Educational Outcomes, Goals, and Objectives for Postgraduate Year Two
(PGY2) Pharmacy Residencies in Drug Information
Overview of PGY2 Pharmacy Residencies in Drug Information
PGY2 pharmacy residencies in drug information are designed to transition PGY1 residency
graduates from generalist practice to a specialized role as an organizational leader in the
development of safe and effective medication-use policies and/or processes and in the expert
analysis of medication-related information.
Residents leave the program as experts in searching, retrieving, analyzing, synthesizing, and
disseminating biomedical literature. Their analysis includes the ability to differentiate the degree
to which information is evidence-based. They can assert their ability to access and interpret the
facts as decisions about policy development for the use of medications, and the development of
medication-use processes that reflect those policies, are made. Graduates possess the advanced
facilitation skills to inform the organization’s policy-making bodies, influence their decision
making, and participate in the management of the decision-making process.
Pharmacists completing the residency are well prepared to meet the education and training needs
of both health care professionals and health care professionals in training. Also, they are very
capable of representing the pharmacy perspective to design and application of technology and
automation systems. Their excellent writing skills equip them to both contribute to the
biomedical literature themselves and to provide peer review for other contributors.
The superior communication skills developed in this residency enable a graduate to function as a
leader for activities such as conducting drug information practice-related projects and
contributing to the management of other projects.
1
Explanation of the Contents of This Document:
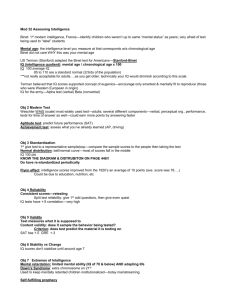
Each of the document’s objectives has been classified according to educational taxonomy
(cognitive, affective, or psychomotor) and level of learning. An explanation of the taxonomies is
available elsewhere.1
The order in which the required educational outcomes are presented in this document does not
suggest relative importance of the outcome, amount of time that should be devoted to teaching
the outcome, or sequence for teaching.
The educational outcomes, goals, and objectives are divided into those that are required and
those that are elective. The required outcomes, including all of the goals and objectives falling
under them, must be included in the design of all programs. The elective outcomes are provided
for those programs that wish to add to the required outcomes. Programs selecting an elective
outcome are not required to include all of the goals and objectives falling under that outcome. In
addition to the potential elective outcomes contained in this document, programs are free to
create their own elective outcomes with associated goals and objectives. Other sources of
elective outcomes may include elective educational outcomes in the list provided for PGY1
pharmacy residencies and educational outcomes for training in other PGY2 areas. Each of the
goals falling under the program’s selection of program outcomes (required and elective) must be
evaluated at least once during the resident’s year.
Educational Outcomes (Outcome): Educational outcomes are statements of broad categories of
the residency graduates’ capabilities.
Educational Goals (Goal): Educational goals listed under each educational outcome are broad
sweeping statements of abilities.
Educational Objectives (OBJ): Resident achievement of educational goals is determined by
assessment of the resident’s ability to perform the associated educational objectives below each
educational goal.
Instructional Objectives (IO): Instructional objectives are the result of a learning analysis of
each of the educational objectives. They are offered as a resource for preceptors encountering
difficulty in helping residents achieve a particular educational objective. The instructional
objectives falling below the educational objectives suggest knowledge and skills required for
successful performance of the educational objective that the resident may not possess upon
entering the residency year. Instructional objectives are teaching tools only. They are not
required in any way nor are they meant to be evaluated.
1
Nimmo, CM. Developing training materials and programs: creating educational objectives and assessing their
attainment. In: Nimmo CM, Guerrero R, Greene SA, Taylor JT, eds. Staff development for pharmacy practice.
Bethesda, MD: ASHP; 2000.
2
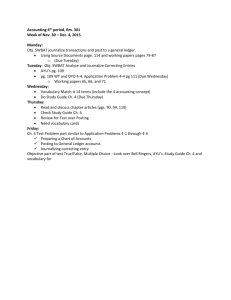
Required Educational Outcomes, Goals, and Objectives for Postgraduate Year Two
(PGY2) Pharmacy Residencies in Drug Information
Outcomes R1 through R5 are required for drug information
residencies in all settings.
Outcome R1: Demonstrate excellence in the provision of education, training, and evidencebased2 information for health care professionals and health care professionals in
training.
Goal R1.1
Provide effective education and training on medication-use or drug therapy topics
to health care professionals and health care professionals in training.
OBJ R1.1.1 (Application) Use effective educational techniques in the design of all
educational activities.
IO
Identify emerging issues in securing and integrating evidence-based
information suitable for educational sessions.
IO
Identify changes in medication-use that require training of staff.
IO
Explain the differences in effective educational strategies when teaching
colleagues versus residents versus students versus health professionals in
other disciplines.
IO
Design instruction that meets the individual learner’s needs.
IO
Write appropriately worded educational objectives.
IO
Explain how different instructional delivery systems (e.g., demonstration,
written materials, web-based) foster different types of learning.
IO
Design instruction that employs strategies, methods, and techniques
congruent with the objectives for an education or training program.
OBJ R1.1.2 (Synthesis) Design an assessment strategy that appropriately measures the
specified objectives for education or training and fits the learning situation.
OBJ R1.1.3 (Application) Use skill in the four preceptor roles employed in practicebased teaching (direct instruction, modeling, coaching, and facilitation).
IO
Explain the stages of learning that are associated with each of the
preceptor roles.
2
Evidence-based medicine -- the integration of best research evidence, clinical expertise, and
patient values in making decisions about the care of individual patients (Institute of medicine,
2001; Straus and Sackett, 1998). Best research evidence includes evidence that can be quantified,
such as that from randomized controlled trials, laboratory experiments, clinical trials,
epidemiological research, and outcomes research and evidence derived from the practice
knowledge of experts, including inductive reasoning (Guyatt et al., Higgs et al., 2001). Clinical
expertise is derived from the knowledge and experience developed over time from practice,
including inductive reasoning. Patient values and circumstances are the unique preferences,
concerns, expectations, financial resources, and social supports that are brought by each patient
to a clinical encounter. (Institute of Medicine. Health professions education: a bridge to quality.
Washington, DC: The National Academies Press; 2001.)
3
OBJ R1.1.4 (Application) Use advanced public speaking skills to communicate
effectively in large and small group situations.
IO
Explain the importance of developing excellence in public speaking if one
is to fulfill the role of a drug information specialist.
IO
Explain a systematic method for ongoing improvement in one’s own public
speaking skills.
OBJ R1.1.5 (Synthesis) Exercise skill in leading a small group discussion that focuses
on the evaluation of a piece of biomedical literature.
IO
Explain the journal club format.
Goal R1.2
Employ advanced literature analysis skills to analyze and effectively
communicate evidence-based information.
OBJ R1.2.1 (Synthesis) Create an efficient and effective advanced search strategy to
obtain information.
IO
Explain the full range of biomedical information resources that are
currently available.
IO
Explain content and applicability of specialized sources of biomedical
information.
IO
Explain the principles of use of search engines when the search needs to
be at an advanced level.
OBJ R1.2.2 (Analysis) Accurately identify the study design employed for a piece of
biomedical literature.
IO
Explain the key features of observational (e.g., epidemiologic) and
experimental designs and the strengths and weaknesses of each.
OBJ R1.2.3 (Evaluation) Determine if the study’s design and methodology are
appropriate to accomplish the objectives of a piece of biomedical literature.
OBJ R1.2.4 (Evaluation) Accurately interpret statistical information presented in a
piece of biomedical literature.
IO
Explain the application and interpretation of advanced statistical
methods.
IO
Determine instances in which a study conclusion is erroneously supported
by data display.
OBJ R1.2.5 (Analysis) Identify potential sources of bias in a piece of biomedical
literature.
OBJ R1.2.6 (Evaluation) Determine the internal and external validity of a piece of
biomedical literature.
OBJ R1.2.7 (Evaluation) Determine if a study’s results have applicability for
hypothesizing future research or for directing patient care decisions.
IO
Explain how level of evidence is determined.
OBJ R1.2.8 (Evaluation) When presented with conflicting biomedical literature,
determine the validity and applicability for a specific information need.
IO
Compare and contrast the reputations and of biomedical journals.
IO
Compare and contrast the peer-review procedures of biomedical journals.
IO
Explain how to appraise biomedical information for the expertise and
reputation of the author(s).
OBJ R1.2.9 (Evaluation) When presented with limited evidence-based biomedical
literature, synthesize a reasonable response for the specific information need.
4
OBJ R1.2.10 (Evaluation) Appraise information provided by a pharmaceutical
manufacturer.
OBJ R1.2.11 (Synthesis) Prepare an expert response to a complex information need.
IO
Explain standards of care applicable to a specific information need.
IO
Explain a standardized process for documenting, storing, and retrieving
information responses.
Goal R1.3
Contribute to the biomedical literature.
OBJ R1.3.1 (Synthesis) Write a piece of literature (e.g., research article, review, letter
to the editor, case report) that is suitable for publication.
IO
Use a standard style for biomedical journals in the preparation of
research articles, reviews, letters to the editor, or case reports submitted
for publication.
IO
Given a specific article, identify appropriate journals to which that article
might be submitted for publication.
IO
Given an identified topic related to pharmacy practice, appraise the
potential to publish an article on that topic.
IO
Explain the rules governing who may declare authorship of a given work.
IO
Explain rules governing disclosure and ethics for contributions to the
biomedical literature.
OBJ R1.3.2 (Application) Follow the submission requirements of an appropriate peerreviewed publication to submit a manuscript for publication.
OBJ R1.3.3 (Evaluation) Perform peer review of an article submitted for publication or
presentation by a pharmacist.
Goal R1.4
Prepare and deliver effective poster presentations.
OBJ R1.4.1 (Synthesis) Design an effective poster for the presentation of a specific
topic.
IO
Explain the types of content that should be included in a poster.
IO
Explain the rules for visual presentation of poster material.
IO
Explain resources that can be used to generate poster materials.
OBJ R1.4.2 (Synthesis) Exercise skill in responding to questions occurring during the
presentation of a poster.
Goal R1.5
Create pertinent, evidence-based medication information for health care
professionals.
OBJ R1.5.1 (Synthesis) Write evidence-based medication information for health care
professionals using appropriate grammar, punctuation, and style.
IO
Identify medication topics that warrant information distribution.
IO
Select an appropriate publication format for medication information (e.g.,
web page, newsletter, correspondence) for health professionals.
IO
Explain the value of creating polished and professional written and visual
materials.
OBJ R1.5.2 (Evaluation) Edit medication information prepared by others.
IO
Explain the signs and symbols utilized by editors.
IO
Explain the principles of editing.
IO
Explain the principles and methodology for proofreading.
OBJ R1.5.3 (Synthesis) Provide constructive feedback to authors of materials one has
edited.
5
IO
Explain how to provide feedback about written materials that is collegial
and constructive in nature.
OBJ R1.5.4 (Analysis) Determine the appropriate venue for distribution of a specific
piece of evidence-based medication information.
IO
Determine the appropriate method for distribution of information about a
specific medication topic.
IO
Apply the principles of timeliness and inclusiveness in the distribution of
medication information.
Outcome R2: Contribute to the management of the organization’s medication-use policies or
processes.
Goal R2.1
Enhance the quality of committee decisions on medication-use policies or
processes.
OBJ R2.1.1 (Synthesis) Plan a meeting that reflects the organization’s needs and the
political situation.
IO
Explain how to identify the stake holders who should be included in a
particular meeting.
IO
Explain how politics may affect the organization of a meeting.
IO
Explain a systematic process for creating a meeting agenda.
IO
Explain strategies that can be employed in advance to assure the success
of a meeting.
IO
Explain the principles of parliamentary procedure.
OBJ R2.1.2 (Synthesis) Prepare evidence-based information for committee decisions
on a medication-use policy or process, based on an analysis of the committee’s
needs.
IO
Explain the categories of information that the drug information specialist
may need to prepare for the committee.
IO
Explain pertinent therapeutic issues for making medication-use policy
and/or process recommendations or decisions.
IO
Explain ethical issues involved in making medication-use policy
recommendations or decisions.
IO
Explain the contribution of organizational data, knowledge of key
individuals and services, activity in the health care industry, and
reimbursement issues that may affect medication-use policy or processes.
IO
Explain specific areas to be researched when reviewing a product,
including cost, efficacy, and safety.
IO
Explain the pros and cons of establishing a formulary that contains
minimal duplication of therapeutically equivalent products.
IO
Explain the importance of establishing a formulary that restricts use of
non-formulary products to circumstances of true clinical need.
OBJ R2.1.3 (Analysis) Conduct a pharmacoeconomic analysis to support a medication
policy and/or process recommendation or decision.
IO
Explain the principles and methodology of pharmacoeconomic analysis.
IO
Explain reliable sources of data.
IO
Explain the impact of purchasing group and manufacturer contracts on
committee decision making.
6
IO
Explain differences between inpatient, outpatient, and PHS 340b costs.
IO
Explain reimbursement considerations on formulary decision making.
OBJ R2.1.4 (Synthesis) Contribute the drug information specialist’s perspective, as
appropriate, in meetings about a medication-use policy and/or process.
OBJ R2.1.5 (Synthesis) Prepare accurate and effective meeting minutes that satisfy the
requirements of organizational, regulatory, and accreditation considerations, as
applicable.
IO
Explain the requirements of the organization for recording meeting
minutes.
IO
Explain applicable regulatory issues that affect recording meeting
minutes.
IO
Explain applicable accreditation issues that affect recording meeting
minutes.
OBJ R2.1.6 (Synthesis) Design a systematic follow-up that assesses the
implementation and outcome of a change to a medication-use policy or process.
Goal R2.2
Identify opportunities for improvement in the organization’s medication-use
policies or processes.
OBJ R2.2.1 (Comprehension) Compare and contrast the feasibility and effectiveness of
the range of methods that can be used by the drug information specialist to
identify opportunities for improvement in a medication-use policy or process.
IO
Explain how to identify an appropriate topic for process improvement
activities.
OBJ R2.2.2 (Evaluation) Identify opportunities for improvement in a medication-use
policy or process based on the analysis of adverse drug events (ADEs).
IO
Explain methods used to identify ADE occurrences and trends.
IO
Explain the application of guidelines prepared by the Joint Commission
and ASHP to the development and implementation of ADE monitoring and
reporting programs.
IO
Explain the application of various approaches for minimizing ADEs.
OBJ R2.2.3 (Evaluation) Identify opportunities for improvement in a medication-use
policy or process based on the conduct of a medication-use project or a
comparison with benchmarking data.
IO
Explain how the conduct of a project contributes to monitoring for desired
outcomes.
IO
State sources of benchmarking information.
OBJ R2.2.4 (Analysis) Identify emerging trends and issues in medication use external
to an organization.
IO
Explain ways to monitor for emerging safety trends.
IO
Explain ways to monitor for emerging therapeutic issues.
OBJ R2.2.5 (Analysis) If applicable, identify emerging trends and issues in medication
use within one’s organization.
Goal R2.3
Develop and implement plans for improvements to the organization’s medicationuse process or policies.
OBJ R2.3.1 (Synthesis) Design an intervention to change a problematic or potentially
problematic aspect of a medication process or policy with the objective of
improving quality.
7
OBJ R2.3.2 (Synthesis) Collaborate with an interdisciplinary team to write or revise an
existing guideline or protocol.
OBJ R2.3.3 (Synthesis) Write or revise a medication-use policy or procedure with the
objective of improving its quality.
IO
Explain the influence of organizational climate on the design and
implementation of medication-use policies and procedures.
IO
Appraise current policies for congruence with the organization’s mission,
goals, and needs.
IO
Appraise current procedures for congruence with the organization’s
mission, goals, and needs.
OBJ R2.3.4 (Synthesis) Implement an intervention to change a problematic or
potentially problematic aspect of a medication policy or process with the
objective of improving quality.
IO
Explain the importance of continually reassessing medication-use
processes and policies.
IO
Describe the key organizational stakeholders and entities in the
implementation of a specific medication-use policy or procedure.
IO
Explain the kinds of educational activities that need to accompany
implementation of new or revised policies or procedures.
OBJ R2.3.5 (Evaluation) Measure the impact of a change to a medication-use process
or policy.
Goal R2.4
Develop strategies for improving an organization’s adverse drug event (ADE)
monitoring and reporting program.
OBJ R2.4.1 (Synthesis) Formulate strategies for improvement of the organization’s
ADE monitoring and reporting program.
IO
Explain the impact of a non-punitive culture or environment on ADE
reporting.
IO
Explain how the method of ADE data collection affects results and the
ability to detect trends.
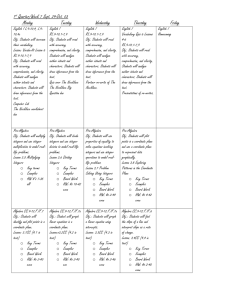
Outcome R3: Exercise leadership and practice management skills.
Goal R3.1
Exhibit essential personal skills of a practice leader.
OBJ R3.1.1 (Characterization) Practice self-managed continuing professional
development with the goal of improving the quality of one’s own performance
through self-assessment and personal change.
IO
State the criteria for judging one’s performance of tasks that are critical
in one’s own practice.
IO
Explain the importance of staying current with pertinent biomedical
literature.
IO
Explain the importance of staying current with health news in the popular
media.
IO
Explain the importance of continuing to keep current and grow in both
clinical and management skills.
IO
Explain the role of board certification in the development and
maintenance of expertise in drug information practice.
IO
Explain the role of the drug information specialist as a process expert.
8
OBJ R3.1.2 (Characterization) Demonstrate commitment to the profession of
pharmacy through active participation in local, state, and/or national pharmacy
professional organizations.
OBJ R3.1.3 (Comprehension) Explain the nature of mentoring in pharmacy, its
potential connection with achievement, and the importance of willingness to serve
as mentor to appropriate individuals.
OBJ R3.1.4 (Comprehension) Explain the general processes of establishing and
maintaining an ASHP-accredited residency program.
OBJ R3.1.5 (Comprehension) Explain the importance of contributing to the
advancement of the profession through presentations and publications.
OBJ R3.1.6 (Application) Use time management skills effectively to fulfill practice
responsibilities.
IO
Explain an effective system for the management of one’s time in
professional practice.
IO
Explain strategies for preventing procrastination.
IO
Explain how effective time management can reduce stress.
IO
Explain the importance of prioritizing according to the level of importance
and rapidly adapting to change.
IO
Explain how to develop a reasonable timeline for a project.
IO
Explain strategies for keeping one’s work on a project at a pace that
matches the timeline plan.
IO
Explain strategies for satisfactorily making progress on several projects
simultaneously.
IO
Explain potential negative consequences of failure to achieve balance in
personal and professional life.
OBJ R3.1.7 (Characterization) Use sound ethical reasoning to guide practice decisions.
IO
Explain common practice situations that can present ethical dilemmas.
IO
Appraise current policies governing relations between the organization
and the pharmaceutical industry to ensure that ethical practices are
observed.
IO
Explain why pharmaceutical industry representatives regard the drug
information specialist as an influential individual in their organization.
IO
Explain the appropriate relationship between the drug information
specialist and a pharmaceutical industry representative.
IO
Explain ethical issues that may arise in publishing and applying
biomedical literature.
OBJ R3.1.8 (Analysis) Identify potential conflict-of-interest situations in one’s
practice.
IO
Explain the concept of perceived conflict-of-interest versus actual conflictof-interest.
IO
Explain the types of conflict-of-interest that may arise in research,
purchasing, formulary decision-making, publishing, and professional
practice.
IO
Explain potential strategies for resolving various conflict-of-interest
situations that commonly occur in practice.
9
OBJ R3.1.9 (Comprehension) When applicable, explain the intricacies of all regulatory
and accreditation requirements that affect the medication-use policies or processes
of the organization.
IO
Explain the contents and implications of The Joint Commission standards
relevant to medication-use policies and/or procedures.
IO
Explain the contents and implications of the United States Pharmacopeia
standards relevant to medication-use policies and/or procedures.
IO
Explain the contents and implications of regulations regarding drug
research.
IO
Explain the contents and implications of regulations regarding the
marketing of drugs.
IO
Explain the drug regulatory process and its implications for practice.
IO
Explain the contents and implications of regulations governing the
pharmaceutical industry.
Goal R3.2
Exercise superior communications skills.
OBJ R3.2.1 (Application) Use effective negotiation skills to resolve conflicts.
OBJ R3.2.2 (Characterization) Demonstrate a commitment to advocacy for optimal
care of patients through the assertive and persuasive presentation of patient care
issues to members of the organizational leadership, health care team, the patient,
and/or the patient’s caregivers.
OBJ R3.2.3 (Application) Use group participation skills when leading, facilitating, or
working as a member of an interdisciplinary committee or informal work group.
IO
Explain the roles and responsibilities of the facilitator of a meeting.
IO
Explain effective strategies for facilitating meetings.
OBJ R3.2.4 (Synthesis) Develop strategies for dealing with challenging
communications situations.
IO
Explain how to assess the level of health literacy of a patient.
IO
Explain the importance of adjusting one’s communications according to
the level of health literacy of the patient.
IO
Explain common situations in the work of a drug information specialist
that can produce a difficult communications encounter.
IO
Explain effective communications strategies that could be used in a
difficult encounter.
IO
Explain the importance of adjusting one’s communications to adjust for
cultural differences.
IO
Explain communication strategies that are appropriate for patients who
are non-English speakers or who are impaired.
IO
Explain ways in which a communication strategy can be modified to
accommodate the individual’s personal characteristics.
OBJ R3.2.5 (Analysis) Determine the appropriate type of communication, and the
medium and organization for it, using an understanding of the target audience, the
characteristics of the information to be communicated, effectiveness, efficiency,
customary practice and the recipient's preferences.
IO
Accurately identify the primary theme or purpose of one's written or oral
communication.
10
IO
Accurately determine what information will provide credible background
to support or justify the primary theme of one's written or oral
communication.
IO
Logically sequence ideas in written and oral communication.
IO
Accurately determine the depth of communication appropriate to one's
audience.
IO
Accurately determine words and terms that are appropriate to one's
audience.
IO
Accurately determine one's audience's needs.
IO
Accurately identify the length of communication that is appropriate to the
situation.
IO
Explain the importance of assessing the receiver's understanding of the
message conveyed.
IO
Explain techniques for persuasive communications.
IO
Explain the value of consulting with administrators and key decisionmakers when choosing route(s) for communication of information.
IO
Explain issues, including confidentiality, surrounding the choice of media
to communicate information.
IO
Explain the differences in impact of different modes of communication.
OBJ R3.2.6 (Application) Use listening skills effectively in performing job functions.
IO
Explain the use of body language in listening to others.
IO
Explain verbal techniques that can be used to enhance listening to others.
IO
Explain the process of active listening.
IO
Explain the role of active listening in effective communications.
Goal R3.4
Demonstrate political skills necessary to improve the organization’s medicationuse process or policies.
OBJ R3.4.1 (Analysis) When confronted with a barrier to the accomplishment of a
particular project, analyze the organizational environment, including its structure,
network of resources, and politics, to determine a strategy for achieving success.
IO
Explain the organization’s structure including the function of each of its
departments and key individuals.
IO
Explain the importance of effective networking in removing barriers.
IO
Explain how to identify key stakeholders of a given project.
IO
Explain the importance of persuasion as a skill of effective leaders.
IO
Compare and contrast the types of persuasive arguments that are
potentially effective.
IO
Identify formal and informal medical staff leaders and how they can help
achieve the desired goal.
OBJ R3.4.2 (Synthesis) Create an effective professional network.
IO
Explain formal and informal techniques for networking.
OBJ R3.4.3 (Analysis) Identify the organization’s committees where pharmacist
participation is essential.
11
Outcome R4: Conduct drug information practice-related projects.
Goal R4.1
Conduct a drug information practice-related project using effective project
management skills.
OBJ R4.1.1 (Synthesis) Identify a topic of significance for a drug information practicerelated project.
IO
Explain the types of resident projects (e.g., prospective, retrospective,
clinical trials) that will meet residency program project requirements and
timeframe.
IO
Explain how one determines if a potential project topic is of significance
in one’s particular practice setting.
IO
Explain how to conduct an efficient and effective literature search for a
project.
IO
Explain how to generate a research question(s) to be answered by an
investigation.
OBJ R4.1.2 (Synthesis) Formulate a feasible design for a drug information practicerelated project.
IO
Explain the elements of a project proposal.
IO
Explain how to identify individuals who will be affected by the conduct of
the project and strategies for gaining their cooperation.
IO
Explain how to determine a timeline with suitable milestones that will
result in project completion by an agreed-upon date.
IO
Explain the ethics of research on human subjects and the role of the
institutional review board.
IO
Explain various methods for constructing data collection tools.
OBJ R4.1.3 (Synthesis) Secure any necessary approvals, including investigational
review board approval, for one’s design of a project.
IO
Explain how to identify key stakeholders who must approve a particular
project.
OBJ R4.1.4 Secure any necessary funding for one’s project.
IO
Explain the components that make up a budget for a project.
OBJ R4.1.5 (Synthesis) Conduct a drug information practice-related project as
specified in its design.
IO
Explain strategies for keeping one’s work on a project at a pace that
matches the projected timeline.
IO
Given a particular residency project, explain methods for organizing and
maintaining project materials and documentation of the project’s ongoing
progress.
IO
Explain methods of data analysis.
OBJ R4.1.6 (Synthesis) Effectively present the results of a drug information practicerelated project.
OBJ R4.1.7 (Synthesis) Successfully employ an accepted manuscript style to prepare a
final report of a drug information practice-related project.
IO
Given a particular residency project to be presented, explain the type of
manuscript style appropriate to the project and criteria to be met when
using that style.
12
OBJ R4.1.8 (Evaluation) Accurately assess the impact, including sustainability if
applicable, of the residency project.
Outcome R5: Contribute to the management of the organization’s budget.
Goal R5.1
Provide drug cost forecasting.
OBJ R5.1.1 (Analysis) Estimate the future cost implications for the organization of a
new pharmaceutical agent.
IO
List sources of information for medications in the pipeline.
IO
Explain factors to consider when forecasting costs of a new agent.
OBJ R5.1.2 (Analysis) Estimate the future cost implications for the organization from
patent expiration.
IO
List sources of information for patent life.
IO
Explain factors to consider when forecasting savings with a new generic.
OBJ R5.1.3 (Comprehension) Explain the organization’s overall drug costs.
Goal R5.2
Understand organizational decision-making for contracting for pharmaceuticals.
OBJ R5.2.1 (Comprehension) Explain the organization’s process for negotiating
contracts for pharmaceuticals.
IO
Explain the relationships between the manufacturers of medications,
group purchasing organizations (GPOs), wholesalers, and pharmacies.
IO
Explain laws and rules related to “own use” purchasing contracts.
IO
Explain the concept of bundling relative to contracting.
IO
Explain the concept of tiers.
IO
Explain the concept of contract rebates.
IO
Explain the concept of market share.
IO
Explain the concept of chargebacks.
IO
Explain the typical bidding process for the purchase of pharmaceuticals.
IO
Explain the importance of effective contract analysis.
IO
Explain methods that GPOs use to evaluate multi-source drugs and
vendor bid responses.
13
Elective Educational Outcomes, Goals, and Objectives for Postgraduate Year Two
(PGY2) Pharmacy Residencies in Drug Information
Outcome E1 is recommended for drug information residencies conducted in
hospitals and health systems.
Outcome E1: Contribute to the management of the organization’s medication-use process.
Goal E1.1
Contribute to efforts to prevent and identify risk points in the medication-use
process.
OBJ E1.1.1 (Evaluation) Participate in a proactive risk assessment, such as a failure
mode and effects analysis (FMEA) or the Six Sigma methodology to define,
measure, analyze, improve, and control (DMAIC).
OBJ E1.1.2 (Comprehension) Explain the steps and applicability of a root cause
analysis (RCA).
Goal E1.2
Represent the pharmacy perspective to the organization’s design and application
of its technology and automation systems.
OBJ E1.2.1 (Comprehension) Explain how to maintain effective liaisons between the
pharmacy and information technology staff and other health care disciplines to
support medication use.
IO
Explain the value of good peer relationships in the achievement of
informatics projects.
IO
Explain the organization’s information systems organization and the
links/matrix with pharmacy informatics professionals.
IO
Explain differences in the approach to the resolution of information flow
problems between clinicians and information technology professionals.
OBJ E1.2.2 (Synthesis) In collaboration with information technology professionals,
physicians, nurses, pharmacists, and other pertinent health care providers, define
patient information and medication information required by the organization’s
information system to support effective medication-related patient-care decisions
by physicians, nurses, pharmacists, and other pertinent health care providers.
IO
Explain the principles of decision support as they apply to health care
providers making direct patient-care decisions and their effect on
medication use.
IO
Compare and contrast the benefits and risks of currently available
technology and automation systems.
OBJ E1.2.3 (Synthesis) Collaborate with physicians, nurses, pharmacists, and other
pertinent health care providers to standardize the organization’s processes for the
communication of medication orders so that the risk of errors is minimized.
IO
Explain the benefits and risks of a computerized prescriber order-entry
(CPOE) system.
IO
Explain the value of preprinted order forms for improving medication-use
safety in the absence of CPOE.
OBJ E1.2.4 (Application) Participate in coordinating the inclusion of new formulary
and medication-use information into the organization’s technology and
automation systems.
14
IO
Explain the importance of assuring that formulary additions are promptly
entered into the existing technology and automation systems.
Goal E1.3
Collaborate with others in the organization to assure the availability of
appropriate evidence-based medication information for the organization’s health care
providers.
OBJ E1.3.1 (Synthesis) Formulate or make improvements to an existing plan that
assures the availability of complete, current, evidence-based medication
information resources in the pharmacy and in all patient-care areas where
medications are prescribed and/or administered.
IO
For the full scope of medication information resources for use in a specific
area of the organization, accurately assess the currency, accuracy,
effectiveness, and degree to which they are evidence-based.
IO
Explain the importance of ready access to current protocols, guidelines,
dosing scales, and checklists for medications by physicians, pharmacists,
nurses, and other pertinent health care providers.
Outcome E2 is recommended for drug information residencies conducted in
settings with a formal drug information center/service.
Outcome E2: Contribute to the management of a drug information center/service.
Goal E2.1
Contribute to the management of a drug information center/service.
OBJ E2.1.1 (Comprehension) Explain the components of a proposal for the addition of
services or resources to an existing drug information center/service.
IO
Explain the resources needed to initiate a drug information center/service.
IO
Explain the elements of a business plan.
OBJ E2.1.2 (Synthesis) Devise strategies for fiscally sound management of a drug
information center/service.
OBJ E2.1.3 (Synthesis) Devise strategies for managing the human resources of a drug
information center/service that result in an pleasant, effective and efficient
working environment.
IO
Describe the qualifications of personnel for a drug information
center/service.
IO
Explain effective recruitment strategies that could be used for a specific
position in a drug information center/service.
IO
Explain effective interviewing strategies for the selection of potential
employees.
IO
Explain the components of an evaluation system for staff of a drug
information center/service that is consistent with the organization’s
policies on human resource management.
IO
Explain the principles of progressive discipline.
IO
Explain the components of an effective orientation and training program.
OBJ E2.1.4 (Evaluation) Continually reassess the drug information needs of the
organization.
15
OBJ E2.1.5 (Synthesis) Use documented information on services provided by the drug
information center/service to generate reports that describe the center’s/service’s
productivity, quality, and outcomes.
OBJ E2.1.6 (Evaluation) Appraise a drug information center’s/service’s continuous
quality improvement program for effectiveness.
IO
Explain the principles of continuous quality improvement.
OBJ E2.1.7 (Synthesis) Design improvements in a drug information center/service.
Goal E2.2
Formulate the budget for a drug information center/service.
OBJ E2.2.1 (Comprehension) Explain how to formulate a capital budget for a drug
information center/service.
IO
Explain the organization’s capital budgeting process.
IO
Explain what items should be included in a capital budget.
IO
Explain the kinds of data required and appropriate resources for
gathering data to support the need for capital budget items, including
equipment specifications and vendor options.
IO
Explain how to write a justification for items submitted for approval for
the capital budget according to the organization’s policies and
procedures.
OBJ E2.2.2 (Comprehension) Explain how to formulate a personnel budget for a drug
information center/service.
IO
Explain how to identify staffing requirements to include in the personnel
budget.
IO
Use a knowledge of the kinds of data required and appropriate resources
for gathering data to support staffing requirements, including projected
hours of staffing, salaries, overtime, differentials, turnover, workload
analysis, and productivity records.
IO
Explain how to write a justification for staffing resources submitted for
approval for the personnel budget according to the organization’s policies
and procedures.
OBJ E2.2.3 (Comprehension) Explain how to formulate an operating budget for a drug
information center/service.
IO
Explain what items should be included in the operating budget.
IO
Use a knowledge of the kinds of data required and appropriate resources
for gathering data to support the need for operating budget items,
including fixed and variable expenses.
IO
Explain how to determine operating budget accounts and funding levels to
submit for approval.
IO
Explain strategies for securing needed operating budget accounts and
funding levels.
IO
Explain how to write a justification for operating budget accounts and
funding levels submitted for approval according to the organization’s
policies and procedures.
OBJ E2.2.4 (Comprehension) Explain how to formulate a revenue budget for a drug
information center/service.
IO
Explain sources of revenue for a drug information center/service.
16
Outcome E3: Demonstrate excellence in the provision of evidence-based information and
education for the public.
Goal E3.1
Provide effective information and education on medication-use issues to the
public.
OBJ E3.1.1 (Synthesis) Create accurate, appropriate, and timely evidence-based health
information for use by the media.
IO
Explain the types of information that different media will seek.
IO
Explain the lack of control of the final disposition of information provided
to the press.
OBJ E3.1.2 (Synthesis) Create accurate, appropriate, and timely evidence-based health
information for use by a lay person.
OBJ E3.1.3 (Synthesis) Create accurate, appropriate, and timely evidence-based health
information for the community groups.
OBJ E3.1.4 (Synthesis) Design health information educational programs for the lay
public.
Goal E3.2
Understand the role of the drug information specialist in responding to requests
from legal professionals.
OBJ E3.2.1 (Comprehension) Explain the role of the drug information specialist in
responding to requests for information for use in legal cases.
Outcome E4: Participate in the provision of drug study services.
Goal E4.1
Manage the use of study drugs according to established protocols and the
organization’s policies and procedures.
OBJ E4.1.1 (Application) Utilize appropriate procedures in storing study drugs.
IO
Explain the organization’s policies and procedures for storing study
drugs.
IO
Explain problems that commonly occur with storing study drugs.
IO
Explain how to correct common problems that occur with the storage of
study drugs.
OBJ E4.1.2 (Application) Utilize appropriate procedures in dispensing study drugs.
IO
Explain how to identify the correct protocol and determine if a patient
meets study criteria for entry.
IO
Explain the importance of confirming that patients have signed an
informed consent.
IO
Explain the organization’s policies and procedures for dispensing study
drugs.
IO
Explain problems that commonly occur with dispensing of study drugs.
IO
Explain how to correct common problems that occur with dispensing of
study drugs.
OBJ E4.1.3 (Application) Utilize appropriate procedures in documenting actions taken
with study drugs.
IO
Explain appropriate documentation for drug study records.
OBJ E4.1.4 (Application) Utilize appropriate procedures for initiation of a drug study.
IO
Explain how to prepare a drug study budget.
IO
Explain how to identify the processes necessary for conduct of a drug
study.
17
IO
Explain principles for preparing necessary information for a drug study.
OBJ E4.1.5 (Evaluation) Critique a protocol and patient consent according to
conventions established by the organization’s institutional review board.
OBJ E4.1.6 (Comprehension) Explain the process for reporting adverse drug events
that occur during a drug study.
Outcome E5: Demonstrate skills required to function in an academic setting.
Goal E5.1
Understand faculty roles and responsibilities.
OBJ E5.1.1 (Comprehension) Explain variations in the expectations of different
colleges/schools of pharmacy for teaching, practice, research, and service.
IO
Discuss how the different missions of public versus private
colleges/schools of pharmacy can impact the role of faculty members.
IO
Discuss maintaining a balance between teaching, practice, research and
service.
IO
Discuss the relationships between scholarly activity and teaching,
practice, research and service.
OBJ E5.1.2 (Analysis) Explain the role and influence of faculty in the academic
environment.
IO
Explain the responsibilities of faculty in governance structure (e.g. the
faculty senate, committee service).
IO
Describe the responsibilities of faculty (e.g. curriculum development and
committee service) related to teaching, practice, research, and service
roles.
OBJ E5.1.3 (Comprehension) Describe the academic environment.
IO
Describe how the decisions by university and college administration
impact the faculty.
IO
Discuss outside forces (e.g. change in the profession, funding source,
accreditation requirements) that impact administrator and faculty roles.
OBJ E5.1.4 (Comprehension) Describe the types and ranks of faculty appointments.
IO
Explain the various types of appointments (e.g. non-tenure, tenure-track,
and tenured faculty).
IO
Differentiate among the various ranks of faculty (e.g. instructor, assistant
professor, associate professor, full professor).
IO
Discuss the role and implications of part-time and adjunct faculty as
schools continue to expand and faculty shortages occur.
OBJ E5.1.5 (Comprehension) Discuss the promotion and/or tenure process for each
type of appointment.
IO
Identify the types of activities that are considered in the promotion
process.
IO
Identify the types of activities that are considered for tenure.
OBJ E5.1.6 (Application) Identify resources available to help develop academic skills.
IO
Explain the role of academic-related professional organizations (e.g.
AACP) in faculty professional development.
IO
Identify resources to help develop teaching skills and a teaching
philosophy.
18
OBJ E5.1.7
(Comprehension) Explain the characteristics of a typical affiliation
agreement between a college of pharmacy and a practice site (e.g., health
system, hospital, clinic, retail pharmacy).
IO
Explain how the political environments of either a college or a practice
site may affect the other.
Goal E5.2
Exercise teaching skills essential to pharmacy faculty.
OBJ E5.2.1 (Synthesis) Develop an instructional design for a class session, module, or
course.
IO
Construct a student-centered syllabus.
IO
Construct educational objectives for a class session, module, or course
that is appropriate to the audience.
IO
Identify appropriate instructional strategies for the class session, module,
or course to achieve the objectives.
IO
Consider assessment tools that measure student achievement of the
educational objectives.
OBJ E5.2.2 (Synthesis) Prepare and deliver didactic instruction on a topic relevant to
the specialized area of pharmacy residency training.
IO
Identify educational technology that could be used for a class session,
module, or course (e.g., streaming media, course management software,
audience response systems).
IO
Create instructional materials appropriate for the topic and audience.
IO
Identify strategies to deal with difficult learners.
IO
Given feedback from teaching evaluations (e.g. student and or peer),
devise a plan to incorporate improvements in future instruction.
OBJ E5.2.3 (Application) Develop and deliver cases for workshops and/or exercises
for laboratory experiences.
IO
Identify the appropriate level of case-based teachings for small group
instruction.
IO
Identify appropriate exercises for laboratory experiences.
IO
Provide appropriate and timely feedback to improve performance.
OBJ E5.2.4 (Application) Serve as a preceptor or co-preceptor utilizing the four roles
employed in practice-based teaching (direct instruction, modeling, coaching and
facilitation).
IO
Assess the learner’s skill level to determine the appropriate preceptor
strategy for providing practice-based teaching.
IO
Given performance-based criteria, identify ways to provide constructive
feedback to learners.
IO
Develop strategies to promote professional behavior.
IO
Identify strategies to deal with difficult learners in the practice setting.
IO
Given a diverse learner population, identify strategies to interact with all
groups with equity and respect.
OBJ E5.2.5 (Analysis) Develop a teaching experience for a practice setting (e.g.,
introductory or advanced pharmacy experience).
IO
Create educational goals and objectives to be achieved.
IO
Develop activities that will allow achievement of identified educational
goals and objectives.
19
IO
IO
IO
Identify how and when feedback should be provided.
Identify other preceptors for the experience, if appropriate.
Determine training that might be needed for the preceptors to deliver
student education.
IO
Identify potential challenges of precepting and providing patient care
services simultaneously.
OBJ E5.2.6 (Synthesis) Design an assessment strategy that appropriately measures the
specified educational objectives for the class session, module, course, or rotation.
IO
Identify appropriate techniques for assessing learning outcomes in various
educational settings [e.g., written examinations, oral examinations,
practical examinations, Objective Structured Clinical Examination
(OSCE)].
IO
Develop examination questions to assess the knowledge, skills, attitudes
and behaviors that are appropriate to the learner’s level and topic.
IO
Discuss the various methods for administering examination questions
(e.g., computerized testing, paper testing).
OBJ E5.2.7 (Evaluation) Create a teaching portfolio.
IO
Define the concept of a teaching portfolio and describe its primary
purpose
IO
Outline the steps in building a teaching portfolio.
IO
Develop a personal teaching philosophy to guide one’s teaching efforts
and facilitate student learning.
OBJ E5.2.8 (Evaluation) Compare and contrast methods to prevent and respond to
academic and profession dishonesty.
IO
Evaluate physical and attitudinal methods to prevent academic dishonesty.
IO
Discuss methods of responding to incidents of academic dishonesty.
IO
Discuss the role of academic honor committees in cases of academic
dishonesty.
IO
Identify examples and methods to address unprofessional behavior in
learners.
OBJ E5.2.9 (Comprehension) Explain the relevance of copyright laws to developing
teaching materials.
IO
Discuss copyright regulations as related to reproducing materials for
teaching purposes.
IO
Discuss copyright regulations as related to linking and citing on-line
materials.
Outcome E6: Contribute to the organization’s decisions for the selection of medicationrelated devices.
Goal E6.1
Contribute to decisions on the purchase of medication-related devices.
OBJ E6.1.1 (Evaluation) Conduct an evidence-based assessment of a medicationrelated device.
IO
Compare and contrast methodology for evaluating a drug versus
evaluating a device.
IO
Explain the Food and Drug Administration (FDA) device approval
process.
20
Approved by the ASHP Commission on Credentialing on March 8, 2008. Endorsed by the ASHP
Board of Directors on April 18, 2008. Developed by the ASHP Commission on Credentialing in
collaboration with the American College of Clinical Pharmacy (ACCP) and the Consortium for
the Advancement of Medication Information, Policy, and Research (CAMIPR). The design
group comprised the following drug information practitioners, residency program directors, and
ASHP staff: Lisa A. Boothby, Pharm.D., BCPS, Coordinator, Drug Information Services,
Columbus Regional Health Care System; Michelle W. McCarthy, Pharm.D., Drug Information
Specialist, University of Virginia Health System; Linda S. Tyler, Pharm.D., FASHP, Director,
Drug Information Service, University of Utah Hospitals and Clinics; Cindy J. Wordell,
Pharm.D., Assistant Director of Pharmacy, Medication Use Policy, Research and Clinical
Services, Thomas Jefferson University Hospital; Bruce A. Nelson, R.Ph., M.S., Director,
Operations, Accreditation Services Division, ASHP; and Christine M. Nimmo, Ph.D., Director,
Standards Development and Training, Accreditation Services Division, ASHP. This document
replaces the educational goals and learning objectives for drug information pharmacy residencies
approved by the ASHP Board of Directors on November 15, 1997. The contribution of reviewers
is gratefully acknowledged.
Copyright © 2008, American Society of Health-System Pharmacists, Inc. All rights reserved.
The effective date for implementation of these educational outcomes, goals and objectives is
commencing with the entering resident class of 2009.
21