Case 6 Phlyctenulosis - Pennsylvania Optometric Association
advertisement

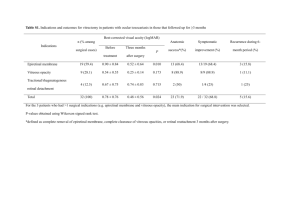
SPRING EDUCATIONAL SEMINAR – 2013 PENNSYLVANIA OPTOMETRIC ASSOCIATION CLINICAL CHALLENGES IN THE DIAGNOSIS AND MANAGEMENT OF OCULAR PATHOLOGY A PANEL DISCUSSI0N MODERATED BY BERNARD H. BLAUSTEIN, O.D., F.A.A.O. Case 1 Hyphema Description - An accumulation of blood in the anterior chamber - Usually results from a tear in the blood vessels at the root of the iris secondary to blunt trauma to the front of the eye (contracoup) but may occur secondary to neovascularization in the iris, intraocular surgery, or bleeding diathesis - The injury may tear the iris away from the ciliary body (iridodialysis) Workup - Rule out globe rupture - severe subconjunctival hemorrhage and edema along with restricted ocular motility. - Rule out orbital floor fracture - displaced globe, restriced elevated gaze, reduced sensation in the distribution of the infraorbital nerve, emphysema of the periorbital tissues, positive CT scan. - Quantify degree of hyphema (if greater than 50%, there is an increased risk of glaucoma and endothelial decompensation leading to blood staining of the corneal stroma). - Quantify flare and cells - Applanation tonometry QD until hyphema resolves - Dilate pupil and evaluate fundus if patient has not sustained a concussion (with concussion, you want to make sure there is no subsequent compression on CN III). - No gonioscopy or scleral depression so as not to disturb clot - Applanation tonometry - Rule out sickle cell disease if patient is black. (sickled cells may block TM causing IOP to rise; reduced perfusion to the optic nerve may occur at lower IOPs) - Attempt to prevent rebleed within 2-5 days post trauma so as to prevent increase in IOP and decompensation of endothelium. Management and Treatment - Attempt to encourage clotting for at least 3 days; then encourage reabsorption of the clot. - Hospitalize patient if he is too young to cooperate or if systemic medications will be administered. -2- Advise bed rest with head elevated 30 degrees (lowers venous pressure so as to reduce chance of rebleed, decreases IOP, facilitates settling of the blood). - Advise against bending or lifting of heavy weights. - Utilize Fox shield to prevent accidental jarring of eye. - Recommend acetaminophen for pain (aspirin may induce rebleed). - Utilize atropine 1% BID to immobilize pupil and to stabilize traumatic iritis; utililize Pred Forte to reduce the inflammation of traumatic iritis. - Consider aminocaproic acid (Amicar) systemically to preserve the clot. - Reduce IOP if above 30 mm Hg in a caucasian or if above 24 mm Hg if patient has sickle cell trait (slight elevations of IOP are beneficial as a tamponade and tend to encourage clotting) - Consider irrigation and aspiration if elevated IOP is nonresonsive, hyphema is greater than 50% and corneal staining is beginning to occur, and if hyphema has not begun to clear in 4 days. - Tonometry 30 days post hyphyma to determine if IOP is rising due to obstruction of the TM by degenerated RBCs (ghost cells); gonioscopy 30 days post hyphyma to check for angle recession; dilated fundus evaluation with scleral depression 30 days post hyphema to check for retinal holes thereafter; Case 2 Recurrent Corneal Erosion (RCE) Description - A recurrent erosion of the corneal epithelium due to some disturbance in the adhesion complex - Usually occurs when the patient awakens from sleep - Erosion has large, loose flap edges Etiology - Antecedent corneal injury from a sharp object which has injured the adhesion complex - Diabetes (weakens the adhesion complex) - Any corneal dystrophy that disrupts the adhesion complex, e.g., epithelial basement membrane dystrophy, Reis Bucklers corneal dystrophy, granular corneal Dystrophy, macular corneal dystrophy Epithelial Basement Membrane Dystrophy - The most common cause of RCE - An autosomal dominant dystrophy found most commonly found in females over age 30 - Consists of reduplicated and thickened basement membrane that has impaired fibrillar attachment to the underlying Bowman’s membrane - Appears clinically as fine epithelial lines which assume the shape of finger- prints or land formations on a map; may also manifest gray-white putty -like formations which represent cysts of fluid and cellular debris -3Treatment of RCE - Debride loose epithelium; apply antibiotic; apply cycloplegia; pressure patch for 24 hours. - Hypertonic saline drops QID and hypertonic ointment HS for 6-8 weeks - If RCEs continue, consider fitting patient with high-water contact lens. - If RCEs continue, consider stromal puncture or phototherapeutic keratotomy (PTK) to bind the basement basement membrane to the underlying Bowman’s layer. - The newest management approach is to have the patient utilize topical steroid, TID for three weeks along with 50 mg doxycycline, BID for 2-3 months. (doxcycline and steroid inhibit matrix metalloproteinase 9, an enzyme that degrades the adhesion complex) Case 3 Thygeson’s Superficial Punctate Keratopathy Description - A bilateral, but often asymmetric, coarse, punctate epitheliopathy usually occuring in females under age 40 - Patient presents with pain, photophobia, and lacrimation - Lesions appear as oval to circular coarse, gray, grainy, elevated dots and will stain with FL - There is little or no conjunctival or lid involvement, i.e. the eyes are minimally injected, and there are no follicles or papillae - The pathology runs a chronic course with exacerbations and remissions. When in remission the lesions are not elevated, do not stain, and induce no symptoms. Management and Treatment - Rule out EKC ( hyperemic conjunctiva, edematous lid, follicles, preauricular lymphadenopathy). - Rule out toxicicty, e.g. the patient admits to using eyedrops. - Treat with low-dose topical steroids, e.g., Alrex, Lotemax, FML - relief is dramatic often occurring in as little as one day. Case 4 Optic Neuropathy Masquerading as Glaucoma Anatomic Considerations – Optic Nerve - The optic nerve consists of axons from retinal ganglion cells, i.e. the nerve fiber layer (NFL). - Retinal NFL is divided into 3 bundles: papillomacular bundle, arcuate bundles, nasal radial bundle 1. Papillomacular bundle - Fibers run a straight course from the fovea to the temporal half of the optic disc and do not respect horizontal meridian. -4- Lesions produce temporal pallor, central or cecocentral scotomas, VA reduction, APD, color vision deficit, light sensitivity deficit - Glaucoma preferentially spares the papillomacular bundle until very late in the disease process. - Temporal pallor is not a normal manifestation of glaucoma. 2. Arcuate bundles - Fibers originate temporal to the macula, arch above and below the papillomacular bundle, and enter disc at the superior and inferior poles. - Fibers are segregated into upper and lower compartments and do not cross the horizontal raphe. - Glaucoma preferentially affects the arcuate bundles. - Lesions affecting arcuate fibers near the fovea, produce paracentral scotomas. - Lesions affecting arcuate fibers near the optic disc, produce partial arcuate scotomas which do not cross the nasal horizontal meridian. - Lesions affecting fibers remote from the disc, produce nasal steps. 3. Nasal radial fibers - Fibers originate nasal to the optic disc. - Fibers fan into the optic disc in a radial fashion. - Fibers do not segregate into upper and lower bundles and do cross the horizontal raphe. - Lesions produce wedge-shaped defects which do not respect the horizontal meridian and do not produce a step-like depression. Case 5 Phlyctenulosis Description - A pinkish-white nodule at the limbal conjunctiva; may not involve the cornea - Nodule is vascular but centered in an area of dilated blood vessels with a local leash of blood vessels running away from the lesion - Usually occurs in children or young adults Conjunctival phlyctenulosis - Mild symptoms of discomfort - After several days, lesion becomes necrotic and sloughs off leaving no scar Corneal phlyctenulosis - Lesion has a triangular shape and sits astride limbus - Significant symptoms of pain, photophobia, and lacrimation - Lesion may be stationary or may migrate onto cornea - If corneal migration occurs, neovascularization and scarring may occur. -5Etiology - Results from a Type 4 delayed hypersensitivity reaction to a systemic antigen - Etiology is usually staphylococcus; tuberculosis is the second most common etiology. - Other etiologies include intestinal parasites, chlamydia, HSV, or gonococcus. Differential diagnosis - Inflamed pingecula - Nodular episcleritis - Vernal limbal keratoconjunctivitis - HSV - Corneal neovascularization running into a stromal infiltrate - Ocular rosacea Treatment - If staphylococcal blepharitis is present – lid hygiene and antibiotic ointment along with topical steroids, e.g. FML, Lotemax - If rosacea is present – systemic tetracycline or erythromycin along with topical steroid - If TB, intestinal parasites, chlamydia, or gonococcus are present coordinate with PCP, and continue topical steroid Case 6 Central Serous Chorioretinopathy (CSR) Description - An exudative chorioretinoapthy characterized by a neurosensory retinal detachment - Appears as a thin, clear, blister-like lesion underneath the macula; the foveal reflex is lost; there are often sub-retinal precipitates. - There may be an associated retinal pigment epithelium detachment. - A positive scotoma, i.e. metamorphopsia and /or micropsia, is present. - An increase in hyperopia is present. - Most cases occur in men between ages 20-50; however, pregnanacy is a known risk in females. - CSR is associated with Type A personality features in individuals who have elevated stress and elevated stress hormones, i.e. corticosteroids and epinephrine. - Other etiologies include topical steroids, steroid inhalers, or systemic steroids. Pathophysiology - The inner choroidal vasculature undergoes vasoconstriction; some of the overlying RPE cells decompensate leading to a focal break between the RPE cells; a malfunction of the RPE pump mechanism occurs, and fluid accumulates in the space between the RPE and the sensory retina. -6- Fluid accumulating between Bruch’s membrane and the RPE results in an RPE detachment which has a yellow-orange appearance and is more solid-looking and thicker than the serous neurosensory detachment. Workup - History of steroid use?, Amsler grid, photo-stress recovery test - OCT – separation between RPE and sensory retina/separation between RPE and Bruch’s membrane - IV fluorescein angiography (IVFA); with CSR a small, diffuse hyperfluorescent spot appears in the choroidal phase and spreads out like an ink blot or spreads upward in a column resembling a smoke stack. The spot increases in intensity and size. With an RPE detachment, there is an early, even leakage with sharp borders. The leakage remains localized, increases in intensity, but does not increase in size. - Rule out other causes of exudative retinal detachment, e.g. choroidal melanoma, metastasis to the choroid, renal disease acute hypertension, choroidal hemangioma, chorio-retinal inflammations. Treatment of CSR - Discontinue all steroid medication - CSR usually resolves in 3-4 months; 90% of patients recover VA to 20/20; 30-40% have recurrences. - Micropulse laser photocoagulation of RPE leakage sites outside FAZ that have been identified via IVFA - Low fluence photodynamic therapy (PDT) Case 7 Macular Pseudo-hole Description - A sharply circumscribed, red, macular lesion within an area of epiretinal membrane traction; the epiretinal membrane pulls the inner portion of the fovea toward the center causing the foveal contour to steepen into a holelike configuration. - The outer nuclear layer and the photoreceptor layer are preserved; VA 20/4020/60 - Lamellar hole is a subcategory of pseudo-hole in which there is an irregular foveal contour, a break in the inner fovea, a split between the inner and outer retina, and intact foveal receptors Differential Diagnosis - Cystoid macular edema – often follows cataract surgery - Full thickness macular hole -7Pathophysiology of Macular Epiretinal Memebrane - Develops at the vitreoretinal interface; consists of proliferating glial cells that have gained access to the retinal surface through breaks in the ILM (ILM) - Breaks in the ILM may be created secondary to PVD, retinal detachment surgery, retinal trauma, retinal vascular disease, or chronic uveitis. - Macular epiretinal membranes are divided into cellophane maculopathy and macular pucker. Cellophane Maculoathy - A thin transparent membrane of fibroglial cells which applies tangential traction to the retina; retinal surface is irregular with fine striae and tortuosity of small blood vessels - Patient may be asymptomatic or may present with mild VA deficit and mild metamorphopsia - Best detected with red-free light Macular Pucker - Caused by increased thickening and contraction of the epiretinal membrane - Severe retinal wrinkling and distortion of the blood vessels are manifest. - White striae may obscure the underlying blood vessels. - Vision deficit and metamorphopsia are more severe. - A macular pseudo-hole may form within the epiretinal membrane. Treatment of Epiretinal Membrane - Vitrectomy and membrane peel Macular Hole - Develops as a result of progressive vitreoretinal traction at the fovea - Progresses through four stages Stage 1a is an impending hole that appears as a yellow foveolar spot with a loss of foveal depression. Stage 1b results from centrifugal displacement of the foveola; characterized by a yellow ring around the fovea and mild VA deficit and mild metamorphopsia Stage 2 is an early, small full-thickness hole that appears as an oval or crescent and has loss of photoreceptors and markedly reduced VA Stage 3 is a larger full-thickness hole about the size of 1/3 of a disc diameter; has a small cuff of subretinal fluid; the posterior cortical vitreous remains attached. Stage 4 is a larger full-thickness hole with a complete PVD; the hole is surrounded by a larger cuff of subretinal fluid; often has tiny yellow flecks at bottom of the hole -8Diagnosis of a Full Thickness Macular Hole - Watske-Allen test – a narrow slit beam is projected vertically and horizontally over the center of the hole. Patients with a true hole will note that the slit beam is broken; patients with a pseudo-hole will note that the slit is thin but not broken. - OCT reveals anvil-shaped edges and complete loss of photoreceptors and the outer nuclear layer Treatment of Macular Hole - If the VA is less than 20/60 and the duration has been less than one year, vitrectomy and removal of ILM followed by injection of gas into the vitreal cavity; patient must maintain a face-down position for one to two weeks to allow the gas bubble to tamponade the hole; success occurs in 80% of patients. Case 8 Talc Retinopathy Description - Intraretinal, yellow, refractile particles in patients found in patients who repeatedly inject drugs intended for oral use (Ritalin, Methadone) intravenously - The oral drugs contain inert fillers such as talc (hydrous magnesium silicate). - The number of talc particles in the retinal vessels is dependent upon the duration of drug abuse and the number of IV injections. Pathophysiology - Oral drugs with talc fillers are injected IV. - Talc passes through the right auricle and right ventricle and enters the lung. - Some of the talc particles are bigger than the pulmonary capillaries and become entrapped. - Granulomas develop causing further occlusion of larger arteries; diminished lung capacity and reduced pulmonary function result. - Pulmonary hypertension results causing enlargement of the right ventricle (cor pulmonale); chest pain, syncope, and sudden death may result. - As pulmonary hypertension increases, collateral blood vessels develop in the lung. - The collaterals are large enough to allow the talc particles to gain access to the systemic circulation as blood passes through the left auricle and left ventricle. - The talc embolizes to the eye, skin, liver, kidney, and bone marrow. - The talc can be scattered throughout the fundus but concentrates in the small arterioles, precapillaries, and capillaries in the macular area. (There is a denser capillary net and greater blood flow in that area.) - Capillary occlusion may result in venous engorgement, blot hemorrhages, cotton wool spots, and peripheral neovascularization. -9Differential Diagnosis - Cholesterol deposits (Hollenhorst plaques ) - Tamoxifen - Canthaxanthine (oral tanning agent) - Calcific drusen Drusen - RPE phagocytizes the tips of the outer segments of the rods and cones. - The engulfed particles are degraded and recycled or are voided into the choriocapillaris. - With increasing age, Bruch’s membrane thickens and prevents the deposition of the breakdown products into the choriocapillaris; the particles become stored in Bruch’s membrane as drusen. Isolated Discrete Drusen - Small, isolated, discrete, yellowish bodies with little evidence of RPE atrophy; VA relatively good Confluent Soft Drusen - Indicate significant thickening of Bruch’s membrane and RPE atrophy - Have the highest risk of developing into advanced AMD Hard Calcific Drusen - Occur in long standing, indolent AMD; VA usually good Workup of Talc Retinopathy - Fluorescein angiography if neovscularization is suspect - Lung x-ray and lung function tests Case 9 Meibomian Gland Dysfunction/Dry Eye Description - Dry eye is a disorder of the tear film that results from decreased tear production, excessive evaporation, or an abnormality in the mucin or lipid components. - The most common cause of dry eye is meibomian gland dysfunction, a condition which causes evaporative dry eye Signs and Symptoms of Dry Eye - Conjunctival hyperemia, fast BUT, decreased tear meniscus, viscous tears, debris-laden tears, SPK on inferior 1/3 of cornea, rose bengal or lissamine green stain of cornea and intrapalpebral conjunctiva, filaments - Patients indicate that the eyes feel sandy, itchy, gritty, or burning, and report intermittent blurred vision, FB sensation, and photophobia. - Symptoms increase as the day wears on. - Symptoms often do not correlate with signs. -10Anatomic and Physiologic Correlates - Tears are composed of three intertwined layers: oil from the, meibomian glands, aqueous from the lacrimal glands, and mucous from the conjunctival goblet cells. - Tears dilute noxious stimuli and flush away inflammatory cells, debris and components of corneal metabolism. - Tears supply oxygen, vitamin A, epidermal growth factors, transforming growth factors, and antimicrobial proteins (lysozyme, lactoferrin, beta lysin). - Tears provide a smooth refracting surface to the cornea by filling in surface defects. - A neural functional reflex loop governs tear secretion: continuous ocular surface challenge induces sensory afferents to fire; secretory efferents stimulate secretion of aqueous, mucous, and lipids. - Dysfunction of the reflex loop alters the quantity and quality of the tear film. Pathophysiology of Inflammatory Dry Eye (Keratoconjunctivitis Sicca) - KCS is a chronic, immune-based, cytokine receptor inflammation characterized by the infiltration and disruption of lacrimal gland tissue by CD4 T lymphocytes - The lymphocytes secrete proinflammatory cytokines that promote apoptosis of lacrimal gland tissue and inhibit the neural reflex loop. - Reduced androgens in perimenopausal and postmenopausal women also induce lacrimal cell apoptosis and the accumulation of proinflammatory cytokines. Meibomian Gland Dysfunction (MGD) Non-obstructive MGD - Occurs in association with hypersecretion of the meibomian glands of the skin (seborrheic dermatitis) and dandruff - The meibomian gland ducts and orifices are dilated, and the meibum can be easily expressed. - The meibum is of normal consistency, but the amount is excessive. - Frothy-appearing tears collect along the lid margin. - Excessive oils adulterate the tear film causing dry spots on the cornea and discomfort. - Endogenous lid bacteria convert the meibum to fatty acids whose low pH causes discomfort. Obstructive MGD - The gland ducts and orifices are clogged, and meibum cannot be easily expressed. - Aqueous portion of the tears evaporate rapidly - Often occurs in middle-aged patients who manifest rosacea - Lid margins are often thickened, notched, and telangiectatic. -11Treatment of Meibomian Gland Dysfunction/Dry Eye - Non-obstructive MGD: warm-to-hot compresses, lid scrubs, anti-dandruff shampoos, non-preserved artificial tears to reconstitute the tear film, topical 1% azithromycin (Azasite) to reduce inflammation, referral to a dermatologist for the seborrheic dermatitis - Obstructive MGD: in-office lid gland expression, at-home warm-to-hot compresses followed by lid gland expression, topical 1% Azasite, consider a short course of systemic tetracyclines, non-preserved artificial tears, consider omega-3 fatty acid supplementation, consider cyclosporine A (Restasis) Case 10 Optociliary Shunt Vessels Description - Optociliary shunt vessels consist of enlarged pre-existing capillaries on the optic nerve head that shunt blood from the central venous circulation to the peripapillary choroidal circulation. - Occurs when there is when there is an obstruction of the normal venous drainage behind the lamina - The shunted blood bypasses the retinal venous circulation and passes into the choroidal venous system; subsequently, the blood passes through the vortex veins and into the superior and inferior ophthalmic veins. Etiology Obstruction of the Central Retinal Vein - Usually occurs as a result of compression of the central retinal vein (CRV) - Most commonly, the compression results from an arteriosclerotic central retinal artery compressing the CRV in the common adventitial sheath. - Compression may also occur from papilledema, an ONH tumor, or laminar compression from elevated IOP. Central Retinal Vein Thrombus - May occur from autoimmune disease, excessive coagulation of the blood, hyperviscosity, or IOP-induced laminar compression causing turbulence of the blood and subsequent thrombus Optic Nerve Sheath Meningioma - Neoplasm arises from arachnoid and affects women over 40 - Involves optic nerve within the orbit causing compression and occlusion of the veins of the optic nerve - Causes slow, progressive vision loss