ORTHOPEDIC SPINE QUESTIONNAIRE
advertisement

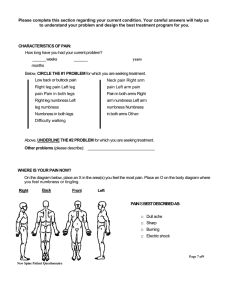
ORTHOPEDIC SPINE QUESTIONAIRE ( ==== PLEASE REPLACE THE TEXT IN BOLD ==== ) (Name of patient) is a (age), (gender), who is being evaluated today for a chief complaint (neck, mid back, low back) pain. They also complain of (no, right/left, arm/leg) pain. The nature of the spine pain is (localized, generalized, sharp, dull, spasms, fatigability). The extremity pain is described as being (nothing significant, numbness, tingling, weakness, heaviness, burning, sharp electrical, dull) pain. The severity of the pain is described as (mild, moderate, severe), and they rate the pain on a scale of 1 to 10 as being (1 through 10). The timing of the symptoms is (intermittent, episodic, constant) and felt on a (daily, weekly, monthly, yearly) basis. The duration of these symptoms has lasted for (days, weeks, months, years). The pain started (suddenly, over a period of time, with no particular beginning). There was (no, an) event that started this process. (The description of the trauma should be a sentence the patient needs to put in at this last sentence.) This (has, has not) happened before, and the symptoms are (less than before, the same as before, more severe than prior). There has been (no, one, several) spine surgeries prior to this event. (First name of the patient) experiences pain traveling away from spine (yes, no), and the pain travels (in the arms/legs, right/left, both). The patient experiences numbness in the (small finger, long finger, thumb, forearm, upper arm or the big toe, the small toe, the feet, the shin, the calf, the thigh). The patient feels weakness (yes or no) in the (arms/legs, right/left, both). (Patient name) experiences (no difficulty or difficulty) walking because of loss of coordination or dexterity. The patient (deny, admit to) loss of control of urination or bowel movements. The aggravating factors for the pain are (standing, sitting, walking, changing position, lifting, bending). Improvement factors are (sitting, walking, exercising, medications). In order to deal with the problem, the patient (has or has not) tried medications, and they have been found to (help, not help). Physical therapy (has, has not) been tried, and this has been found to (help a little, help a great deal, help only on a temporary basis). Chiropractic care (has, has not) been tried and is found to provide (good, mild, no) benefit. The patient (has, has not) had any specific cortisone injections done for the treatment of the spine, and these have proven to be of (no, short-term, significant) benefit. Surgery (has, has not) been tried and has made things (better, unchanged, worse). Past medical history should be a standard intake sheet. Just make sure the review of symptoms includes (1) temporomandibular joint pain; (2) fibromyalgia; (3) headaches; (4) irritable bowel; (5) depression with all of the review of systems issues.