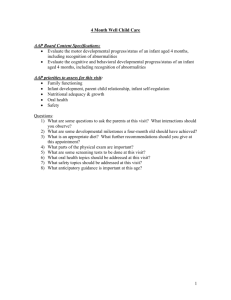
2 Month Well Child Care
advertisement
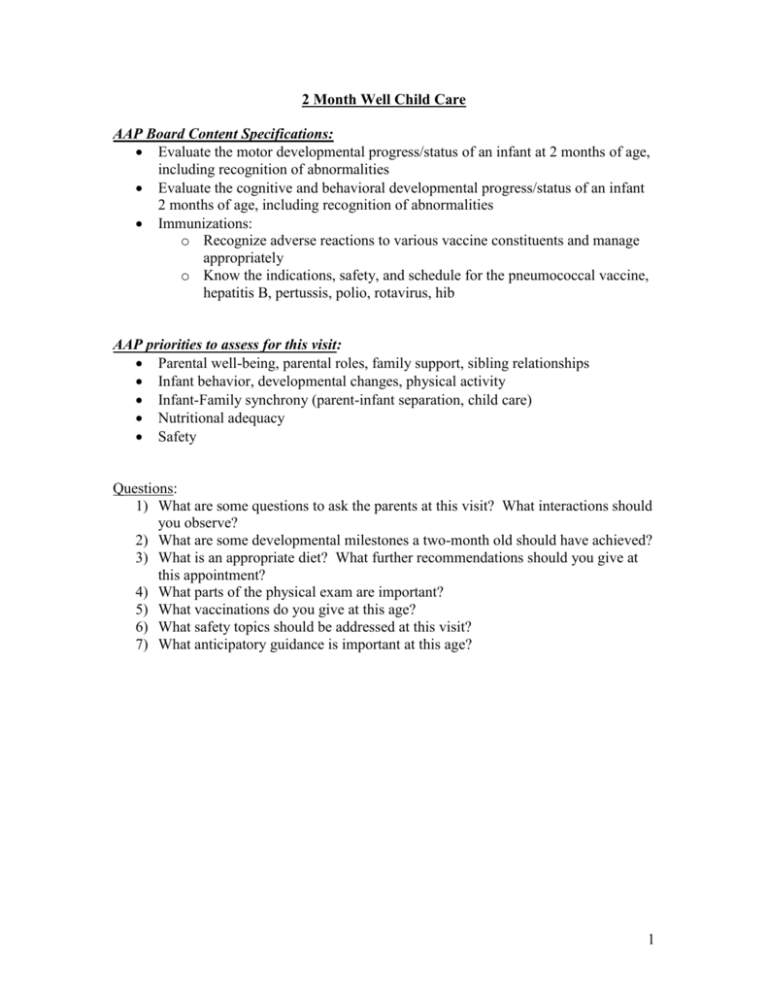
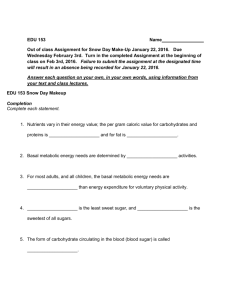
2 Month Well Child Care AAP Board Content Specifications: Evaluate the motor developmental progress/status of an infant at 2 months of age, including recognition of abnormalities Evaluate the cognitive and behavioral developmental progress/status of an infant 2 months of age, including recognition of abnormalities Immunizations: o Recognize adverse reactions to various vaccine constituents and manage appropriately o Know the indications, safety, and schedule for the pneumococcal vaccine, hepatitis B, pertussis, polio, rotavirus, hib AAP priorities to assess for this visit: Parental well-being, parental roles, family support, sibling relationships Infant behavior, developmental changes, physical activity Infant-Family synchrony (parent-infant separation, child care) Nutritional adequacy Safety Questions: 1) What are some questions to ask the parents at this visit? What interactions should you observe? 2) What are some developmental milestones a two-month old should have achieved? 3) What is an appropriate diet? What further recommendations should you give at this appointment? 4) What parts of the physical exam are important? 5) What vaccinations do you give at this age? 6) What safety topics should be addressed at this visit? 7) What anticipatory guidance is important at this age? 1 1) Parent-Child Interaction: Parental Questions? o How are things going? o Maternal post-partum checkup? Depression? o What kind of support system do they have? Parent-Child Interaction o How responsive are the parents and the infant to each other o Do parents appear comfortable with infant and responsive to infant’s distress, comforting, and feeding cues? o Parental roles- Do parents support each other or show signs of disagreement? o Do parents seem anxious, depressed, fatigued, or overwhelmed? 2) Developmental milestones: What to expect for this visit & in the upcoming months Age Gross Motor 2 m/o *Push to prone, holds up chest while prone *Able to hold up head 3 m/o *Partial head lag when pulled from sitting Fine Motor *Hands unfisted 1/2 time *Tracks past midline *Diminishing newborn reflexes *Bats at objects *Sustained palmar grasp Communicative *Indicates boredom (cries/fusses) *Coos *Clearer behaviors to indicate needs *Regards small objects Social *Social smile *Attempts to look at parents *Consoles/comforts self *Echoes speaker *Babbles 3) Diet: At 2 months breastfed infants need about 8-12 feeding in 24 hours. Bottle fed infants take about 21-32 oz in 24 hrs (usually 4-6 oz every 3-5 hrs). Babies only need breast milk or iron-fortified formula in the first 4-6 months of life. Parents should not start solid foods until 4-6 months, when infant is developmentally ready. The only supplement is Vitamin D for exclusively BF babies (Dvisol/Trivisol/Polyvisol) or babies taking under 1L of formula. Avoid honey & cow’s milk o Botulinum spores in honey put an infant under 1 year old at risk for infantile botulism. o Cow’s milk has been shown to increase intestinal blood loss by 30% in infants <1 yr old. Also, higher concentrations of calcium & phosphorous concentrations in cow’s milk, combined with low ascorbic acid leads to low bioavailability of iron. Furthermore, there is a higher solute load puts more strain on the infant’s kidneys. 2 4) Physical Exam: Plot Wt, Ht. and HC; Infants in the first 3 months of life should gain 30gm/day Head: palpate fontanelles, sutures Eyes: red reflex, tracking, watch for fixed eso/exotropia, opacification Mouth: look for thrush CV: listen for murmur, check pulses (including femoral) Abdomen: feel for masses, HSM Musculoskeletal: Perform Barlow and Ortolani maneuvers; look for torticollis Neuro: check tone, strength, symmetry of movements Skin: check for bruises and rashes Growth & Caloric Requirements Age Daily weight gain g/day Monthly weight gain lb/month Monthly Lt cm/month Monthly HC (cm/mo) Recommended Kcal/kg/day Kcal/kg/day 0-3 months 25-35 2 lb 2.6-3.5 2 115 3-6 months 6-12 months 15-21 1.25 lb 1.6-2.5 1 110 10-13 1 lb 1.2-1.7 100 1-3 yrs 4-10 13 oz 0.7-1.1 0.5 0.270.15 4-6 yrs 5-8 8 oz 0.5-0.8 7-10 yrs 5-12 6 oz 5-6 cm/yr 11-18 yrs Varies Catch Up (FTT) Infant: 6090 Child: 30 100 M: 1.5-6cm/6 mo F: 1.5-5cm/6 mo 5) Vaccinations: Pediarix (Dtap, Inactivated Polio, Hepatitis B), Hib, PCV 13, Rotateq Influenza for family members when children <6 months 6) Safety Topics: Remember, BACK TO SLEEP! Discuss other ways to reduce SIDS. 3 Crib slats < 2 3/8 in. (60mm); playpen mesh weave <1/4 in. (6 mm)- never leave baby in a mesh playpen with the drop-side down or in crib with rails down No extra water is required or recommended. Remember, NO BOTTLE PROPPING! Rear- facing car safety seat in back seat for all transportation until 2 y/o Set water heater to 120°; test water before placing infant in bath; never drink hot liquids while holding baby Always monitor baby on changing table, bed, counters, couches-They always learn to roll for the first time when you’re not looking! 7) Anticipatory Guidance: Encourage parents to have alone time together and individually to promote physical and emotional health needed to care for baby. Also do not become socially isolated from friends and family. Have 1:1 time with siblings. Involve siblings in care of baby as age appropriate. Young infants cannot be “spoiled” by holding, cuddling, talking or singing to them. In fact, engaging in these activities during alert states helps strengthen the trust and bond between parents and baby as well as language development. Encourage regular sleep/wake pattern by having baby placed in crib while still in drowsy state to calm self to sleep. Feed more frequently during the day to encourage longer stretch of sleep at night. Infants should not sleep in the parents bed, but a nearby sleep environment is recommended Do not smoke inside home, car, or around infant. Start “Tummy Time” when infants are awake Respond to your baby’s sounds by making sounds, showing your face to encourage “talk back” Vitamin D Supplementation: o Supplement breastfeed & partially breastfeed infants with 400 IU of Vitamin D beginning in the first few days of life. Supplementation should continue until the infant is weaned to 1 L/day or 1 quart/day of Vitamin D fortified formula or whole milk (AAP 2008 Policy Prevention of Ricketsattached). o All non-breastfeed infants who ingest < 1000 ml/day of Vitamin D fortified formula should receive vitamin supplement of 400 IU/day (AAP 2008 Policy of Rickets). o Preterm infants, when able to tolerate full enteral feeds, should be taking 400 IU of Vitamin D with max of 1000 IU/day (AAP 2013 Clinical Report on Calcium & Vitamin D Requirements on Enterally Fed Preterm Infants) References: 1. American Academy of Pediatrics, Bright Futures 3rd edition. 2008: 319-333. 2. Behrman, RE et al. Nelson Textbook of Pediatrics 16th edition. Philadelphia: WB Saunders Company, 2000. 3. Kleigman, RM et al. Nelson Textbook of Pediatrics 18th edition. Philadelphia: WB Saunders Company, 2007. 4