Preliminary Testing

Preliminary Testing
Visual Acuity o Purposes:
To establish a baseline
Legal reasons (driver’s licenses, insurance claim, pension, and disability based on legal blindness)
Legal blindness: 20/200 or worse in better eye OR less than 30 of visual field in the widest meridian of the better eye
Monitor progression or improvement of eye disease
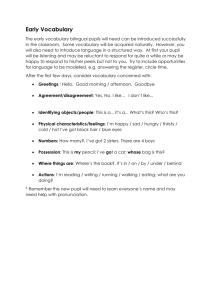
Guide for the rest of the exam (prediction of refractive error, correlation of data, determines additional testing) o Always the first test performed after history
Exception: chemical burn/spill; irrigate first, then check VA o Definition: the resolving power of the eye, or the ability to see two objects as separate
“Normal” resolving power is defined as the ability to detect a gap with a width of 1 min of arc o VA is highest at the fovea and decreases with increasing retinal eccentricity o VA best if pupil is 2-5 mm o Types
Minimum Detectable Resolution (minimum visible): the ability to distinguish an object from its background
Minimum Separable Resolution (minimum resolvable): the ability to resolve two or more spatially separated targets
Gratings, bars, Vernier acuity, preferential looking
Recognition Resolution (minimum legible): the ability to recognize letters, numbers, and geometric forms
Snellen, Landolt C, Tumbling E o Snellen acuity chart is the universal method of measuring VA
Snellen optotypes: width of each stroke is equal to the width of a gap on that line
“Best” letter is E (3 strokes and 2 gaps)
“Not as good” letters are T and L ( no gaps)
At 20 feet, a 20 foot optotype subtends 5 min of arc
Its details each subtend 1 min of arc
20/20 letter is defined as a letter that has a height (x) such that it subtends
5’ arc at 20 ft
Letter height can be altered with test distance
Details (gaps and strokes) each subtend 1’ arc at 20 ft
Utilizes a “folded” room/operatory system
Projector with letters, 2 mirrors and a screen
Test distance= patient to mirror + mirror to screen o MAR (minimum angle of resolution) in minutes of arc is equal to the reciprocal of the decimal acuity value or the Snellen fraction
Snellen fraction = 1/MAR
20 ft (6m) is considered optical infinity, which is defined as the distance at which no accommodation is being used
Snellen fraction = testing distance distance at which the smallest letter read subtends an angle of 5’ of arc
Also described as the distance at which a “normal” eye can see the smallest letter read by this patient o Snellen equivalent is used when VA is taken at a distance other than 20 ft or when other nomenclature is used
It is better to report the actual acuity, not the equivalent o Limitations:
Number of letters tested per line changes as you move down
Letter sizes between lines do not change by a constant ratio
Between row and between letter spacing is not proportional to the letter size
Legibility for optotypes often varies o Standard Chart Specifications
Chart luminance: at least 10 foot lamberts
Chart contrast: at least 90%
Subdued room illumination to enhance chart contrast
Uncorrected refractive error is more likely to impact VA when pupils are slightly dilated o Distance VA should be performed during ALL patient encounters
Procedure
Seat patient comfortably and dim lighting
VAs taken without correction(sc) and then with correction(cc) o Minimizes chance of patient memorizing
Clean occluder with alcohol swab
Begin with full chart open and ask “Which of these is the smallest line of letters that you can read?”
Isolate smallest LOL that the patient can read; continue to scroll down to the next LOL and have patient read it; stop when the patient is unable to read the entire LOL o Find the patient’s threshold
OBSERVE the patient (no squinting, cheating, leaning forward, etc) o Observe the speed and degree of difficulty
Record VA as the smallest line in which not more than 2 letters were missed for OD, OS, OU o The number at the end of each line signifies the level of acuity o Some use several 20/20 lines to minimize memorization o “normal” best-corrected VA is 20/20
Corrected visual acuity (best corrected VA) is measured with the best refractive correction in place
Habitual visual acuity is measured with patient’s own spectacles/CLs o Near VA performed during full/comprehensive exam and if they have a near vision complaint
Procedure
Use full illumination: stand lamp on recording card
Done without, then with near correction
Measure the distance from the patient’s spectacle plane to the reading card in cm
Cover OS and instruct to “Read the smallest paragraph that you are able to”, switch to cover OD, and then remove to read with both eyes open
Re-measure the working distance with their correction
Record working distance (in meters!) over the smallest print read for
OD, OS, OU
M system: a 1M letter subtends 5’ of arc at 1 meter
Allows patient to hold card at their desired reading distance
Reduced Snellen system: gives the appearance of expressing the distance
VA that is equivalent to the near VA
Should NOT be used for near VA (not appropriate to use a term that suggests a test at 20 ft when that distance is not relevant to near vision)
Jaeger system: indicates the size of the print by the letter J followed by a number
Poor system because there is no standardization of the Jaeger sizes and there is no intrinsic meaning to the “J” number o Pinhole testing: a measure of potential visual acuity
Nullifies small amounts of refractive error by 1) increasing the depth of focus and 2) decreasing the size of the blur circles
Most effective diameter is 1.32 mm
If VA improves with pinhole, suggests that refractive error is probably the cause of the reduced VA
Done when entering acuities are 20/40 or worse (based on better VA)
Record PH followed by VA obtained
If no improvement, record PHNI
Super Pinhole, PAM (potential acuity measure) and laser interferometer are commonly used to determine potential VA before cataract surgery o Brightness Acuity Test (BAT): used when you suspect acuity would be worse in a glare situation
VA with BAT is worse than without BAT for patients who have glare problems o Alternative distance VA charts
OKN drum: cortical function only; objective test
Teller acuity cards: infants, non-responsive patients
Tumbling E: preschool, illiterate or non-verbal patients
LEA chart: children
Allen figures: children
Landolt C:
HOTV chart: amblyopes
Each letter is surrounded by crowding bars
Amblyopia: decreased VA (not correctable to 20/20) NOT due to pathology o Snellen chart produces contour interactions (slow responses, some correct responses over a wide range of letter sizes, correct end-letter responses, out of order responses, perform better with isolated lines or letters)
Feinbloom chart: patients unable to see the 20/400 E on Snellen
Full illumination and test distance of 5 or 7 ft
Record test distance over smallest number size seen o Alternative near VA charts (used during low vision)
Bailey-Love Chart: patients unable to see large print on other cards
Space between the letters is equal to the letter width (prevents crowding effect)
5 letters on each line
Between row spacing is equal to the height of the letters in the smaller row
Lighthouse cards o Other measures of VA
Light perception (performed at ~ 1 ft)
LPP: light perception with projection
LPO: light perception only
NLP: no light perception
Hand motion (used as last ditch effort when Feinbloom efforts exhausted)
Count Fingers
“Fix and follow”: unresponsive patients
MUST ALWAYS ATTEMPT TAKING VISUAL ACUITIES o Correlation of VA and refractive error
General rule: each 0.25DS of uncorrected refractive error accounts for ~ 1 line of Snellen VA
For cylinder, take spherical equivalent (sphere + ½ cyl)
For oblique axis, add a line for the axis
Patient must have NO accommodation or be cyclopleged
Pupil Testing o Pupil performs 3 primary functions
Controls entering light
Modifies depth of focus (inverse relationship)
Smaller pupil increases depth of focus
Varies optical aberrations (smaller has less aberrations) o Should be performed during ANY patient encounter regarding eye health
Important because it is a neurological test that can detect optic nerve disease, brain mass and aneurysm
Gross examination can detect iris abnormalities, media opacities, and o Shape leukocoria
Pupils should round and centered within the iris on optic axis
Irides should be of the same color
Abnormalities o Corectopia: displaced or misshapen pupil o Ectopic pupil: significantly decentered o Polycoria: more than one pupil o Heterochromia: iris color different between eyes or between different areas in one eye o Aniridia: absence of iris, therefore non-existent pupil o Size
Average of 3.5 mm in adults under normal illumination
Become smaller after adolescence due to senile miosis
Should equal one another within 1 mm
Anisocoria: unequal pupil size
20 % have physiologic anisocoria
Controlled by the autonomic nervous system
Iris dilator muscle dilates; sympathetic innervation
Iris sphincter muscle constricts; parasympathetic innervation o Pupillary pathways
Afferent
Light enters pupil impulse in retina (PR and ganglion cells) optic nerve optic chiasm: ½ cross, ½ ipsilateral optic tracts to superior colliculi pretectal nuclei of hypothalamus crossed and uncrossed fibers to EW synapse with efferent fibers
Parasympathetic efferent
From EW nucleus travels with CN III (inferior division) cavernous sinus pierces globe deviates from CN III and synapses at ciliary ganglion postganglionic fibers reach iris sphincter via short ciliary nerves o 97 % of the fibers control accommodation (ciliary body) o Only 3 % innervate the sphincter
Sympathetic efferent
Hypothalamus synapses at ciliospinal center of Budge (C8-T4)
2 nd order neurons leave spinal cord ascending close to the apex of lung synapses at superior cervical ganglion 3 rd order neurons follow the ICA’s to the globe iris dilator via the long ciliary nerves
Sympathetic innervation reaches Muller’s muscle in upper lids o Response to light
Miosis (=constriction) occurs via parasympathetic innervation
Some latency in initial constriction is normal (depends on brightness and age)
Direct response: response that occurs in one eye while the light is shone in that eye
Consensual response: response that occurs in one eye while the light is shone in the other eye
Pupillary escape: gradual and partial re-dilation without change in light intensity
Pupillary unrest or hippus: small oscillations in pupillary diameter that occur during maintained stimulation
Due to normal fluctuation in sym/parasym equilibrium o Response to near
Independent of retinal illumination
Near reflex is ALWAYS present when direct light reflex is intact
Near triad: pupil constriction, convergence, accommodation o Swinging flashlight test
Compares the strength of the direct pupillary response with that of the consensual response
Detects afferent pupillary defect due to retinal abnormalities or optic nerve pathway anterior to LGN (APD or RAPD) o Procedure
Remove spectacles and examiner positioned off to one side
Use a distant, non-accommodative target (2-3 lines above VA)
Measure pupil size under normal lighting conditions
Expected findings: should equal one another o Size in bright: 2-4mm Size in dark: 4-8mm
If pupils are unequal, measure size in both dark and bright light
To visualize dark irides, use: o Burton lamp: hold ~25 cm (10in) from the patients and below the patient’s line of sight o Ophthalmoscope: use as a dim flashlight to illuminate both eyes simultaneously (“light from below”)
Judge the roundness of each pupil and describe any abnormalities
Observe pupil’s response to light in dim illumination
Note the magnitude of change (quantity) using scale 0-3
Note the rapidity of reaction (quality) using slow (-) or fast (+)
Expected findings o Direct response of OD should equal direct response of OS o Consensual response of OD should equal consensual response of OS o Direct response of OD should equal consensual response of
OD
Perform the swinging flashlight test
Expected findings o Rate and amount of constriction should be the same for both pupils o Direct should equal consensual for both eyes
If it is not the case for either eye: afferent pupillary defect in the eye with less constriction
Record using PERRLA (-) APD if all reflexes are normal
PE: pupils equal
R: round
RL: reactive to light (direct and consensual)
A: responsive to accommodation
(-) APD: no APD o Afferent pupil anomalies result in an APD
Severe retinal disease, optic nerve diseases or compromise, mass/lesion behind eye compressing optic nerve or chiasm
NOT with disorders of ocular media
Afferent pupillary defect (RAPD) indicates unilateral or asymmetric damage to the anterior visual pathways
When the consensual response is greater than the direct response of one eye
If present, pupils of both eyes will constrict less when the light is directed into the affected eye o Both eyes will constrict when light beam directed into unaffected eye
When light beam is directed in affected eye, causes less constriction in o Affected eye: reduced direct reflex o Unaffected eye: reduced consensual reflex
Graded from trace to 4+ o 3-4+APD: immediate dilation of the pupil, instead of initial/equal constriction o 1-2+APD: no change in pupil size immediately, followed by dilation o Trace APD: initial constriction, but greater escape to a larger intermediate size than when light is swung back to normal eye
Amaurotic Pupil: severe or 4+APD
Patients have an eye with “NLP”
Light beam directed into affected eye no direct response in affected eye and no consensual response in unaffected
Light beam directed into unaffected eye direct response in unaffected eye and consensual response in affected eye
Near reflexes will be intact
Reverse (indirect) APD
Performed when one pupil is fixed, dilated, or constricted o ONLY observe the reactive pupil
If APD in eye with reactive pupil, that pupil will constrict more with consensual stimulation than with direct
If APD in eye with fixed pupil, the reactive pupil will constrict more with direct stimulation than with consensual
Note reverse APD (implies you used a reverse technique) o Efferent pupil anomalies: unilateral defects/lesions will often generate anisocoria
Anisocoria: usually 2-4 mm difference in dark and light
If same degree of anisocoria in light and dark: physiologic
Big pupil problems: anisocoria greater under bright conditions due to a defect/lesion of the parasympathetic
Adie’s tonic pupil o Relatively common; primarily in females 20-40
o Presentation
Unilateral semi-dilated pupil
Pupil with minimal and slow reaction to light
Pupil with reduced direct, consensual (poor constriction of sphincter) and near responses to light
May present with a reduced near vision complaint
Vermiform motion of iris: quivering motion of iris at pupillary border due to segmental palsy of sphincter
10-20% eventually affecting other eye
Reduced direct response to light bilaterally
Decreased near VA
Prolonged pupil cycle time o Etiology
Lesion of the parasympathetic pathway (ciliary ganglion) on the side of the pupil problem
Viral o Diagnosis
0.125% pilocarpine (wait 10-15 min)
Constriction: Adie’s confirmed
No constriction: either pharmacologic or 3 rd o Management nerve
Rule other orbital and ocular conditions
Cosmesis
Accommodation
Near add, sometimes unequal adds
Equalize accommodation during refraction and other near or binocular testing
Accommodation generally returns within 2 yrs
Cranial Nerve Palsy o Presentation
EOM paresis—exotropia and hypertropia (“down and out”) of eye affected
Ptosis
Fixed and dilated pupil, or non-reactive pupil o Etiology
Pupil fibers are on the outside of CN III; they are involved early in a compressive lesion and are rarely involved in an ischemic infarction
Lesions that involve the pupil: tumor and aneurysm
Lesions that spare the pupil: vascular disease causing ischemia (diabetes, hypertension) o Diagnosis
0.125% pilocarpine—will NOT constrict
1% pilocarpine—WILL constrict o Management
Presentation of acute 3 rd nerve palsy with pupil involvement considered a medical emergency!
Manage diplopia and systemic cause of palsy
Pharmacologic anisocoria: dilation of one eye o Presentation
Usually unilateral, fixed and dilated pupil
Anticholinergic substances block the action of acetylcholine on the ciliary muscle and cause mydriasis o Etiology
Scopolamine
Jimsonweed
Antihistamine drops
Atropine, homatropine, cyclopentalate o Diagnosis
0.125% pilocarpine—Will NOT constrict
1% pilocarpine—Will NOT constrict o Management
Reassurance and patient education
Little pupil problems: anisocoria is greater in dim conditions due to a defect/lesion to the sympathetic nervous system
Horner’s syndrome o Presentation
Miosis (can be mild: less than 1 mm of anisocoria)
Ptosis
Anhydrosis
***All on the same side as the lesion*** o Etiology
Interruption of the sympathetic system anywhere in its path
Congenital Horner’s: idiopathic or trauma at birth
Heterochromia and anhydrosis
Central lesions: stroke, MS, spinal cord cancer, neck trauma
Preganglionic lesions: pancoast tumor, trauma, thyroid enlargement or lesion
Postganglionic lesions: extracranial or intracranial cause (Raeder’s, ICA dissection, complicated otitis media) o Diagnosis
Look at old photographs
History of trauma, endardectomy, thyroidectomy?
Dilation lag test
Take picture immediately after turning off lights and take another picture 15 seconds
Horner’s pupil has a dilation lag in the dark of
~15 sec
0.5% Apraclonidine (Iopidine) (wait 15-30 min)
Dilates: confirms diagnosis of Horner’s
10% Cocaine drop in affected pupil (wait 15 min)
Does NOT dilate: confirms diagnosis of Horner’s o Management
Important to determine before or after the bifurcation of the carotid artery
Differentiate by testing for anhydrosis (prism bar test and corn starch under heat lamp)
Postganglionic lesions generally do not cause anhydrosis
1 % hydroxyamphetamine (done 48 hrs after cocaine test) o Dilation: central or preganglionic lesion o No dilation: postganglionic (“fail safe” affected pupil fails to dilate)
Argyll-Robertson pupil o Presentation
Bilaterally miotic, irregular pupils
Difficult to dilate
Direct and consensual responses absent or sluggish in affected eye(s)
DOES react to near (there is light-near dissociation) o Etiology
Midbrain lesion
Neurosyphilis or neuropathy from diabetes, alcoholism
Pharmacologic anisocoria: constriction of one eye o Cholinergic agents: pilocarpine (glaucoma drop) and physostigmine o Near-Light Dissociation: pupils fail to respond to light, but near response intact
Afferent pathways interrupted, efferent pathways intact
Examples of conditions that manifest near-light dissociation
Neurosyphilis: Argyll-Robertson pupil
APD or amaurotic pupil
Aberrant regenerations o Pupil Irregularities
Aniridia: congenital absence of the iris (usually bilateral)
Iris coloboma (“keyhole” pupil)
Usually involves the inferior nasal portion of the iris
Wider at the pupillary margin than at the iris root
Corectopia: displaced pupil (frequently bilateral)
May be displaced in any direction
Iridectomy: surgically created sector cut of the iris
Iris atrophy
From age, inflammation, ischemia, trauma
Iris holes may form creating polycoria
May be sectoral (herpes zoster) or widespread
Iris cysts/tumors
If extensive enough, may distort pupillary margins
Laser iridotomy: hole created in iris usually located superiorly at 10:00 or
12:00
Shape of the pupil usually not affected
Persistent pupillary membrane (PPM): persistent embryolic structure
Rarely affects pupillary movement
Trauma
Tears of pupillary margin and sphincter o Traumatic mydriasis and abnormal pupil light reflexes permanent
Iridodialysis o Tear at the iris root; D-shaped pupil o Monocular diplopia may occur
Posterior synechia: attachment of iris to anterior lens surface from active or history of anterior uveitis or intraocular inflammation
Iridonesis: quivering of the iris
Pupillary margins are irregular and reactivity will be reduced
Seen in aphakic patients o Pharmacologic dilation (bilateral)
Anticholinergics
Antihistamines
CNS depressants
Sympathomimetis and CNS stimulants (bind with alpha receptors on dilator muscle to cause mydriasis)
Epinephrine, Cocaine, amphetamines o Pharmacologic constriction (bilateral)
Barbituates
Opioids
Levodopa
Marijuana
Vitamin A
EOM Testing o Saccades
Rapid abrupt conjugate movement; stimulated by alternately fixating objects
Can be voluntary or reflex o Pursuits (Versions)
Slower smooth conjugate movements; stimulated by target movements
Used to test binocular, conjugate movements of the eyes allowing the lines of sight (LOS) to move in a parallel direction (or fixed angle) o EOM
Innervation
CN VI (abducens): LR
CN IV (trochlear): SO
CN III (oculomotor): MR, SR, IR, IO
Planes of action
LR and MR: horizontal plane
SR and IR: vertical plane, 23-25° temporal
SO and IO: vertical plane, 51-53° nasal
Muscle paresis is most obvious when the LOS is directed to move the eye in the direction of its primary action within its plane of action
Synergistic muscles: muscles in same eye that assist in an action
Antagonistic muscles: muscles in same eye that have opposite actions
Yoked muscles: neurologically paired in opposite eyes
Hering’s Law of Equal Innervation o Procedure
Remove spectacles and use high illumination
Fixation target held ~40 cm from patient’s eyes
Instruct patient to follow light as its moved in “H” pattern
Make sure you test to the extreme field of gaze (limit of the EOM)
Note any overactions (+) or underactions (-); perform ductions
Ductions are monocular eye movements into the 6 cardinal positions of gaze
Identifies the faulty muscle(s)
Can test each muscle in its field/plane of action
Parks 3-step used for hyper deviations to determine faulty muscle
Record EOM: full and smooth (F and S)
FROM: full range of motion
SAFE: smooth accurate full extent
** Also record if ductions=versions, etc**
Stereopsis o Stereopsis: the perception of 3-D visual space due to binocular disparity cues
(disparities of the two retinal images) o Stereoacuity: ability to discriminate very fine differences of objects in space by using binocular vision
Stereo acuity is not the same as depth perception
Must have some level of binocular vision to appreciate stereo acuity
Requires changes in both vergence and accommodation o Monocular cues to depth perception must be learned
Retinal image size, linear perspective, texture density, luminance variations, aerial perspective, overlay, motion parallax, kinetic depth, myosensory cues from muscles controlling accommodation and convergence o Each point on the retina has a local sign or directional value
Fovea: principal visual sign (straight ahead)
Corresponding retinal points: pairs of points in each eye that have the same local sign (point in one eye corresponds to an area in the other eye)
Objects that stimulate a pair of corresponding points appear to be single and located at the same position in space o Stereo Tests Designs
Local stereopsis (line or contour)
Targets have edges that are separated on background to produce disparity
Smaller separation defines better stereopsis
Howard Dolman Peg Test o Thresholds stereopsis o Most accurate o Two types of testing: null threshold and JND
Titmus Stereofly o Linear polarized test o 3 parts: “fly” for gross stereo (3,000’’), “animal” test (400’’-
100’’), Wirt circles (800’’-40’’)
Stereo Reindeer
Global stereopsis
Matrix of black dots on gray background
Lateral shift in central pattern
NO monocular cues
Random Dot o Uses 3-D cross polarized spectacles o Right side: 8 random dot figures-- 500 sec of arc on top and
250 sec of arc on bottom-----must identify which cell is empty o Left side: modified circles (400’’ – 20’’), animals (400’’ – 100’’) o Procedure
Present test perpendicular to LOS at a distance of 40 cm (16 in)**
Spectacles are placed over habitual
Score last number correct after 2 errors
Record sec of arc @ test distance, test used and note cc or sc
Color Vision o Three types of cones responsible for color vision
Each contain photopigments that maximally absorb different wavelengths
Red (long), green (middle), blue (short) o Defects
Protan: red wavelength (L cones)
Deutan: green wavelength (M cones)
Tritan: blue wavelength (S cones) o Inherited color deficiencies
Anomalous trichromat (3 cone pigments)
Protananolmalous: red weak
Deutananolmalous: green weak
Tritananolmalous: blue weak
Dichromat ( 2 cone pigments)
Protanopia
Deutanopia
Tritanopia
Monochromat
Rod
o True color blindness (may have few cones but abnormal in shape) and poor vision
Cone o Variation of color blindness (only one cone type present)
Inherited
Permanent (not correctable)
Acquired
Changes with progression or regression of primary cause
Test result relatively stable Test results strongly influenced with changes in test conditions
Defect same in each eye in both type and severity
More prevalent in males
Always binocular
Almost always red/green
Severity may be greater in one eye, or one eye could be normal and the other not
Equally prevalent in males and females
Can affect only one eye
Most are blue/yellow
Transmitted via X chromosome Caused by medications (plaquinel), disease, toxic effects of chemicals, aging o Prevalence
Overall 4%
Males 8% o Protanomaly 1% Protanopia 1% o Deuteranolamly 5% Deutranopia 1.1% o Tritanopia 0.002%
Females 0.5% o Patient selection
Children at an early age
Patients at initial office visit
Unexplained decreased in VA
Report changes in color vision
Abnormal fundus findings o Types of color vision tests
Color Naming
Color Mixing
Anomaloscope o Assess ability to make metameric matches o Change mixture of monochromatic red and green
Color Confusion
Pseudoisochromatic plates (PIC) o Diagnostic plates: figure is isochromatic for one defect but not for another so it identifies type of deficiency o Vanishing figure: normal sees, defective does not see o Transformation: normal and defective see different figures o Hidden digit/symbol: defective sees, normal does not see o Screening mostly for inherited defects
HRR o Detects inherited and acquired defects o Can be used on illiterate patients (symbols used)
Ishihara o Screen for inherited red/green anomalies
Color Matching (arrangement)
Detects inherited or acquired
Farnsworth D-15 o Quantifies depth of defect (mild/severe) o Used only as diagnostic (not screener)
Farnsworth-Munsell 100-Hue o Good for detecting/classifying early acquired color deficiencies caused by ocular disease o Detects subtle color discrimination
Occupational
PIC, D-15, Farnsworth Lantern test (FALANT), ISCC Color Matching
Aptitude test o Procedure
Use “standard” illumination “C”
MacBeth Easel Lamp
Incandescent lighting inadequate
HRR
Plates perpendicular to LOS at 75 cm
Use correction unless tinted and test monocular!
Ask patient how many symbols, what are they, and have trace where they are with brush
Time limit: 20 sec/page
Record check marks when correct for screening plates 5-10 o If ALL 6 correct: normal CV o Only plate 5 or 6 missed test plates 21-24: B/Y defect o Only 1 or more plates 7-10 missed test plates 11-20: R/G defect
Ishihara
Plates perpendicular to LOS at 75 cm
Use correction unless tinted and test monocular!
Ask patient what do they see
Time limit: 3 sec/plate
Record number plates correct over number tested with pass/fail noted and the numbers said if missed o Normal if 10/1l o If </= 7 correct, test plates 12,13,14 to classify whether protan or deutan
Farnsworth D-15
Caps should be 45 deg to patient’s LOS at 50 cm
Use correction unless tinted and test monocular
Instruct patient to place caps in chromatic order
No time limit
**When recording, note the test used and if cc or sc** o Management
Rod chromatism (poor VA and photophobia)
Tinted lenses (red and amber) to obtain low scotopic luminance transmittance but decreased visibility in short wavelengths
Acquired defects should be directed to cause
Inherited defects: counseling, career limitations
Cover Test o Fusion: both eyes are looking at the same target at the same time o Alignment
Orthophoria (ortho): “normal”, both eyes fixate on the same spot even after you break fusion o Misalignment
Tropia (strabismus): manifest deviation of the line of sight of one eye
The LOS of one eye is directed toward the object and the LOS of the other eye is directed elsewhere
If the eye is misaligned outward it is called exotropia o Will move in when the other eye is covered
If the eye is misaligned inward it is called esotropia o Will move out when the other eye is covered
If the eye is misaligned upward it is called hypertropia o Will move down when the other eye is covered
If the eye is misaligned downward it is called hypotropia o Will move up when the other eye is covered
Patient may have symptoms such as double vision, eye strain, headaches, fatigue, and reduced stereo
Phoria: latent deviation of the LOS
Eye aligned except when fusion is disrupted o Bruchner: observe the red reflex from the retina with the ophthalmoscope to detect leukocoria, strabismus, or anisometropia o Hirschburg: use the transilluminator to find the corneal light reflex
To see 1 mm, patient must have 22 diopters o Krimsky: perform Hirschburg and line up the corneal light reflex with prism o Cover Test: objective test to determine the presence, amount, and direction of misalignment
Unilateral cover test (cover-uncover): detects tropia
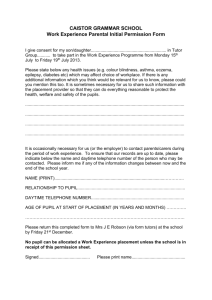
Alternating cover test: to detect phoria and measure amount of tropia o Procedure
Unilateral
Distance: patient fixates on a letter that is one line larger than the best VA of the worst eye
Near: patient uses a fixation stick with a small accommodative target o Done at 40 cm or working distance
Important to come from the nose
Clinician covers OD and watches OS for movement; then covers OS and watches OD for movement o Presence of movement indicates strabismus or tropia
Alternating
Patient still fixates a target
Clinician covers OD for 2 sec, then swings cover paddle from one eye to next
Do NOT allow patient to view with both eyes at the same time o Presence of movement on alternating but not on unilateral indicates phoria o If there is movement on both unilateral and alternating, it is a tropia (tropia trumps a phoria) o If there is no movement on both unilateral and alternating, check with 4 BI and 4 BO and there should be equal and opposite movements o Measuring magnitude
Prisms deviate the image towards the apex
‘Exos’ need the image sent OUT---- use base IN
‘Esos’ need the image sent IN---- use base OUT
‘Hypers’ need the image sent UP---- use base DOWN
‘Hypos’ need the image sent DOWN---- use base UP
Procedure
Put the prism behind the cover paddle and place in front of the eye at the same time o For eso and exo, put prism in front of either eye o For hyper and hypo, put prism in front of deviated eye
Move occluder to other eye without allowing binocular fixation
Increase prism amount without allowing binocular fixation until movement stops=neutrality
Continue to increase amount until the direction of the movement reverses o Recording
Record amount of prism that resulted in neutrality before reversal
Orthophoria (lack of manifest or latent deviation)
Horizontally ortho
Vertically ortho
Ortho both horizontally and vertically
Magnitude: prism diopters
Direction: exo (X), eso (E), hyper, hypo*
Only name the hypo eye if it also has a horizontal constant tropia
Laterality: right (R), left (L), alternating (A)
Note the fixation preference
Frequency: constant (C) or intermittent (I)
If intermittent, write down percentage
Nature: comitant or incomitant
Use 9-gaze test or Park’s 3-step test
Also note: Testing distance, cc or sc
Normal: Distance 1 XP + 2 Near 3 XP + 3
o Duane’s Classifications
Basic: <8 Δ difference between distance and near
Distance vs. Near Deviations
Convergence Insufficiency o Exo at near > distance
Convergence Excess o Eso at near > distance
Divergence Insufficiency o Eso at distance > near
Divergence Excess o Exo at distance > near
Blood Pressure o Important to do routine BP measurements:
Elevated blood pressure increase the risk of coronary heart disease, stroke, and kidney failure
“Silent killer” since you cannot tell by the way you feel
Patients will often seek eye care before other health care
HTN can result in significant visual morbidity o Risk Factors for HTN
Smoking, high cholesterol, obesity, diabetes, age (elderly), family history, race (African-Americans), gender (male) and stress o Systolic pressure: ventricular contraction o Diastolic pressure: ventricular relaxation o Korotkoff Sounds
Phase 1: appearance of clear taping sounds (systolic)
Phase 2: swishing of sounds
Phase 3: increase clear sounds, increase intensity
Phase 4: abrupt muffling of sounds (diastolic I)
Phase 5: complete disappearance of sound (diastolic II)
Auscultatory gap: early, temporary disappearance of sound between phase
1 and 2 that can cause serious underestimation of systolic (or overestimation of diastolic pressure) o Procedure
Patient should be seated and relaxed with legs uncrossed
Patient’s arm should be slightly bent, resting on the arm rest with palm up and unrestricted baring of arm
Palpate for systolic pressure
Place cuff ~1’’ above antecubital crease
Palpate the radial artery at wrist using fore finger and middle finger
Inflate cuff to ~30mmHg above level at which the pulse disappears
Note reading and deflate cuff
Place diaphragm over brachial artery between the crease and the lower edge of the cuff
Inflate cuff to 30 mmHg above systolic (determined by palpation)
Deflate at a rate of 2-3 mmHg/sec
Listen for phase 1 sound (regular tapping sound)
Note reading: systolic pressure
Continue deflation and listen for phase 5 (complete disappearance of sound)
Note reading: diastolic pressure
If sounds are too weak, ask patient to open and clench fist ~10x or inflate cuff quickly
Repeated inflation will cause venous engorgement and decrease sounds
Deflate cuff and remove
Record: systolic/ diastolic, arm used, posture, time of day, and cuff size if other than regular o Sources of Error
Falsely High
Brachial artery below heart level
Asucultatory gap (diastolic)
Cuff too small
Anxiety or fear
Isolated sources: anxiety, stress, recent exertion, pain, caffeine
Falsely Low
Brachial artery above heart level
Asucultatory gap (systolic)
Cuff too large
Deflating too rapidly
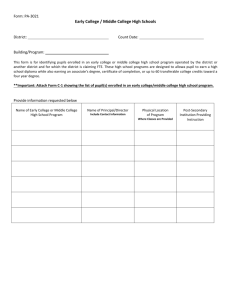
Hypertension Classification
Stage I Stage II Pressure
Systolic
Diastolic
Normal BP
< 120
< 80
Referral Guidelines
Initial Screening Blood Pressure
(mmHg)
Systolic Diastolic
Prehypertension
120-139
80-89
<130
130-139
140-159
<85
85-89
90-99
140-159
90-99
> 160
> 100
Follow-Up Recommended
Recheck in 2 yrs
Recheck in 1 yr
Confirm within 2 months
160-179
180-209
> 210
100-109
110-119
> 120
Evaluate or refer to source of care within 1mo
Evaluate or refer to source of care within 1 wk
Evaluate or refer to source of care immediately
Confrontation Visual Fields o Visual field: the perceptual space available to the fixating eye o Purpose: to provide a gross check for any defects in the peripheral visual field o Extinction phenomenon
Patients with right parietal lesions can exhibit a form of visual extinction.
When shown two objects, one contralateral (left) and one ipsilateral (right) to the lesioned hemisphere, subject will report seeing only the one in the ipsilateral (right) field o Riddoch’s phenomenon
Some patients with neurological defects suffer from stato-kinetic dissociation
Moving objects are perceived better than static ones
Defects present on automated perimetry (static) tend to be more extensive compared to those measured by manual perimetry (kinetic) o Finger counting
Tests the patient’s ability to correctly identify gross targets in each of the 4 major quadrants
Procedure
Examiner and patient remove spectacles
Sit at eye level and 1m away
Have patient occlude OS with palm of their hand and fixates clinician’s OS with their OD (clinician’s visual field corresponds to the patient’s)
Place one hand in the mid-plane (50 cm) at about 45° from fixation o Important to be exactly between you and the patient so the patient’s field can be compared to yours
Fingers more than 50 cm from patient patient’s field will be underestimated/constricted
Fingers are less than 50 cm from patient field will appear to be normal but you may be more likely to miss a defect/constriction
Present one, two, or four fingers in one of the four quadrants
Repeat for other 3 quadrants
Present both hands simultaneously in both superior quadrants
Present the fingers of both hands and ask patient to add together o Do NOT use the same numbers in each hand
Repeat for OS
Record normal fields as FTFC (full to finger counting) OD, OS o If not full, then document/draw constricted quadrant
Advantages
Sensitive to homonymous (neurologic) quadrantic and hemianopic
VF defects
Fast and can be performed in any location
Can test for extinction phenomenon
Disadvantages
Results are not meaningful to the DMV
Sensitivity is not very high
Limits of the VF are not tested o Field Limits
Compares known peripheral field limits to the patient’s peripheral field limits
Procedure
Patient removes spectacles and occludes OS; have patient fixate your nose
Move target (wand) from behind patient (non-seeing to seeing) toward the horizontal limit of the field o Test slightly above and below the temporal midline
Have patient tell you when it comes into view
Do the same for the superior and inferior visual field o Test on both sides of the superior and inferior midline
Test nasal side o Test on either side of the nasal midline
Repeat for OS
Record limits (ALWAYS record from the patient’s perspective) o Normal
Advantages
Provides a means to quantify confrontation fields
Easier for patient to understand and/or respond
Disadvantages
Testing the limits of the VF produces variable sensitivity , therefore difficult to detect true visual field loss in the far peripheral field
Does not screen for extinction phenomenon
Interpupillary Distance o Distance between centers of the entrance pupils
Important for:
Alignment of optical instruments (avoids prismatic effects induced)
Spectacle design considerations o Optical centers match PD’s (if not, induces prism)
Documentation of craniofacial abnormalities
Measure monocular PD’s for high powered spectacle prescriptions, PALs o Procedure for binocular PD
Sit at eye level with patient ~40 cm away
Close your right eye and have patient look into your open left eye
Place zero at the temporal limbus of the right eye (DO NOT MOVE)
Note position that is aligned with the nasal limbus of the left eye: NEAR PD
Close left eye and have patient look into your open right eye
Note position that is aligned with the nasal limbus of the right eye:
DISTANCE PD
Record distance/near o Procedure for monocular PD
Place ruler on the patient’s bridge
Close your right eye and have patient look into your left eye
Align zero mark with the center of the pupil (CANNOT use pupil margin or limbus)
Note the mark centered on the bridge: OD MONOCULAR PD
Move ruler and place an easily recognized mark on the center of the bridge
(use this as the zero mark)
Open your right eye, close your left, and have patient look into your right eye
Note mark centered in the patient’s left pupil; subtract the ‘zero’ reading from the last reading: OS MONOCULAR PD o Use Prentice’s rule to calculate the induced prism from decentration
P= dF o Errors: unsteady positioning, error in parallax, patient’s with fixation disparities and doctor’s PD significantly wide (will overestimate)
Ocular Dominance o The preferential sighting of a target with one eye o In monovision CLs fitting, the dominant eye is generally fit with the distance o Useful when the subjective match in the clarity of the lines of letters cannot be achieved during binocular balance
Leave dominant with slightly clearer vision o Do not leave the VA of the dominant eye worse than the non-dominant eye o Place prism before the non-dominant eye o Procedure
Instruct patient to fully extend arms and create a triangle with both hands
Patient looks through aperture at the doctor’s right eye
Eye aligned with the doctor’s is the dominant eye
Record ocular dominance