ю ° T Р яяяяяяяя Й) 8. . . " 8. 8. 8. PА а=Р/ Р Р
advertisement
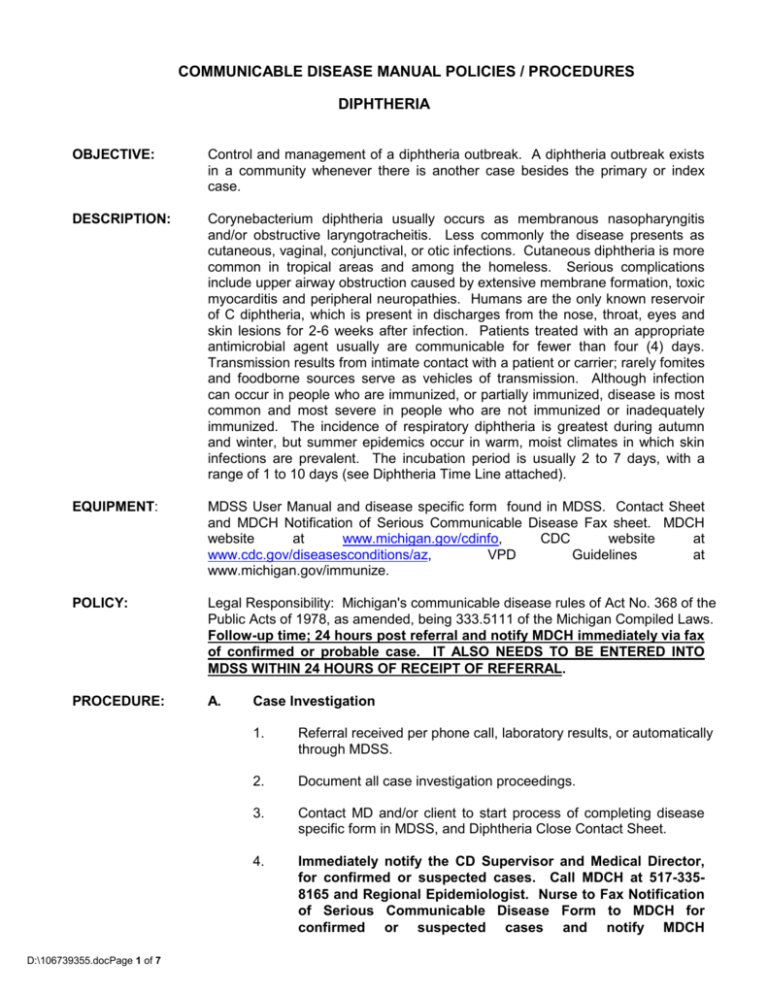
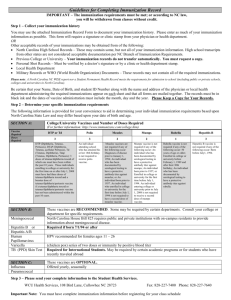
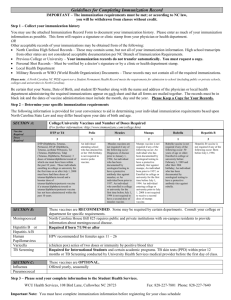
COMMUNICABLE DISEASE MANUAL POLICIES / PROCEDURES DIPHTHERIA OBJECTIVE: Control and management of a diphtheria outbreak. A diphtheria outbreak exists in a community whenever there is another case besides the primary or index case. DESCRIPTION: Corynebacterium diphtheria usually occurs as membranous nasopharyngitis and/or obstructive laryngotracheitis. Less commonly the disease presents as cutaneous, vaginal, conjunctival, or otic infections. Cutaneous diphtheria is more common in tropical areas and among the homeless. Serious complications include upper airway obstruction caused by extensive membrane formation, toxic myocarditis and peripheral neuropathies. Humans are the only known reservoir of C diphtheria, which is present in discharges from the nose, throat, eyes and skin lesions for 2-6 weeks after infection. Patients treated with an appropriate antimicrobial agent usually are communicable for fewer than four (4) days. Transmission results from intimate contact with a patient or carrier; rarely fomites and foodborne sources serve as vehicles of transmission. Although infection can occur in people who are immunized, or partially immunized, disease is most common and most severe in people who are not immunized or inadequately immunized. The incidence of respiratory diphtheria is greatest during autumn and winter, but summer epidemics occur in warm, moist climates in which skin infections are prevalent. The incubation period is usually 2 to 7 days, with a range of 1 to 10 days (see Diphtheria Time Line attached). EQUIPMENT: MDSS User Manual and disease specific form found in MDSS. Contact Sheet and MDCH Notification of Serious Communicable Disease Fax sheet. MDCH website at www.michigan.gov/cdinfo, CDC website at www.cdc.gov/diseasesconditions/az, VPD Guidelines at www.michigan.gov/immunize. POLICY: Legal Responsibility: Michigan's communicable disease rules of Act No. 368 of the Public Acts of 1978, as amended, being 333.5111 of the Michigan Compiled Laws. Follow-up time; 24 hours post referral and notify MDCH immediately via fax of confirmed or probable case. IT ALSO NEEDS TO BE ENTERED INTO MDSS WITHIN 24 HOURS OF RECEIPT OF REFERRAL. PROCEDURE: A. D:\106739355.docPage 1 of 7 Case Investigation 1. Referral received per phone call, laboratory results, or automatically through MDSS. 2. Document all case investigation proceedings. 3. Contact MD and/or client to start process of completing disease specific form in MDSS, and Diphtheria Close Contact Sheet. 4. Immediately notify the CD Supervisor and Medical Director, for confirmed or suspected cases. Call MDCH at 517-3358165 and Regional Epidemiologist. Nurse to Fax Notification of Serious Communicable Disease Form to MDCH for confirmed or suspected cases and notify MDCH Immunization Division Vaccine-Preventable Disease (VPD) Surveillance Coordinator at 517-335-8159. 5. B. If outbreak, or one (1) probable or confirmed case, notify CD Supervisor who will then report to Medical Director and State Health Department as necessary. Case Classification Clinical Case Definition: An upper-respiratory tract illness characterized by sore throat, low-grade fever, and an adherent membrane of the tonsil(s), pharynx, and/or nose. Case Classification: Probable: A clinically compatible case that is not laboratory confirmed and is not epidemiologically-linked to a laboratoryconfirmed case. Confirmed: A clinically compatible case that is either laboratory confirmed or epidemiologically-linked to a laboratory-confirmed case. Comment: Respiratory disease caused by nontoxigenic Corynebacterium diphtheriae should be reported as diphtheria. Cutaneous diphtheria should not be reported. All diphtheria isolates, regardless of association with disease, should be sent to the Diphtheria Laboratory National Center for Infectious Diseases, CDC. Arrangements should be made through the MDCH laboratory. Note: On rare occasions, respiratory diphtheria may result from infection with other Corynebacterium species (C. ulcerans or C. pseudotuberculosis). These isolates should also be forwarded to the CDC. C. Lab Criteria for Diagnosis. 1. MDCH accepts only isolation of Corynebacterium diphtheriae from a clinical specimen from a culture and PCR, or 2. Histopathologic diagnosis of diphtheria. 3. Guidelines for Collection of Specimens for Isolation of C. diphtheriae (source: World Health Organization [WHO]). Throat Swabs D:\106739355.docPage 2 of 7 Pharynx should be clearly visible and well illuminated. Depress tongue with an applicator and swab the throat without touching the tongue or inside of the cheek. Rub vigorously over any membrane, white spots, or inflamed areas; slight pressure with a rotating movement must be applied to the swab. If any membrane is present, lift the edge and swab beneath it to reach the deeply embedded organisms. Nasopharyngeal Specimens Insert the swab into the nose through one nostril beyond the anterior nares. Gently introduce the swab along the floor of the nasal cavity, under the middle turbinate until the pharyngeal wall is reached. Force must not be used to overcome any obstruction. Skin Diphtheria and Other Lesions D. E. Lesions should be cleansed with sterile normal saline and crusted material removed. Press the swab firmly into the lesion. 4. Diphtheria testing may not be available in most clinical laboratories. Contact MDCH Microbiology Laboratory (517-3358067) and MDCH VPD Surveillance Coordinator (517-335-8159) for further direction. Immunity/Susceptibility 1. Lifelong immunity is usually, but not always acquired after disease or inapparent infection. 2. Immunization with toxoid produces prolonged, but not lifelong, immunity. 3. Serosurveys in the U.S. indicate that 40 percent of adults lack protective levels of circulating antitoxin. 4. Antitoxin immunity protects against systemic disease, but not colonization in the nasopharynx. Control Measures 1. D:\106739355.docPage 3 of 7 Patient related measures: Reports of suspect diphtheria should be investigated immediately. Suspect cases should be reported promptly by telephone to MDCH VPD Surveillance Coordinator so that arrangements can be made to obtain diphtheria antitoxin for the patient from CDC and the MDCH Laboratory can be notified to set up for cultures. Contact information: MDCH VPD Surveillance Coordinator 517-335-8159 MDCH Communicable Disease Epidemiology Office 517-335-8165 CDC Consultation (National Immunization Program) 404-639-8257 CDC after-hours: 770-488-7100 or 404-639-2888 or 404-639-2889 MDCH Laboratory: 517-335-8067 D:\106739355.docPage 4 of 7 The patient should be placed in strict isolation, which should be maintained until elimination of the organism is demonstrated by negative cultures of two samples obtained at least 24 hours apart after completion of antimicrobial therapy. Obtain both nasal and pharyngeal swabs for culture, if this has not yet been done, to confirm the diagnosis. Ideally these should be collected prior to initiation of antibiotic treatment. Obtain serum for serology studies of antibodies to diphtheria toxin. Obtain, if possible, a consultation from an Infectious Disease physician on the patient; consider treatment with diphtheria antitoxin in consultation with MDCH and CDC authorities. Begin/assure antimicrobial therapy (antimicrobial therapy is not a substitute for antitoxin treatment). Antimicrobial therapy is recommended until patient can swallow comfortably. Administer/assure active immunization with diphtheria toxoid during convalescence, because clinical diphtheria does not necessarily confer immunity. Obtain repeat nasal and pharyngeal specimens for culture a minimum of two (2) weeks after completion of antimicrobial treatment to assure eradication of the organism. Persons who continue to harbor the organism after treatment with either penicillin or erythromycin should receive an additional 10-day course of oral erythromycin and should submit samples for follow-up cultures. 2. Contact Management: Management is based on individual circumstances, including immunization status and the likelihood of surveillance and adherence to prophylaxis. Identify close contacts: Household members Persons with a history of direct contact with a casepatient (e.g., caretakers, relatives, or friends who regularly visit the home); Medical staff exposed to case-patient’s oral or respiratory secretions. Assess and monitor contacts for signs and symptoms for diphtheria for at least seven (7) days. Obtain nasal and pharyngeal swab specimens from all contacts for C. diphtheriae cultures irrespective of their immunization status. Administer/assure antimicrobial prophylaxis for contacts. Use the Diphtheria Close Contact Sheet for recording contacts and their antibiotic prophylaxis. Recommended prophylaxis: A single dose of intramuscular benzathine penicillin G (600,000 units for persons < six (6) years of age and 1.2 million units for persons > six (6) years of age). OR A 7- to 10-day course of oral erythromycin (40 mg/[kg/d]) for children and 1 g/d for adults. Contacts who cannot be kept under surveillance should receive: Benzathine penicillin G, but not erythromycin for reasons of compliance. An initial dose of DTaP, Tdap, DT or Td, depending on age and the person’s immunization history. Cultures done before and after prophylaxis. Assess diphtheria toxoid (DPT, DTaP, Tdap, DT, or Td) vaccination history status of Asymptomatic contacts: D:\106739355.docPage 5 of 7 If < three (3) doses: Administer immediate dose of diphtheria toxoid and complete primary series according to schedule. F. D:\106739355.docPage 6 of 7 If > three (3) doses with last dose > five (5) years ago: Administer immediate booster dose of diphtheria toxoid. If > three (3) doses with last dose < five (5) years ago: Children in need of their fourth primary dose. Adult contacts whose occupations involve handling food, especially raw milk, or close association with nonimmunized children, should be excluded from work until bacteriologic exam proves them not to be carriers. Active immunization against diphtheria should be undertaken during convalescence from diphtheria in every patient because this exotoxin - mediated disease does not necessarily confer immunity. Upon orders of Supervisor and/or Medical Director, the following should be done: Record search of preschool, day care center and school to determine who has not had adequate doses of DPT/DT/Td for age. EXCLUDE FROM SCHOOL all students not vaccinated adequately. May re-enter school if proof provided of adequate vaccination. If they are not vaccinated (per waiver or non-compliance), wait until 14 days after date of onset of last reported case. Health Department to provide clinic for all students who need vaccination. Educate contacts regarding period of communicability, incubation period, spread and treatment. An excellent Question and Answer Diphtheria Information Sheet from the Immunization Action Coalition is located with your Fact Sheets in this policy. In the event of death, obtain and send copies of hospital discharge summary, death certificate, and autopsy report to MDCH Immunization Division. MDSS Case Reporting: 1. Complete case investigation using disease specific form in MDSS. 2. Notify CD Supervisor that the case report is ready for review. PHN will be notified if corrections are needed prior to closing case in MDSS. 3. REFERENCES: D:\106739355.docPage 7 of 7 CD Supervisor reviews case for completeness and closes MDSS case report. Current Epidemiology and Prevention of Vaccine-Preventable Diseases (pink book) Current Red Book Current Control of Communicable Diseases Manual Current disease specific “Fact Sheet” Websites: www.cdc.gov/diseasesconditions/az/a.html www.michigan.gov/cdinfo www.michigan.gov/immunize (VPD Guidelines)