Blood Administration and Transfusion Reactions –Exam
advertisement

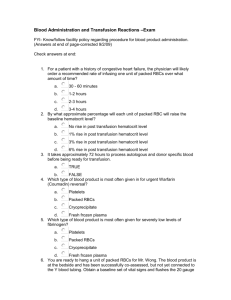
Blood Administration and Transfusion Reactions –Exam FYI- know and follow facility policy regarding procedure for blood product administration. Check answers at end: 1. For a patient with a history of congestive heart failure, the physician will likely order a recommended rate of infusing one unit of packed RBCs over what amount of time? a. 30 - 60 minutes b. 1-2 hours c. 2-3 hours d. 3-4 hours 2. By what approximate percentage will each unit of packed RBC will raise the baseline hematocrit level? a. No rise in post transfusion hematocrit level b. 1% rise in post transfusion hematocrit level c. 3% rise in post transfusion hematocrit level d. 6% rise in post transfusion hematocrit level 3. It takes approximately 72 hours to process autologous and donor specific blood before being ready for transfusion. a. TRUE b. FALSE 4. Which type of blood product is most often given for urgent Warfarin (Coumadin) reversal? a. Platelets b. Packed RBCs c. Cryoprecipitate d. Fresh frozen plasma 5. Which type of blood product is most often given for severely low levels of fibrinogen? a. Platelets b. Packed RBCs c. Cryoprecipitate d. Fresh frozen plasma 6. You are ready to hang a unit of packed RBCs for Mr. Wong. The blood product is at the bedside and has been successfully co-assessed, but not yet connected to the Y blood tubing. You obtain a baseline set of vital signs and flush the 20 gauge saline lock to assure patency. The saline lock is clearly infiltrated and will need to be restarted. You are familiar with this patient and estimate 20-30 minutes of time to successfully start the new peripheral IV. What should you do with the PRBC blood product while starting the new IV line? a. Temporarily store the unit of PRBCs in the medication refrigerator b. Leave the unit of PRBCs at the bedside and hope for quick IV start c. Return the unit of PRBCs back to the designated blood bank designated refrigerator d. To avoid delay, piggy back the blood tubing into the continuous heparin drip IV line and administer the unit of PRBCs through this shared line 7. The standard IV blood administration tubing can be safely used to administer up to 3 units of packed RBCs? a. True b. FALSE 8. The only approved IV solution to be used to prime blood tubing is: a. 0.45 % Normal Saline b. D5 ½ Normal Saline c. 0.9% Normal Saline d. Lactated Ringers 9. Which blood type is considered to be the Universal Donor? a. Type O + b. Type O - c. Type AB + d. Type AB 10. Which blood type is considered to be the Universal Recipient? a. Type O + b. Type O - c. Type AB + d. Type AB 11. Which of the following is NOT an essential component of the safe co-assessment between the wrist-band and blood bag label prior to blood product administration: a. Last blood glucose level b. ABO/RH type compatibility c. Blood bank armband number d. Medical record number or other designated number 12. Which of the following is a potential acute transfusion reaction? a. HIV infection b. CMV infection c. Hepatitis infection d. Hemolytic reaction 13. The most common medications prescribed to treat an allergic transfusion reaction include: a. Diuretics. b. Beta blockers. c. Vasopressor therapy. d. Antipyretic and antihistamines. 14. Your patient shows signs of an allergic reaction to a blood transfusion by exhibiting a temperature of 100.9F. You administer Tylenol 650mg PO. It is now safe to resume the blood product transfusion since your patient has been treated and is now asymptomatic from their allergic (type) of blood transfusion reaction. a. TRUE b. FALSE 15. A hemolytic blood transfusion reaction is highly dangerous and is the result of: a. Decreased RBC production. b. Contamination of the blood product. c. Incompatible ABO or Rh blood type. d. Antibodies react against donor white blood cells or platelets. 16. If a hemolytic blood transfusion is suspected, the blood bank will ask the RN to send: a. Nasal swab culture. b. Medication and allergy list. c. The original MD order for the blood product. d. A new blood specimen & first voided urine specimen. 17. To prevent bacterial contamination of the blood product and possible sepsis, you will: a. Run the blood product through an infusion pump. b. Assure the peripheral IV catheter is an 22 gauge or larger. c. d. Co-assess the key elements with another licensed colleague prior to hanging the product. Change blood administration set and filter every 4 hours or after every 2 units of PRBCs. 18. Ten minutes after starting a new infusion of PRBCs, you suspect an acute hemolytic transfusion reaction. You stop the blood infusion, and keep the vein open with NS and new IV tubing. You also obtain vital signs, notify the MD and the blood bank. In addition to the above, what else is important for you to followup on? a. Ask the MD for an order to administer an anticoagulant b. Call the family and ask if they want to alter the advance directive c. Send the blood bag and IV tubing back to the blood bank for testing d. Assess for new signs and symptoms of deep vein thrombosis (DVT) 19. The most common type of post-transfusion (late) infection is: a. HIV. b. CMV. c. Syphilis. d. Hepatitis. 20. Despite advances in blood bank testing and infection-control guidelines, it remains possible for a person receiving a blood transfusion to become infected with hepatitis or HIV because: a. Answers1. d 2. c 3. a 4. d 5. c 6. c 7. b 8. c 9. b Medications such as Epogen or Procrit can cure hepatitis and HIV. b. Specific donor screening questions are not being asked of high-risk blood donors. c. Donors with O+ blood type cannot be successfully screened for hepatitis and HIV. d. Specific antibodies for hepatitis and HIV are not detectable for several weeks after exposure. 10. c 11. a 12. d 13. d 14. b 15. c 16. d 17. d 18. c 19. d 20. d