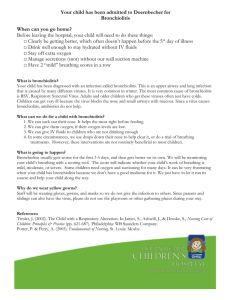
Bronchiolitis guideline – Nsambya Hospital Background: Bronchiolitis is infant disease caused by inflammation of the small airways. It is characterized by wheeze, respiratory distress and crepitations and mild fever. It is often precipitated by a flu-like illness. There is a viral aetiology: RSV is the most common but also influenza, parainfluenza, adenovirus, metapneumovirus have been found. There is some co-infection with mycoplasma pneumoniae but secondary bacterial infection is less common. Usually presents between 2 months and 1 year. Peak severity is at 3-5 days of illness. Pathology is airways obstruction causing areas of hyperinflation and atelectasis with a resultant ventilation perfusion mismatch. Patients with high risk of severe disease: -Prematurity -Congenital heart disease -Chronic respiratory conditions eg chronic lung disease) -Neurological conditions (eg cerebral palsy) -Immunodeficiency Categories of severity: Information to be taken from history: presence of runny nose, fever, cough, difficulty breathing, change in feeding pattern, vomiting, lethargy. Mild (can be managed at home) Moderate (admit to ward) Severe (admit to ward) -Cough -No oxygen requirement -Able to take at least 50% of normal feeds -No tachypnea -Tachycardia -RR >50 -Recessions, head nodding, nasal flare -unable to feed -lethargic -cyanosis despite oxygen therapy -decreased GCS -rising pCO2 Examination also to look at hydration status, neurological condition of child. Investigations: CBC Urea and electrolytes if on long term IV fluids. (CXR, blood cultures, blood gas not routinely required unless deterioration) Initial management: Supportive care is mainstay of treatment: 1. Oxygen if required, keep saturations >92%, humidified oxygen via nasal cannula or facemask. 2. Feeding support: Encourage breastfeeding or bottle feeding if mild and able to manage at home – encourage small frequent feeds. May require NG feeds or IV fluids (isotonic fluids eg Ringers Lactate) depending on level of respiratory distress. 3. Limit fluids to 75% maintenance in the acute phase as there is a high chance of SIADH 4. Admit to paediatric inpatient if there is an oxygen requirement or feeding significantly decreased. 5. Close observations 2-4hourly – be aware of apneas. 6. Isolation recommended 7. Anti pyretic 8. If being managed from home, advise parents to watch for signs of deterioration (apneas, cyanosis, respiratory distress, decreased feeding) Other therapies that can be tried– but do not persist if there is no improvement: 1. 0.9% saline nebuliser (4 hourly) 2. Hypertonic 3% saline nebuliser (3mls 4 hourly – be aware of bronchospasm and consider using with 1.25mcg salbutamol neb) 3. Salbutamol nebuliser 2.5mg (4 hourly) 4. Ipratropium bromide nebulizer 125mcg (6 hourly) 5. Adrenaline nebulizer 0.5mls/kg (1:10,000) – max 5mls 6. Consider antibiotics if there is a neutrophilia and child is not improving after initial therapy (review after 48 hrs). On going deterioration: 1. Consider bubble CPAP 2. Consider intubation if ongoing lethargy/significant distress/apneas if there is a means of transfer to a intensive care setting 3. Always remember to consider alternative diagnosis in a severely unwell child (asthma, pneumonia, infection in immunocompromised child, congenital heart disease, vascular ring, aspiration, foreign body aspiration) Adapted from St Mary’s Hospital, London PICU guidelines, Royal Melbourne Children’s Hospital Guidelines, Recent Advances in Management of Bronchiolitis, Verma et al, Journal of Indian Paediatrics. Dr Yuheng Zhou Nov 2014