Supplementary Information (doc 57K)
advertisement

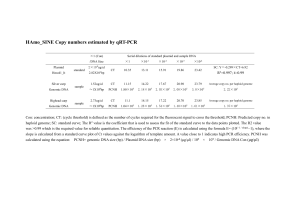
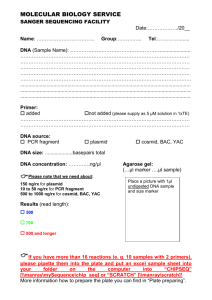
Titles and legends to figures Figure 1 - PIP-São Paulo microdeletion at 7q34 detected by array-CGH in cancer patients. Array-CGH profile of a chromosome region at 7q34 (microarray platform Agilent 180K - Agilent Technologies, Santa Clara, USA), showing heterozygous losses of a similar genomic segment (green bars) (image adapted from the Genomic Workbench software, Agilent Technologies): A – Patient 1; B – Patient 2; C – Patient 3; D – Patient 4, and E – Y87 (TP53 mutated patient who was not part of the cohorts). In the chromosome 7 ideogram, the red bar marks the microdeletion area, which is showed in detail underneath. The deleted segment (solid green bar) is shown in the context of the genomic region. UCSC genes are also represented (figure adapted from UCSC Genome Bioinformatics, http://genome.ucsc.edu, GRCh37). Supplementary Figure 1 – Data on PIP-São Paulo microdeletion. A. Eletropherogram of a PCR fragment amplified in the patients (primers F-CCAGATCCAGGAGATAATC and R-GGTATGGTGTATGATAAAGG). Arrow indicates the breakpoints’ junction. Genomic positions near the breakpoints are displayed. B. 64bp genomic sequence encompassing the junction fragment of the PIP-São Paulo deletion. In red, last bases adjacent to the breakpoints; in black, the sequence of the rearranged fragment with the grey box indicating the junction; the deleted sequences adjacent to the breakpoints are shown in grey letters. C. PCR fragment from the 7q34 microdeletion bridging the 69 kb gap in selected tumor samples from patients. Samples 1-10 (Standard PCR): 1: negative control for the microdeletion; 2: positive control for the microdeletion; 3-6: positive results from 4 different adenomas from the patient 4 with FAP; 7-9, positive results from (in order) adenoma, adenocarcinoma and metastasis from patient 5 with multiple tumors; 10: no template control. Samples 11-17(Booster PCR): 11-13 results from (in order) basal cell carcinoma and two different sections of the breast carcinoma from patient 6 with multiple tumors; 14-15 results from (in order) dermatofibroma; and schwanoma from patient 7 with multiple tumors. 16: positive control for the microdeletion; 17: no template control. Supplemental Material 1 MATERIAL AND METHODS Subjects The initial sample of this study was based on patient cohorts for familial and pediatric cancer, exhibiting an increased cancer predisposition. All 123 subjects were seen at the AC Camargo Hospital, São Paulo, Brazil and the research protocol approved by the ethics committee of the same institution. The first cohort comprised 70 probands from unrelated families selected for matching either “classic” Li–Fraumeni Syndrome (LFS), (OMIM #151623) or Li-Fraumeni Like (LFL) criteria1-4 that showed no mutations in TP53 gene. The second cohort consisted of 50 patients manifesting various types of pediatric cancer (<18 years age). The third cohort was composed of 3 probands from families clinically diagnosed as classical or attenuated Familial Adenomatose Poliposis (FAP/AFAP), with no mutations in the APC or MUTYH genes (Torrezan et al, in preparation). No other criteria except the date of diagnosis and informed consent to participate were used. As control, a Brazilian group of 260 non-related subjects was used: 100 healthy individuals, and 116 unrelated relatives from patients with idiopathic mental retardation, (maximally one per family), unselected regarding familial history of cancer. The replication sample of patients was composed under similar criteria to the initial sample of increased cancer predisposition. The replication sample consisted of 166 non-related individuals that had presented with more than one tumor (multiple tumors) prior to 60 years of age, and 53 probands of hereditary melanoma families with no mutations in the CDKN2A and CDK4 genes. All subjects were seen at the AC Camargo Hospital, São Paulo, Brazil. A second control group consisted of 847 persons with no history of cancer and was used as controls in the replication study. Array-CGH DNA from patients and controls was obtained from peripheral blood. Investigation of copy number changes was performed by array-CGH using the whole genome Agilent Sure Print G3 Human CGH Microarray (Agilent Technologies, Santa Clara, USA) containing ~180.000 oligonucleotides. Briefly, samples were labeled with Cy3- and Cy5-dCTPs by random priming; purification, hybridization, and washing were carried out as recommended by the manufacturer. Scanned images of the arrays were processed and analyzed using Feature Extraction and Genomic Workbench software (both from Agilent Technologies), using the statistical algorithm ADM-2 and a sensitivity threshold of 6.7. We used two reversed labeled hybridizations for each sample. Gains or losses in copy number were accepted when the log2 ratio of the Cy3/Cy5 intensities of a given genomic segment was > 0.6 or < -0.8, respectively, and where putative alterations encompassed at least three consecutive probes; any alterations not detected in both dye-swap experiments were disregarded. All detected imbalances were compared to CNVs reported in the Database of Genomic Variants (DGV; http://projects.tcag.ca/variation/ - freeze of March, 2011), and to data from our own group. Copy number variation by Real time PCR Copy number determinations were carried out for selected targets (PIP and TAS2R39 genes) using TaqMan Gene Copy Number Assays (Applied Biosystems, Foster City, CA). All assays were conducted in 96-well plates (MicroAmpOptical 96-Well Reaction Plate, Applied Biosystems, Foster City, CA). Each well contained FAM-labeled TaqMan probe for either PIP (Hs01602128_cn) or TAS2R39 (Hs00679076_cn) and VIC-labeled TaqMan probe for the reference gene (RNaseP) (4403326). As the reference sample or calibrator, we used commercial human genomic DNA (Promega, Madison, WI). Real-time data analysis was carried out using the 7500 Real time PCR system (Applied Biosystem, Foster City, CA). The relative number of DNA copies for each probe was determined by the DDCt ((FAM Ct - VIC Ct) sample - (FAM Ct – VIC Ct) calibrator) method, which assumes that the calibrator DNA has two copies of the reference gene. Results were analyzed using CopyCaller v 1.0 software (Applied Biosystem, Foster City, CA). Assessment of PIP-São Paulo deletion in blood DNA Briefly, the PCR mixture consisted of 12.5μl of GoTaq Colorless Master Mix (Promega, Madison, WI), 250 ng of DNA and 10 μM of each primer, in a final reaction volume of 25μl. The following cycling parameters were used: initial denaturation at 95ºC for 5 min followed by 35 cycles of denaturation at 95ºC for 30 s; annealing steps at 55ºC for 30 s; and extension at 72ºC for 30 s followed by 72ºC for 6 min (primers F5´CCAGATCCAGGAGATAATC 3´ and R -5´GGTATGGTGTATGATAAAGG 3´). Assessment of PIP-São Paulo deletion in tumor DNA The presence of the PIP-São Paulo was screened by PCR in tumor samples from formalinfixed paraffin-embedded (FFPE) blocks. Tumor-enriched areas of FFPE samples were identified in H&E-stained slides and two core punches (1 mm × 3-5 mm) were taken from the corresponding region of the block. DNA was extracted from FFPE cores using the QIAamp DNA FFPE Tissue Kit (Qiagen, Germantown, MD) according to the manufacturer’s directions. The DNAs quantification was performed with Qubit® dsDNA HS Assay Kit with the Qubit® 2.0 Fluorometer (Invitrogen, Grand Island, NY). Samples that yielded more than a 25 ng of DNA were amplified by regular PCR, while samples that yielded less were amplified with Booster PCR. Briefly, regular PCR reactions consisted of 25 ng of template and 500 nM of each primer (primers PIP2_F-5´ GTCTGCTATCTGAGAGCTTCTT 3´ and PIP2_R-5´ GTTCCACTGGTTGATATGTATG 3´) in a final volume of 20 µl with KAPA2G Fast HotStart ReadyMix (Kapa Biosystems, Woburn, MA). The following cycling parameters were used: initial denaturation at 95ºC for 2 min followed by 40 cycles of denaturation at 95ºC for 18 s; annealing steps at 55ºC for 20 s; and extension at 72ºC for 1 s followed by 72ºC for 3 min. Booster PCR was performed with the same primer pair and cycles parameters described above and consisted of 2 steps: 1) 3 to 7.5 ng of template were amplified for 20 cycles with 0.25 nM of each primer in a final volume of 20 µl with KAPA2G Fast HotStart ReadyMix; 2) 200 nM of each primer were diluted in 3 µl of KAPA2G Fast HotStart ReadyMix, added in the reaction from step one and amplified for more 50 cycles. DNA sequencing PCR products were purified with exonuclease I and alkaline phosphatase (EXO-SAP ITUSB/GE, SP, Brazil) and sequenced in both directions. DNA sequence was determined on an ABI Prism 3130 (Applied Biosystems, Foster City, CA) and analyzed using CLC Bio software. SNP typing Affymetrix Human Mapping 500 K array sets (Affymetrix Inc, Santa Clara, CA) consisting of two chips (Sty and Nsp) with ~250 000 SNPs each, were used in combination with the Genotyping Console 4.0 (GTC 4.0). The SNPs in predefined genomic regions were genotyped based on the BRLMM algorithm exhibiting scores above the quality control (QC) threshold. DNA denaturation, labeling, hybridization, and scanning were performed according to the manufacture’s protocols (http://www.affymetrix.com) using an Affymetrix Fluidics Station 450, Affymetrix Hybridization Oven 640 and Affymetrix GeneChip Scanner 3000. Statistics The statistics software packet IBM SPSS 19 was used to determine the significance of differences in PIP-São Paulo deletion frequencies between patients and controls using the Fisher exact test (two sided); this demonstrate that the differences in PIP deletion frequency between the pooled controls and patients were significant at the 0.05 level. A chi2 test of homogeneity for deletion frequency between the first and replicate samples of the patients and controls respectively, demonstrated that there were no significant differences at the 0.05 level. References 1. Li FP, Fraumeni JF, Mulvihill JJ et al: A cancer family syndrome in twenty-four kindreds. Cancer Res 1988; 48: 5358-5362. 2. Eeles RA: Germline mutations in the TP53 gene. Cancer Surv 1995; 25: 101-124. 3. Birch JM, Heighway J, Teare MD et al: Linkage studies in a Li-Fraumeni family with increased expression of p53 protein but no germline mutation in p53. Br J Cancer 1994; 70: 1176-1181. 4. Tinat J, Bougeard G, Baert-Desurmont S et al: 2009 version of the Chompret criteria for Li Fraumeni syndrome. J Clin Oncol 2009; 27: e108-109; author reply e110.