Steve`s Anatomy of the Thorax
advertisement

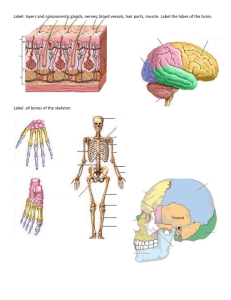
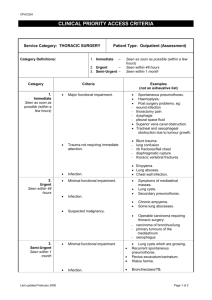
S Tran Anatomy of the Thorax Learning Objectives 1. Explain the roles of skeleton, muscles, pleural cavities and lungs in breathing. 2. Explain the functions, positions and relations of the structures entering and leaving the lungs. 3. Explain the anatomical principles underlying insertion of chest drains and relief of tension pneumothorax and cardiac tamponade. 4. Describe the arterial supply and venous drainage of the thoracic viscera and thoracic walls. 5. Define the mediastinum and demonstrate its subdivisions and contents. 6. Explain the principles of X-ray imaging methods and identify the features of the normal adult chest in conventional X-ray and CT images. 7. Demonstrate using correct terminology the position and relations of the pericardium and pericardial sac, heart chambers and valves in anatomical specimens, living subjects and images. 8. Explain the origins of heart sounds and demonstrate optimal auscultation of each valve. 9. Describe and recognise normal breath sounds and percussion sounds. 10. Explain the pathways through which the heart, lungs, chest wall and diaphragm obtain their sensory and motor nerve supplies and explain referred pain of thoracic origin. 11. Describe the anatomical organisation and pathways of lymphatic drainage of the breasts. 12. Explain the physiology of lymph formation, the structure and functions of lymph nodes, the importance of lymphatic drainage in the dissemination of cancers and infections and the main pathways for lymphatic drainage of the body. 13. Demonstrate the intrathoracic positions and relations of the trachea, oesophagus, thoracic duct, vagus nerves and phrenic nerves. pg. 1 S Tran Lecture 1: The Thoracic Wall: Ribs: TRUE: 1-7 reach sternum FALSE: 8-10 reach costal cartilage above FLOATING: 11-12 lack anterior attachment Articulations/joints with vertebral column (heads)/costal cartilage(tubercles) Most lung tissue and most capacity for lung expansion is in the lower thorax Diaphragm: Has a flat central tendon with muscle radiating to costal margin and vertebrae. 1st – dome flattens to increase vertical diameter of chest. 2nd – pulls costal margin up to increase transverse and antero-posterior diameters Sternum: MANUBRIUM BODY XIPHOID a. b. c. d. e. 1st costal cartilages attach to manubrium 2nd to M-S joint 3rd – 7th to Sternum 8th – 10th to Cartilage above 11th & 12th Floating Thoracic Inlet is a ring formed of: pg. 2 S Tran 1st Thoracic Vertebra (T1) 1st Ribs Manubrium Intercostal Muscles Have a secondary role – stiffen chest wall to improve efficiency of breathing movements 1. External Intercostals – a. Downwards & laterally from lower border of rib above to rib below. b. Replaced by anterior intercostal membrane at costo-chondral junction. 2. Internal Intercostals – a. attachments begin anteriorly at the sternum – from lower border of rib above to rib below – fibres directed at right angles to external intercostals. b. Replaced by membrane posteriorly 3. Innermost intercostals – Relatively trivial Intercostal neurovascular bundles VAN = Vein, Artery & Nerve, just below rib deep to internal intercostals Each intercostals artery joins (anastomoses) with a major artery at each end of the intercostal space Drains into internal thoracic vein Intercostal Nerves o 11 pairs T1-T11 (+ 1 Subcostal – T12) o Mixed (Motor & Sensory) o Supplies intercostals spaces o Lateral cutaneous branches (anterior and posterior) o Anterior cutaneous – medial and lateral pg. 3 S Tran Lecture 2: Bronchi, Lungs, Pleura and Diaphragm Bronchial Tree Trachea o o o Primary (main) Bronchi (L&R) o o Formed at T4/5 Right Wider and more vertical than left Lobar (Secondary) Bronchi o o o C6 to T4/5 Held open by C-shaped Cartilage rings Lowest ring has a hook – Carina (keel of ship) Formed within the lungs Supply the lobes of the lungs 2 LEFT 3 RIGHT Segmental (Tertiary) Bronchi o Supply the bronchopulmonary segment Lungs Essential for Respiration Separated from each other by mediastinum Lie freely in its pleural cavity apart from attachment to heart and trachea at the lung root (HILUM) Conical in shape APEX o Thoracic inlet oblique – apex rises 3-4cm above first costal cartilage level BASE o Concave o Rests on Convex surface of diaphragm 3 Borders – ANTERIOR, POSTERIOR, INFERIOR 3 Surfaces – COSTAL, MEDIAL(MEDIASTINAL), INFERIOR (DIAPHRAGMATIC) Diaphragm separates the right lung from right lobe of liver and the left lung from left lobe of the liver, stomach & spleen. Mediastinial surface: POSTERIOR – in contact with thoracic vertebrae ANTERIOR – deeply concave – accommodates heart – cardiac impression larger on L than R ABOVE & BEHIND – cardiac impression – hilum where vessels, bronchi & nerves enter. pg. 4 S Tran Left Lung Two lobes separated by oblique fissure: o Superior o Inferior Superior lies above the fissure and includes apex & most of anterior part of lung. Right Lung Slightly larger three lobes separated by oblique fissure & horizontal fissure: o Superior o Middle o Inferior (Oblique fissure) The Root (Hilum) of the Lung Connects mediastinal surface to heart & trachea, all enveloped in plerua: Principal (Primary) Bronchus Pulmonary Artery 2 Pulmonary Veins Bronchial Arteries (oxygenated blood from descending aorta) & Veins Pulmonary plexus of nerves (Autonomic) Lymph vessels and nodes The Pleura “Thin layer of flattened cells supported by connective tissues that lines each pleural cavity and covers the exterior of the lungs.” o Visceral Pleura– covers surface of lungs and lines fissures between the lobes o Partietal Pleura – lines inner surface of chest walls Visceral and parietal pleura are continuous with each other around the hilum. Pleural cavity is collapsed, but moist surfaces allow lungs to glide as they expand and collapse. Originally pleural pleura lined the pleural cavities, lung buds grew into them within visceral pleura covering. Costo-diaphragmatic recess of pleura – free of lung except in maximal inspiration. Breathing 1. Controlled by nervous system and produced by skeletal muscle 2. Brings about inhalation and exhalation of air into/out of the lungs, to ventilate the gas exchange areas - alveolar sacs 3. capacity of thoracic cavity can be increased: by movements of the diaphragm by movements of the ribs pg. 5 S Tran Mechanism of breathing Pleural Cavity expanded by wall muscles Elastic lungs expand with the pleural cavity, sucking air down trachea and bronchi into lungs The Diaphragm – Main Inspiratory Muscle Contracts increase vertical dimension of the thoracic cavity Diaphragm presses on the abdominal viscera which initially descend due to abdominal wall relaxation during inspiration. Further descent is stopped by abdominal viscera, so more contracts raises the costal margin. Increased thoracic capacity produced by diaphragm & rib movements, reduces intrapleural pressure, with entry of air through respiratory passages & expansion of the lungs. Costal margin (lower border of rib cage) of diaphragm o Xiphoid process o Ends of ribs 11 and 12 o Lumbar vertebrae Ribs in breathing: Ribs elevated – anterior ends thrust forward & upwards – increase antero-posterior dimension of thoracic cavity. Ribs are everted, increasing transverse diameter of thoracic cavity Internal & external intercostal muscles stiffen the rib cage to increase efficiency of diaphragm pg. 6 S Tran Raising the costal margin also raises drooping anterior ends ribs, tilting sternum upwards to increase antero-posterior diameter of pleural cavities (pump-handle action – blue arrow) Breathing out Quiet expiration is a passive activity not requiring muscles It depends on elastic recoil in the elastic tissue throughout the lungs and in the rib cage In deep or forced expiration, this is assisted by the muscles of the abdominal walls that squeeze the abdominal organs against the diaphragm and pull the lower ribs downward pg. 7 S Tran Lecture 3: Superior Mediastinum Thick midline partition between two pleural cavities Conduit (channel) for structures that passes through the thorax or to other body regions. Extends from SUPERIOR THORACIC APERTURE (inlet) to INFERIROR THORACIC aperture Between STERNUM (anterior) and the THORACIC VERTEBRAE (posterior) Content Trachea (Larynx to bifurcation into principle (R&L main) bronchi Oeseophagus (Pharynx to T10 Diaphragm) Heart & Pericardium Thoracic Duct (Cisterna Chyli to Left brachiocephalic vein) Nerves Great Vessels Divisions o o o o o Superior: above sternal angle Inferior: below sternal angle Anterior: anterior to heart in pericardial sac Middle: PERICARDIAL SAC & HEART Posterior: posterior to pericardial sac and diaphragm Content of Superior Mediastinum (A-P) Thymus Phrenic Nerves Great Veins Main Lymphatic Trunks Vagus Nerves Great Arteries Trachea & Main Bronchi Upper Oeseophagus ToP VaVLe GATO Great Veins: Subclavian Vein + Internal Jugular Vein = Brachiocephalic Vein Left Brachiocephalic Vein crosses POSTERIOR to Manubrium R & L Brachiocephalic Vein (Asymmetric) = Superior Vena Cava – Enters RA from above. Azygos Vein drains posterior wall of thorax & abdomen. pg. 8 S Tran o Arches over RIGHT LUNG ROOT into SVC IVC enters RA from below (through central tendon of diaphragm) Arteries: Ascending Aorta 1. R & L Coronary Arteries Arch of Aorta 1. Left Subclavian Artery 2. Left Common Carotid Artery 3. Branchiocephalic Trunk i. Right Common Carotid ii. Right Subclavian Artery Descending Aorta Aortic Arch arises ANTERIROR to Trachea. Arches OVER left main bronchus at lung root. Trachea lies behind & between brachiocephalic and left common carotid arteries. Common Carotids External & Internal Carotid Arteries Pulmonary Trunk Starts at RIGHT ventricle Deoxygenated blood to Lungs Divides into L & R Pulmonary Arteries Ligamentum arteriosum (previously: ductus arteriosus) connects PT to aortic arch. Phrenic Nerves C3, 4, 5 Motor to Diaphragm Sensory to: o Mediastinal Pleura o Pericardium o Peritoneum of Central Diaphragm RIGHT PHRENIC NERVE Right Brachiocephalic Vein Superior Vena Cava Right Side of Heart + Pericardium – In FRONT of lung root. LEFT PHRENIC NERVE Crosses left vagus to cross aortic arch more anteriorly Passes over Pericardium towards Diaphragm. RIGHT VAGUS NERVE Lies on Trachea pg. 9 S Tran Crosses BEHIND lung root Recurrent laryngeal branch – recurs around right subclavian artery Breaks into branches on the oesophagus LEFT VAGUS NERVE Lateral to Common Carotids Passes Anterior to Aortic Arch Crosses BEHIND lung root to form Recurrent Laryngeal Nerve around Ligamentum artiosum. Breaks into many branches around oesophagus pg. 10 S Tran Lecture 4: Nerves in the Thorax Somatic Nerves (Body) Necessary for skeletal muscle & skin. Sensory to body wall Segmental nerves combine to form PLEXI supplying specialised area (cervical, brachial, lumbosacral) Dermatome – Skin area supplied by a single spinal nerve on one side/single spinal cord Myotome - Skeletal muscle supplied by a single spinal nerve on one side/single spinal cord Intercostal Nerves: o 11 Pairs (+ 1 subcostal) o Mixed (Motor & Sensory) o Spinal/Segmental Nerves (Anterior Primary Rami) o Supplies intercostals spaces, lateral cutaneous branch (A&P), anterior cutaneous (Medial & Lateral) o Autonomic/Visceral – Organs & smooth muscles and glands. Phrenic Nerves: o Derived from Anterior Rami of C3-5 o No autonomic function/visceral distribution o Motor supply muscle of diaphragm o Sensory supply central diaphragm, mediastinal pleura and pericardium. o Supply peritoneum on interior surface of central diaphragm. Autonomic Nerves (Visceral) o o o Motor to Cardiac Muscle, Smooth Muscle and Glands Sensory to Visceral organs Parasympathetic & Sympathetic Parasympathetic Nerves 1. 2. 3. 4. Oculomotor (III) cranial nerves Facial (VII) cranial nerves Glossopharyngeal (IX) cranial nerves Vagus (X) cranial nerves pg. 11 S Tran 5. Sacral (S2 – S4) spinal nerves Visceral Sympathetic Trunks All autonomic pathways have preganlionic and postganlionic neurones. Branches from T1-L2 Sympathetic nerves to smooth muscle + glands Nerves to BODY WALL synapse in TRUNK GANGLIA Nerves to VISCERA synapse in LOCAL GANGLIA Pain Fibres back to CNS from viscera T5-T12 to abdomen in SPLANCHNIC NERVE bundles. Sympathetic to Lungs & Heart o o T2-T4 passes through cervical & upper thoracic ganglia of trunk Micro-ganglia synapses in pulmonary and cardiac plexuses Pulmonary Plexuses Sympathetic nerves DILATE bronchioles Parasympathetic nerves(vagus) CONSTRICT the bronchioles Cardiac plexuses Efferent Sympathetic efferents increase heart rate and force of contraction Parasympathetic efferents (vagus) decrease heart rate via the pacemaker tissue and constrict coronary arteries. Afferent Sympathetic afferents relay pain sensations from the heart Parasympathetic afferents (vagus) relay blood pressure and chemistry information from the heart Vagus Nerves Cranial nerve X – arise from medulla & leave skull through jugular foramina pg. 12 S Tran Descend neck posterolateral to common carotid arteries LEFT vague crosses ANTERIOR to aortic arch then posterior to left lung root RIGHT vagus passes posterior to right lung root Both Vagi form a plexus around the oesophagus Separates to form anterior and posterior oesophageal/gastric nerves Oesophageal plexus Sympathetic afferents relay pain sensation from oesophagus Parasympathetic afferents (vagus) senses normal physiological information from the oesophagus Vagus nerves To chest & abdomen are parasympathetic (smooth & cardiac muscle + glands of gut and airway) Large sensory (enteroceptor) content from gut and lungs No autonomic supply to body wall (e.g. arterioles & sweat glands) Recurrent laryngeal branch of vagus is NOT parasympatheteic – recurs up to the neck and supplies the skeletal muscles of the larynx. Oesophagus’plexus is supplied posteriorly by the right vagus. Acquire many sympathetic fibres Inferior continuation of the vagi takes the fibres through the diaphragm to the abdominal viscera Intrinsic nerves of the Oesophagus Plexus of ganglia and axons within the wall coordinate its activity Can be up or down-regulated by the autonomic nerves Part of the ENTERIC NERVOUS SYSTEM pg. 13 S Tran Lecture 5: Lymphatic System Why? More fluid leaves capillaries than returns to them. No fluid movement = oedema + loss of blood volume Lymphatic drains excess fluid Immunological significance Pathogens Hormones Cell Debris Fats Small Intestine: Fats absorbed into Chylomicrons (protein coated lipids) Released into interstitial fluid Drains into Lacteal (Lympathic capillaries) Returns to venous system via the neck Opaque and Milky – Chyle. pg. 14 S Tran Clear + Odourless in other vessels. Movement: Action of adjacent structures: Skeletal muscles + Pulses in arteries Valves ensure unidirectional Lymph Nodes Small (<2.5cm long) Found along lymph vessels Contain lymphocytes and macrophages Can act upon foreign bodies in the lymph Drainage from infected regions detectable in enlarged lymph nodes Armpit, groin, neck Lympathic Drainage Thoracic wall o Internal thoracic arteries (PARASTERNAL) o Bronchomediastinal Trunks o Ribs (INTERCOSTAL) o Upper –Bronchomediastinal Trunks o Lower – Thoracic Duct pg. 15 S Tran o Diaphragm (DIAPHRAGMATIC) o Branchiocephalic o Aortic/Lumbar o Superficial o Axillary or Parasternal The Thoracic Duct Main Drainage Channel Begins at Cisterna Chyli Begins at L2 Enters behind Oesophagus through diaphragm Ascends on right of midline – Between Aorta and Azygous Vein Crosses to Left at T5 Empties into LEFT BRACHIOCEPHALIC VEIN – Between left subclavian and internal jugular vein join. The Lungs TRACHEOBRONCHIAL Around Bronchi + Trachea From within lung through Hilum Unites with PARASTERNAL + BRACHIOCEPHALIC = BRONCHIOMEDIASTIUM(L & R) The Heart Follows coronary arteries into BRACHIOCEPHALIC TRACHEOBRONCHIAL The Posterior Mediastinum Nodes on Aorta receive lymph from oesophagus, diaphragm, liver and pericardium and drains into i. Thoracic duct ii. Posterior Mediastinal pg. 16 S Tran Lecture 6: Breast Anatomy Breast Development Mammary Ridge (Milk Ridges): 4th week Thickened strips of ectoderm Extend from axillary to inguinal region Normally only persist in pectoral area Mammary Gland 6th week Solid growths of EPIDERMIS into underlying meschencyme along mammary ridges. Primary Bud = Primordium of Mammary Gland o Gives rise to Secondanchry Bud o Secondary Bud develops into Lactiferous Ducts & branches Surrounding meschencyme o Gives rise to fibrous connective tissue and fat Epidermis at origin of mammary gland (Late Fetal Period) o Becomes indented/depressed = Mammary Pit = Nipple o At Birth: Nipples poorly formed & depressed o Nipples arise from proliferation of surrounding connective tissue of the areola Birth: Rudimentary mammary glands in M&F. Main lactiferous ducts formed. Possible “Witch’s milk” caused by transitory changes by maternal hormones Puberty: Fat & Connective Tissue Development Growth of duct system Pregnancy: Increase in Oestrogen & progesterone Intralobular ducts develop & form buds which become alveoli Abnormalities: Athelia: Absence of Nipples Amastia: Absence of Breasts Polymastia: Extra breast Polythelia: Extra Nipple pg. 17 S Tran Extra nipples and breast form along mammary ridges from extra mammary buds. Gynaecomastia: Excessive development of male breasts (Pathological or Physiological) Breast structures develop in both sexes Hormonal stimulus to grwoth during female puberty Extra nipples or pigmented skin along mammary line Hormones of pregnancy stimulate gland formation Breast Structure Breasts have an ‘Axillary Tail’ Muscle Beds underlying Breasts 1. Pectoralis major 2. Serratus anterior 3. External oblique pg. 18 S Tran Breasts in relation to the axillary walls 1. 2. 3. 4. Clavicle Anterior axillary fold – Pectoralis major Posterior Axillary fold – Latissimus dorsi Medial axillary wall – Serratus anterior Summary: 12-20 lactiferous ducts open separately on each nipple Lactiferous sinuses underlie areolae No glandular tissue in non-pregnant or nonlactating woman Most of non-pregnant breast is adipose tissue Breast supported by internal suspensory ligaments Artery Supply Lymph Draginage & Nodes Lymph drainage parallels blood supply Axillary and internal thoracic nodes are main normal routes Cancer can block drainage – raised lymph pressure forces lymph through unusual drainage route pg. 19 S Tran Nodes 6. 7. 8. 9. 10. Medial (Central) Lateral Anterior (Pectoral) Posterior Apical pg. 20 S Tran Lecture 7: Posterior Mediastinum Content: Oesophagus Descending aorta Thoracic duct Azygos venous system Posterior mediastinal lymph nodes Thoracic sympathetic trunks Splanchnic nerves Oesophagus Begins at C7 T7: o Bends Anteriorly o Stops being right of aorta o Deviates to the left o Gets progressively anterior to aorta Diaphragm at T10 Ends T11 Four Constrictions: o Oesophagus junction with PHARYNX o Crosses ARCH OF AORTA o Compressed by LEFT MAIN BRONCHUS o At the OESOPHAGEAL HIATUS Thirds Upper Middle Lower Artery Vein Lymph Length Inferior Thyroid Inferior Thyroid Deep Cervical 9cm Aortic Branches Azygos Branches Mediastinal 9cm Left Gastric Left Gastric Gastric 9cm Nerves within Inferior Mediastinum Phrenic (C3, 4, 5) – Anterior to lung roots then cross pericardium to diaphragm Vagi (Carnial Nerve X) – Posterior to lung root + form plexus following oesophagus into abdomen branches to heart and lung on the way. pg. 21 S Tran Sympathetic trunks lie each side of the posterior mediastinum Vagus Parasympathetic (Control smooth + cardiac muscle + glands of gut and airways) Large sensory from Gut and Lungs LEFT RECURRENT LARYNGEAL NERVE o NOT parasympathetic o Arch of Aorta starts o runs back up neck to supple larynx’s skeletal muscles Sympathetic Trunks Branches from T1-L2 Distribute sympathetic nerves to smooth muscle + glands Nerves to BODY WALL synapse in TRUNK GANGLIA Nerves to VISCERA synapse in LOCAL GANGLIA Pain Fibres back to CNS from viscera T5-T12 to abdomen in SPLANCHNIC NERVE bundles. Azygos Venous System o o o Drains posterior wall, upper abdomen and posterior mediastinal organs LEFT ACCESSORY HEMIAZYGOS VEIN (Upper) + HEMIAZYGOS VEIN (Lower) join single right Azygos Vein Azygos Vein arches over RIGHT LUNG ROOT to enter SVC above right atrium pg. 22