UPDATE ON THE AUTISM INSURANCE MANDATE
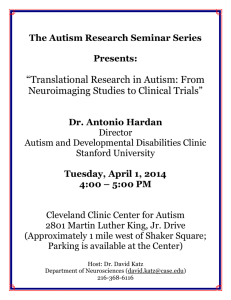
advertisement

UPDATE ON THE AUTISM INSURANCE MANDATE Submitted by Jan Stevens, OTR Wisconsin has a new insurance benefit for children with Autism. The mandate became effective November 1, 2009, with the provision that insurers would implement the coverage as policies renewed or, in the case of collective bargaining agreements, when the agreement is either renewed or expires. The final rule was put in place October 1, 2010, describing covered services and what training is required of the providers. To obtain a copy of the full text of the rule, go to http://oci.wi.gov/ocirules.htm. The mandate is in place for insurance plans over fifty (50) employees, self-insured health plans sponsored by the state, county, city, town, village or school district to cover certain services for children with the autism spectrum disorder. Occupational therapists and speech pathologists may provide therapy in both intensive and nonintensive. The therapists must be licensed in the State of Wisconsin. Some payers are requiring an attestation form stating that the therapist meets the qualifications of the rule. Forms for Arise, WPS, Anthem and Dean are attached. Please contact the insurers that you bill to request the form if necessary. Therapists may be required to be in the payer network. Coverage Includes Intensive and Non-Intensive Services Intensive Level Services (2-9 years old): If a child is receiving intensive behavioral services, the therapist must coordinate their treatment plan with the intensive treatment plan and document coordination of services ongoing. A release of information must be in place. Non-Intensive Services (over 9 years old): Same as any outpatient. The autism benefit coverage is outside of the rehabilitation benefit (i.e. UHC 20 visit limit). If a child is being seen for anything other than autism, i.e. hand surgery, botox, or other physical issues, the autism diagnosis should not be used and services are covered under the rehab benefit. ICD-9 Codes for Autism Use the Same Code for Diagnosis and Treatment 299 codes need 5th digit The basic code will be 299.00 (autism disorder unspecified) Other 299.00 – 299.91 codes can be used if more explicit on the physician order Families may have a large deductible or co-pays. If the child has Medical Assistance, it is recommended that you complete a prior authorization. You must have a denied PA on file in order to bill the family. Please check with the payer if they cover 97533 (Sensory Integration) and 97353 (Self-care Training). Some payers do not cover these codes. It may be helpful to ask these questions: Is this a self-funded plan? (Self-funded plans are not mandated to cover autism) Does your company have the autism mandate in place? (If the plan is outside of Wisconsin, the insurance company must still comply). If they say “no”, ask if they have less than fifty (50) employees which makes them exempt. Ask if services will be covered in the home as well as in the clinic Ask if codes 97530 – 97533 and 97535 will be covered. It is recommended that you request the autism report from the family confirming the autism diagnosis. Diagnosis of Autism must be made by the following: Psychiatrist Psychologist Behavior analyst Social worker (certified/licensed to practice psychotherapy) Note: Physician, Pediatrician, etc. order alone is not adequate nor is school report. For additional information, visit these websites: Frequently Asked Questions on Mandated Coverage for Autism Services http://oci.wi.gov/rules/faq_autism.pdf Frequently Asked Questions About How the Autism Insurance Mandate Affects Children Participating in the CLTS Waivers http://www.dhs.wisconsin.gov/bdds/clts/autism/autismfaq.htm Please contact me at jstevens@rehabresourcesinc.net if you have further questions. 2