Advice leaflet for chronic cough
advertisement

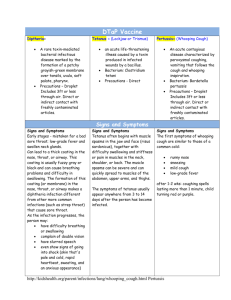
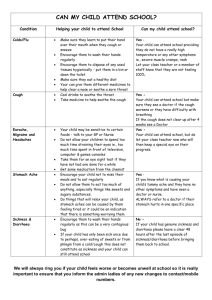
ADVICE FOR THOSE WITH CHRONIC DRY COUGH ‘Chronic dry cough’ is a cough that has persisted for over 6 weeks If a cough lasts over 3 weeks, patients should see their GP for review Depending on other symptoms, the GP may arrange a chest X-ray, sputum sample, breathing tests, tests of heart and/or lung function and possibly referral on to a specialist Chronic cough can be due to one or more causes, including: 1. Chronic lung conditions: asthma, COPD, bronchiectasis and others 2. Heart disease: heart failure 3. Nasal disease: rhinitis/sinusitis 4. Laryngopharyngeal reflux: escape of stomach acid and proteins into the throat (known as ‘silent reflux’ because many patients with throat symptoms do not experience heartburn/indigestion) 5. Medications: ‘ACE inhibitors’, used for hypertension and heart disease 6. Rarely, lung cancer If at any point you experience coughing up blood, unexplained weight loss, increasing shortness of breath, chest pain, worsening cough, a lump or swelling in the neck or difficulty swallowing food it is important that you see your GP in case further investigation is required. A clear cause, such as those above, should be ruled out, but for many patients with chronic cough a cause remains elusive. How the cough reflex works The cough reflex protects the lungs by removing or stopping irritants getting to the lungs. Irritants stimulate cough receptors in the throat, windpipe and lungs which send nerve impulses to the spine and brain. They respond by sending nerve impulses back to the body muscles that produce a cough. Throat irritants increase the number of cough receptors making the cough reflex more sensitive. A person with a more sensitive cough reflex will cough when exposed to normal everyday things more so than another individual with a less sensitive cough reflex. It is likely that by allowing time to pass, looking after the respiratory tract (nose, throat, windpipe and lungs), and by applying “mind over matter” the cough reflex sensitive can be reduced to a more acceptable level. However, it is likely that with the next significant stimulation, such as a bad cough/cold infection, the cough may be troublesome again and the same measures will need to be adopted to allow it to settle. In this sense, for many patients, a chronic cough is indeed a chronic symptom they have to learn to manage. An irritated respiratory tract may be caused by many factors, including: Poor diet or poor vocal hygiene (see below) Allergies such as asthma and allergic rhinitis Reflux of acid and enzymes from the stomach (usually ‘silent’ reflux) Environmental irritants – dust, cleaning fluid fumes, paint aerosols etc Infection: Following an infection, irritation can persist even after the infection has cleared Treatment is to minimise as many irritant factors as possible and always includes improving vocal hygiene. Treatment of laryngopharyngeal reflux is often important also (even if you are not aware this is occurring – ‘silent reflux’). It may take up to 2 months for the symptoms of an irritated airway to settle with these measures. 1 Vocal Hygiene Advice Many airway and throat symptoms can be improved with vocal hygiene measures which reduce the “irritating” effects on the throat of caffeinated drinks, dehydration, smoke and stomach acid It may take 2 months for symptoms due to throat irritation to improve with vocal hygiene measures In short, it is important to: Drink plenty of water. Aim for 8 to 10 glasses per day (¾ to 1 litre) Use Steam inhalations twice daily or more often to soothe, cleanse and lubricate the throat. (Boil a kettle of water and fill a bowl. Allow water to cool a little so you do not burn yourself. Lean over bowl and place towel over head and bowl. Inhale steam. Do not add any oils/vapours to the water.) Avoid medicated throat lozenges as these dehydrate and irritate the throat when used often. Instead use steam inhalations and try chewing gum (as below) Avoid caffeinated drinks, e.g. Coffee, Tea & Cola. These are dehydrating and irritate the throat. If you must have a coffee or tea, make sure you have a glass of water at the same time Avoid fizzy/carbonated drinks as they are acidic Avoid acidic foods Avoid irritants such as smoking, alcohol, spicy food and smoky, dusty or dry atmospheres Chewing gum containing bicarbonate of soda (sold as tooth whitening gum) may help Take action to minimise stomach acid production, which can affect the throat. For example: o Avoid fatty foods, e.g. pastries, fast foods. o Eat small regular meals. o Do not eat late at night, try to eat 2 to 4 hours before going to bed. Avoid excessive coughing and ‘throat clearing’. The irritation in your airway feels like mucus and coughing/throat clearing may give you temporary relief but it will make your symptoms worse by causing more irritation. Often you can avoid the need to cough by having a sip of water instead or by doing a ‘dry swallow’. You should try this every time you feel the need to cough/throat clear. (This advice is for those with a chronic dry cough only – if you are not sure ask your doctor.) STOP COUGHING/THROAT CLEARING DRINK WATER INSTEAD CATARRH AND THROAT IRRITATION 2 COUGHING AND THROAT CLEARING Specific Treatments Nasal symptoms Patients whose cough is due to nasal disease will have other symptoms like a runny nose, dripping of secretions at the back of the nose (postnasal drip), blocked/congested nose and reduced sense of smell In these situations, treatment of the nose with nasal sprays +/- antibiotics, antihistamines and sometimes surgery may help Post Nasal Drip Many patients who have a feeling of post nasal drip without any other nasal symptoms or throat symptoms will have a normal examination and no clear cause will be found. In this situation, vocal hygiene measures as above should be taken in addition to the use of nasal douche on a regular basis. This may not provide a long term cure but will help manage the symptoms on a daily basis. Nasal douching can be carried out using proprietary preparations such as NeilMed Sinus Rinse available from chemists or by mixing you own salt solution (1 pint of boiled then cooled water with half teaspoon of salt and half teaspoon of sodium bicarbonate, as used for cooking) then sniffing the solution up each nostril from the cupped palm of your hand. Douching can be carried out as many times per day as you wish; two or three times per day is recommended. “Frog in the throat” or feeling of mucus/catarrh in the throat As for post nasal drip, many patients with this symptom and no other symptoms will have a normal examination with no clear cause found. Vocal hygiene measures remain the mainstay of management, often supplemented by anti reflux treatment such as regular Gaviscon Advance Medicines which reduce acid reflux o o Available ‘over the counter’ at your chemists: Gaviscon advance (licensed for the treatment of laryngopharyngeal reflux) Zantac/Ranitidine There are many other medicines available and the Pharmacist will be able to advise you. Other medicines available on prescription from your Doctor. Proton Pump Inhibitors (PPIs) e.g. Lansoprazole/Zoton; Omeprazole/Losec; Rabeprazole/ParietProkinetics Prokinetics e.g. Metoclopramide, domperidone. Studies have shown that for patients with throat symptoms (rather than just heartburn), medicines work best when taken regularly. They also take 2 months to relieve throat symptoms. Behavioural modification Relaxation techniques and cognitive behavioural techniques will help to suppress the sensation to cough These treatments are not currently available through local NHS services. It is likely that many other alternative medical treatments may help also Cough suppressants Morphine-related drugs suppress the cough reflex: They usually contain pholcodeine or codeine and are available in liquid form Some antihistamines are also cough suppressants. Cough suppressants should not be used for prolonged periods without medical supervision Treatments for lung and heart conditions causing cough are not covered here. 3