DURA-SUP - California State University, Long Beach
advertisement

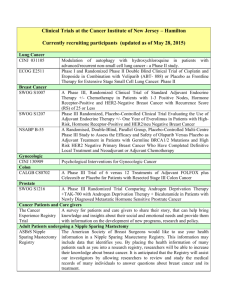
A DISSENTING VIEW ON PRIORITIES IN ADJUVANT THERAPY FOR BREAST CANCER May 16, 1998 prepared by Michael J. Halliwell, Ph.D. California State University Long Beach CA 90840 Home address: 2930 Colorado Ave. # D-18 Santa Monica, CA 90404-3647 Home phone: 310-829-2821 Home fax: 310-828-9174 UNSETTLING ASPECTS OF A "SETTLED" CONSENSUS Sometimes cancer a treatment prevailing is so well consensus on established an aspect that it of breast requires no footnoting in an otherwise well documented review of the state of our knowledge. Thus Dr. Hortobagyi's introduces CONTROVERSIES IN THE MANAGEMENT OF EARLY-STAGE BREAST CANCER by stating: It has been established that . . . four to six cycles of a single combination are as effective as longer durations of treatment. Id. at 129. With the benefit of adjuvant chemotherapy thus circumscribed, there is no mention of any potential gains from the more extensive use of cytotoxic drugs in the defining goals for Session E6, which urge oncologists to move in the opposite direction: At the conclusion of this session, the participant should be able to. . . .determine what subgroups of patients with early breast cancer do not require adjuvant systemic therapies. However, there are very few invasive breast cancers which are so unlikely to relapse that the popular regimens of chemotherapy (such as CMF) carry a greater mortality risk. This is especially true for premenopausal women who are in generally good health and whose breast cancers account for most of the years of life lost to this disease. The recent publication patients (which shows that in Lancet of a study tamoxifen is very of 37,000 effective in postponing breast cancer relapses in premenopausal women) means that once any surge in micrometastatic growth has been halted, it is safe to spread out chemotherapy to the point where it can be tolerated indefinitely by normal tissues. 1 GAINS FROM LONGER CHEMOTHERAPY ARE LARGER FOR LESS ADVANCED TUMORS In these comparisons, Ontario study results are from Table 4 at 1221 of Levine et al (1990), and SECSG study results are from Tables 2 and 3 at 276-277 of Velez-Garcia et al (1984). ONTARIO STUDY: 36 MONTH RELAPSE-FREE SURVIVAL IN WOMEN UNDER 50 36 WEEK REGIMEN Patients RFS 12 WEEK REGIMEN Patients RFS Long-Short Prob. Any Nodes 89 72% 89 54% + 18% .002 1-3 Nodes 55 84% 56 59% + 25% .002 SECSG STUDY: 42 MONTH RELAPSE-FREE SURVIVAL IN PREMENOPAUSAL WOMEN 12 MONTH REGIMEN Patients RFS 6 MONTH REGIMEN Patients RFS Long-Short Prob. 1-3 Nodes 42 93% 58 78% + 15% .047 1 Node 18 100% 29 76% + 24% .034 In the Milan II study, intention-to-treat analysis is used even though there are three times as many dropouts in the 12-month arm, and in the longer-treatment group 21% fewer of the patients completing therapy received at least 85% of the prescribed dosage (Tancini et al, 1979 at 286; Bonadonna et al, 1985b at 98). Table 6 at 440 Bonadonna et al (1981) and Table 3 at 98 of Bonadonna et al (1985) produce a relationship free of most of this dosage bias: MILAN STUDY: 48 MONTH RELAPSE-FREE SURVIVAL IN PREMENOPAUSAL WOMEN 12 MONTH REGIMEN > 85% Dose Patients RFS 6 MONTH REGIMEN Patients RFS Long-Short Prob. Any Nodes 30 80.0% 66 66.7% +13.3% .046 1-3 Nodes 18 88.9% 39 69.3% +19.6% .030 These advantages can be extended with tamoxifen or raloxifene. 2 EXTENDED CHEMOTHERAPY HELPS HOST DEFENSES DELAY TUMOR RECURRENCES Demichelli et al (1996) analyze Milan Tumor Institute data: A total of 1173 patients treated between 1964 and 1980 with mastectomy alone and no adjuvant therapy were studied. The hazard function for first failure presented an early peak at about 18 months after surgery, a second peak at about 60 months and then a tapered plateau-like tail extending up to 15 years. Relapse can take place at the local-regional level when the body tumor burden is low and the capacity of host defenses has yet reached the breaking point. However, there is a very noticeable "dam burst" effect in the case of distant metastases, as their Figure 4 shows. Senn and Barett-Mahler (1987) discuss how a short regimen of chemotherapy affects breast cancer recurrence in a Swiss study: While node-negative women experienced an impressive RelapseFree Survival gain during the first 3-4 years, this advantage was vanishing thereafter at 5 and more years of median follow-up (figure 3a). The strange accumulation of relapses among our chemotherapy patients at 4-5 years favors the idea of testing "late adjuvant reinduction regimens" (Speer et al, 1984) in present day trials such as International Breast Cancer Study Group Trial VI (Goldhirsch and Gelber, 1987). Id. at 244. When the Vienna study used much longer chemotherapy, Jakesz et al (1987) found that the relapse curve was greatly pushed back: Our results are comparable with those from Osako at the same observation period (Senn et al (1986). Interestingly this trial reported at 4-5 years of median follow-up an accumulation of late relapses among the chemoimmunotherapy group. Whether or not our concept of delivering chemotherapy over 3 years is the reason why we did not observe these late re-currences has to remain speculative. There is, however, theoretical reason to believe that late periodic adjuvant consolidation cycles could be of some benefit (Speer et al (1984). Id. at 230. 3 OPPORTUNITIES AND RISKS ASSOCIATED WITH PREMENOPAUSAL MAMMOGRAPHY The increasing utilization of mammographic screening by women in their 40's will catch many breast cancers at an earlier stage, where longer chemotherapy is most advantageous. However, when a breast into tumor is shifted by earlier detection the node- negative category, there is a serious risk if this causes one to withhold adjuvant documented a chemotherapy. shortening of Simpson-Herren lifespans in murine et al tumor (1976) implant experiments, which are linked with "outbursts of metastatic growth following surgical excision of a primary tumor." Id. at 1753. In the Stockholm trial, Frisell et al (1991) report a small medium-term increase in breast cancer deaths in 40-49 year-old screened patients, but a sharp increase in the years just after tumor removal: Of the women under 50, 16 died of breast cancer in the screened population and 8 in the control population. The relative risk was 1.09 (95 percent confidence interval: 0.4-3.0) and no reduction in mortality was found (Table 5). The cumulative number of deaths in this age group is seen in Fig. 6. Id. at 52. These earlier deaths may be caused by a growth surge of metastases in the lungs (whose castoff clumps pass through the heart only once before entering the general circulation). With respect to a similar phenomenon, Simpson-Herren et al (1976) note "the residual tumor foci, stimulated to more rapid growth, should be appropriate targets for adjuvant chemotherapy." Id. at 1749. 4 REFERENCES Bonadonna G, Valagussa P, Rossi A, et al (1981): Multimodal Therapy with CMF in Resectable Breast Cancer with Positive Axillary Nodes -- The Milan Institute Experience. Pp. 435-444 in Adjuvant Therapy of Cancer III (Salmon SE and Jones SE, eds.) Orlando, Grune & Stratton. Bonadonna G, Valagussa P, Rossi A, et al (1985): Ten-Year Experience with CMF-Based Adjuvant Chemotherapy in Resectable Breast Cancer. Breast Cancer Res Treat 5: 95-115. Demicheli R, Abbattista A, Miceli R, Valagussa P, and Bonadonna G (1996): Time Distribution of the Recurrence Risk for Breast Cancer Patients Undergoing Mastectomy: Further Support about the Concept of Tumor Dormancy. Breast Cancer Res Treat 41:177-185. Frisell J, Eklund G, Hellstrom L, Lindbrink E, Rutqvist LE, and Somell A (1991): Randomized Study of Mammography Screening -- Preliminary Report on Mortality in the Stockholm Trial. Breast Cancer Res Treat 18: 49-56. Goldhirsch A and Gelber RD (1987): Adjuvant Therapy for Breast Cancer: The Ludwig Breast Cancer Trials 1987. Pp 297-309 in Adjuvant Therapy of Cancer V (Salmon SE, ed.) Orlando, Grune & Stratton. Jakesz R, Kolb R, Reiner G, et al (1987): Adjuvant Chemotherapy in Node-Negative Breast Cancer Patients. Pp 223-231 in Adjuvant Therapy of Cancer V (Salmon SE, ed.) Orlando, Grune & Stratton. Levine MN, Gent M, Hryniuk WM, et al (1990): A Randomized Trial Comparing 12 Weeks Versus 36 Weeks of Adjuvant Chemotherapy in Stage II Breast Cancer. J Clin Oncol 8: 1217-1225. Senn HJ and Barett-Mahler AR (1987): Update of Swiss Adjuvant Trials with LMF and CMF in Operable Breast Cancer. Pp. 243-252 in Adjuvant Therapy of Cancer V (Salmon SE, ed.) Orlando, Grune & Stratton. Senn HJ, Jungi WF, Amgwerd R, et al (1986): Swiss Adjuvant Trial (OSAKO 06/74) with Chlorambucil, Methotrexate, and 5-Fluorouracil Plus BCG in Node-Negative Breast Cancer Patients: Nine-Year Results. NCI Monographs 1: 129-134. Simpson-Herren L, Sanford AH, and Holmquist JP (1976): Effects of Surgery on the Cell Kinetics of Residual Tumor. Cancer Treat Rep 60: 1749-1760. Speer JF, Petrovsky VE, Retsky MW, and Wardwell RH (1984): A 5 Stochastic Numerical Model of Breast Cancer Growth that Simulates Clinical Data. Cancer Res 44: 4124-4130. Tancini G, Bajetta E, Marchini S, Valagussa P, Bonadonna G, and Veronesi U (1979): Preliminary 3-Year Results of 12 versus 6 Cycles of Surgical Adjuvant CMF in Premenopausal Breast Cancer. Cancer Clin Trials 2: 285-292. Velez-Garcia E, Moore M, Vogel C, et al (1984): Adjuvant Chemotherapy with or without Radiation Therapy in Women with Breast Cancer and Positive Axillary Nodes: The Southeastern Cancer Study Group (SECSG) Experience. Pp. 273-282 in Adjuvant Therapy of Cancer IV (Jones SE and Salmon SE, eds.) Orlando, Grune & Stratton. 6