DOWNLOAD and VIEW the full-length interview with Dr

“The World’s Smallest Heart Pump”
Vivian Dimas, MD
Dr. Vivian Dimas, MD, Assistant Professor of Pediatrics at University of Texas Southwestern,
Interventional Cardiologist at Children’s Medical Center at Dallas, talks about the world’s smallest heart pump.
How many heart surgeries do you do on kids a day?
Dr. Dimas: We actually don’t do heart surgery. We do catheterizations. We do typically two to four catheterizations per day five days a week for children.
What does that usually involve?
Dr. Dimas: It can involve anything from what we call a diagnostic procedure, where we put the catheters in that look like long tubes or straws, to just defining the anatomy; taking pictures, measuring pressures, getting ready for an open heart surgery, all the way to closing holes and sometimes making holes. So, we do a little bit of everything.
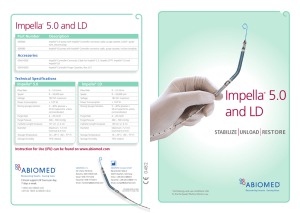
Tell me what is the Impella?
Dr. Dimas: The Impella is actually the smallest heart assist device that’s on the market. It’s a device that helps failing hearts, but the difference between it and what we currently have available is that it’s able to be put in through an artery in the leg as opposed to having to have open heart surgery.
So, before you had to use the Berlin heart?
Dr. Dimas: Yes. So, the Berlin heart is actually a different type of assist device. It’s a more permanent type of assist device, meaning that child has failed conventional therapy whether that is medicines alone or what we used to use to support children who needed short-term support called ECMO, which is extra corporeal oxygen membrane oxygenation (a fancy word for a heart/lung bypass machine). The ECMO circuit is very invasive and it requires surgery where they put the tubes into the arteries and veins through the neck and into the legs and sometimes through an open chest. They actually take the blood out of the heart and oxygenate and pump it back in because the heart cannot do that work itself.
How is the Impella different from the ECMO?
Dr. Dimas: The Impella differs because it can be put in from the leg either straight in like a catheter or with just a little surgical cut. You can actually support the heart without having to place someone on the heart/lung bypass machine, which is very invasive and also has a lot of complications associated with it. It provides very short-term assistance for children who we expect might recover.
How long can it be used for?
Dr. Dimas: It can be used for a fe w days. It’s approved was for short-term use in the United
States, but it has experience being used for up to five to seven days. It’s being used for longer, but I think routinely people use it up to about five days.
What did this Impella do for Emily?
Dr. Dimas: Emily has had a heart transplant for restrictive cardiomyopathy. She came in with an acute rejection episode, which was actually the first episode of rejection that she’s had and her heart was failing. She was actually deteriorating fairly quickly after her admission, which is pretty typical for patients who are in rejection. We had to determine a way to support Emily as quickly as possible or we were worried that we were going to lose her. We decided that we would place her on the Impella to support her left heart so that we could complete the catheterization, where we get a piece of tissue from the heart, so that we could determine how severe and which type of rejection she had to guide our therapy.
So why not do the ECMO or the Berlin?
Dr. Dimas: ECMO is a very invasive procedure that requires multiple surgical cut downs. The other issue with that is that ECMO usually requires blood product administration. Every time you give children blood products, particularly patients who’ve had a heart transplant, you sensitize them. Meaning that they develop antibodies to other blood types, which then makes episodes of rejection more likely should she recover from that episode. It also complicates future transplants because they are more sensitized to other donors and it limits the donor pool for them. So blood products are a very big issue in our population.
This gave her the days that she needed to get a heart?
Dr. Dimas: Yes. This bought her the days so that we could treat her rejection episode. So, as she continued to deteriorate we decided to put this in a cath lab that day. We were able to successfully support her. We got through the catheterization procedure, but then she actually continued to get worse to the point that her left heart was essentially not functional. It was pumping very little if any blood and she was being supported entirely by the Impella. We kept her on it for about four and a half days, long enough for us to give her very aggressive antirejection therapy. As she responded to the medicines for rejection she slowly recovered her heart function and was able to be weaned from the Impella and we were actually able to take the Impella out and she recovered and was able to go home from the hospital following that initial episode. The issue with Emily is that the heart never really fully recovered. She had a type of rejection that also affected the arteries. So the heart never actually recovered.
For Emily, this allowed her heart to rest to prevent rejection?
Dr. Dimas : Yes, to allow us to treat it.
Did she start rejection because of any infection?
Dr. Dimas: It’s hard to know because sometimes infections can affect the body so that you aren’t absorbing your medicines as well as you should be and so your levels of the anti-rejection medicines can get a little bit low. So, anytime someone has an infection it can actually alter their ability to fight infections just because they’re on those medicines and it can affect the absorption.
It then could lead to having what we would call inadequate or sub-therapeutic drug levels and that can precipitate an episode of rejection. I t’s hard to know how she got there, but she was
presented she was in Grade Three R rejection, which is our most severe type of rejection that we’ve been able to survive people through. So, once we put her on the Impella, we were able to back off on the very aggressive medicines we gave her to treat the rejection and her heart began to recover and we were able to resume the workload by weaning the Impella and she tolerated that very well and then we discontinued the device. We were actually able to send her home but the heart never fully recovered and we ultimately relisted her for heart transplant, which she successfully underwent the day after Christmas.
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Children’s Medical Center
(214) 456-7000
Sign up for a free weekly e-mail on Medical Breakthroughs called
First to Know by clicking here
.