Pulmonary Function Test (PFT) Tutorial
advertisement

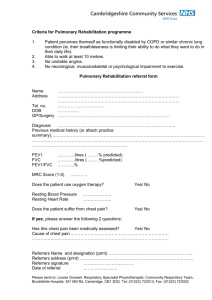
Case 1 A 65 year-old man undergoes pulmonary function testing as part of a routine healthscreening test. He has no pulmonary complaints. He has never been a s smoker but has a history of asbestos exposure while serving in the Navy. His pulmonary function test results are as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) FRC (L) ERV (L) RV (L) TLC (L) Actual 4.39 3.20 73 3.17 0.63 2.54 6.86 Predicted 4.32 3.37 78 3.25 0.93 2.32 6.09 % Predicted 102 95 98 68 109 113 Question 1.1 How would you classify the pattern of test results for this patient? A. Normal spirometry and lung volumes correct & explanation B. Obstructive pattern incorrect, try again C. Restrictive pattern incorrect, try again D. Mixed obstructive and restrictive patterns incorrect, try again Explanation for Question 1 Pulmonary function tests can be used to characterize a patient’s respiratory function abnormalities and this information, can be used, in turn, to guide further diagnostic workup and management for the patient. Each parameter that is measured can be expressed as an absolute value as well as relative to the predicted value of that parameter for that particular patient. This is often referred to as “percent of predicted” with the predicted value being a function of the patient’s age, gender, height, weight and race. The different parameters listed in the table above and their normal ranges are listed below: • The forced expiratory volume in one second (FEV1) is the volume of gas exhaled in the first second of a forced exhalation maneuver. The FEVl is deemed to be normal if it is greater than 80% of the predicted value. • The forced vital capacity (FVC) is the entire volume of gas exhaled during a forced exhalation maneuver. The FVC is deemed to be normal if it is greater than 80% of the predicted value. This maneuver can sometimes be performed with a slow exhalation in which case it is referred to as a Slow Vital Capacity (SVC). • The FEV1/FVC is the absolute value of the FEV1 divided by the absolute value of the FVC. Note that the units for these two parameters cancel and the ratio has no units. It is typically expressed as a decimal (e.g., 0.7). The lower limit of normal for this parameter varies based on which authority you consult. The Global Initiative for Obstructive Lung Disease (GOLD) and the American Thoracic Society and European Respiratory Society (ATS/ERS) guidelines set the lower limit of normal as 0.7. At the University of Washington, the lower limit of normal is determined by taking the predicted ratio for that patient and subtracting 0.08 if the patient is a man and 0.09 if the patient is a woman. For example, if you had a male patient and the predicted ratio was 0.76, the lower limit of normal for this patient’s FEV1/FVC ratio would be 0.68. Values below that would be considered abnormal. • The total lung capacity (TLC) is the maximal volume of the lungs. It is considered to be normal if it falls between 80% and 120% of the predicted value. • The residual volume (RV) is the volume of air left in the lungs at the end of a forced expiration. The normal range for this parameter is between 80% and 120% of the predicted value. Based on the observed values for the parameters described above, we can describe several basic patterns of abnormalities on pulmonary function tests including: • Normal: The FEV1/FVC ratio is above the lower limit of normal and the TLC resides between 80 and 120% predicted. • Obstructive pattern: is marked by reductions in the FEV1 and FVC and the FEV1/FVC ratio. The reduced FEV1/FVC ratio is considered the sine qua non of the obstructive pattern and a patient cannot be deemed to have this pattern unless this abnormality is present. In some cases, the SVC can be substituted for the FVC in order to calculate this ratio. • Restrictive pattern: is marked by reductions in the FEV1 and FVC but a preserved (i.e., normal FEV1/FVC ratio) and a reduced TLC. The reduction in FEV1 and FVC with a preserved ratio is only suggestive of the diagnosis of restriction, however, and the TLC must be reduced in order to label a patient as having a restrictive defect. • Mixed obstructive and restrictive pattern: is present when the patient has both a reduced FEV1/FVC ratio and the TLC is less than 80% of the predicted value. In this case, the FEV1, FVC, FEV1/FVC are normal, indicating there is no evidence of an obstructive defect. Because the TLC is 113% of predicted, the patient does not have a restrictive defect either. As a result, this patient has normal spirometry and lung volumes. Case 2 A 54 year-old man presents to his primary care provider with dyspnea, cough and intermittent chest tightness. His cough is worse at night, in the early morning and with exercise. He is a non-smoker with no relevant occupational exposures. Test FVC (L) FEV1 (L) FEV1/FVC (%) Pre-Bronchodilator (BD) Actual Predicted % Predicted 3.19 4.22 76 2.18 3.39 64 68 80 Post- BD Actual % Change 4.00 25 2.83 30 71 4 Question 2.1 How would you classify the pattern of test results for this patient? A. Normal spirometry incorrect, please try again B. Obstructive pattern correct & explanation C. Restrictive pattern incorrect, please try again D. Mixed obstructive and restrictive pattern incorrect, please try again Question 2.1 Explanation: If you use the criteria set forth by GOLD and the ATS/ERS, the actual ratio of 0.68 is below the 0.7 cutoff and the patient has an obstructive defect. If you use the criteria used at the University of Washington, the patient’s predicted ratio is 0.80. Given that this is a male patient, the lower limit of normal is determined by subtracting 0.08 from that value (0.72). His actual ratio of 0.68 falls below that cut-off as well so he would also be deemed to have airflow obstruction by this criterion. Question 2.2 How would you rate the severity of the observed abnormality? A. Mild defect incorrect, please try again B. Moderate defect correct & explanation C. Severe defect incorrect, please try again D. Very severe defect incorrect, please try again Question 2.2 Explanation For obstructive patterns, the severity is graded based on the decrement in the FEV1. • • • • > 80% predicted: mild obstruction > 50% and < 80% predicted: moderate obstruction > 30% and < 50% predicted: severe obstruction < 30% predicted: very severe obstruction Restrictive defects are graded based on the decrement in the TLC. • • • > 65% and < 80% predicted: mild restriction > 50% and < 65% predicted: moderate restriction < 50% predicted: severe restriction In this case, the FEV1 is reduced to 64% of predicted, indicating that the patient has moderate obstruction Question 2.3 Does the patient have a bronchodilator response? A. Yes correct B. No incorrect (Brian Valentine: Either answer should forward them to the explanation since it’s basically a 50/50 shot and sending them to guess again has no learning value.) Question 2.3 Explanation A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration In this case, there was an improvement of 25% (and 810 mL) in the FVC and 30% (and 650 mL) in the FEV1 so the patient would be classified as having a bronchodilator response. The presence of a bronchodilator response can be used to make a diagnosis of asthma, since the hallmark of that disorder is reversible airflow obstruction and the presence of a bronchodilator response demonstrates some evidence of reversibility. Keep in mind that although some patients with COPD may not demonstrate a bronchodilator response on pulmonary function testing, bronchodilators are still the mainstay of therapy in this patient population, as they still derive symptomatic benefit from their administration. Case 3 A 60 year-old man presents to his primary care provider with complaints of increasing dyspnea on exertion. He has a 40 pack-year history of smoking and is retired following a career as a building contractor. His pulmonary function testing is as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 1.89 4.58 41 0.89 3.60 25 47 79 5.72 2.31 248 7.51 6.41 117 76 37 15.73 33.43 47 Post- BD Actual % Change 3.69 96 1.89 112 Question 3.1 How would you classify the pattern of test results for this patient? A. Normal spirometry incorrect, please try again B. Moderate obstructive defect incorrect, please try again C. Very severe obstructive defect correct and explanation D. Restrictive pattern incorrect, please try again Question 3.1 Explanation The patient has a low FEV1 and low FVC and the ratio is reduced. This pattern is consistent with an obstructive pattern. The TLC is normal, as it falls between 80 and 120% of predicted and, therefore, there is no evidence of restriction. Because the FEV1 is < 30% of predicted, this would be classified as a very severe obstructive process. Question 3.2 Based on the information provided, how else can you characterize this patient’s pulmonary function? A. Air-trapping correct, explanation B. Hyperinflation incorrect, please try again C. Air-trapping and hyperinflation incorrect, please try again D. No bronchodilator response incorrect, please try again Question 3.2 Explanation When the residual volume (RV) (the volume of gas remaining in the lungs at the end of a forced expiration) is greater than 120% of predicted, the patient is deemed to have evidence of air-trapping. If the total lung capacity (TLC) is greater than 120% of predicted, the patient is deemed to have hyperinflation. Air-trapping and hyperinflation are findings that help characterize the patients physiologic abnormalities better but are not necessary to confirm the diagnosis of air-flow obstruction. Many patients with airflow obstruction based on the low FEV1/FVC ratio will have a normal RV and/or TLC. This patient’s RV is 248% of predicted while the TLC is only 117% predicted, indicating that he has air-trapping but not hyperinflation. Question 3.3 What conclusions can you draw from the patient’s DLCO? A. Normal DLCO incorrect, please try again B. Reduced DLCO indicating a loss of surface area for gas exchange correct & explanation C. Reduced DLCO indicating that he likely has polycythemia incorrect, please try again D. Reduced DLCO indicating high levels of carboxyhemoglobin in his blood from smoking incorrect, please try again Question 3.3 Explanation The DLCO is the diffusing capacity of the lung for carbon monoxide. This parameter gives us information about the adequacy of the surface area for gas exchange and can be used along with spirometry and lung volumes to understand the patient’s underlying physiology and generate a differential diagnosis. • In patients with obstructive defects on spirometry, a reduced DLCO suggests they have underlying emphysematous changes as the source of the reduced surface area for gas exchange. • A reduced DLCO with normal spirometry and lung volumes may suggest anemia. • In patients with restrictive lung disease, a reduced DLCO suggests that the restrictive physiology is due to a process intrinsic to the lung (e.g., idiopathic pulmonary fibrosis). A normal DLCO would indicate that restriction is due to something outside the lungs (e.g., chest wall or neuromuscular disorders) • Patients with pulmonary hypertension in the absence of underlying parenchymal lung disease often have an isolated decrease in their DLCO but otherwise normal spirometry and lung volumes. • In patients with diffuse alveolar hemorrhage, the DLCO may actually be elevated as the intra-alveolar red blood cells take up the carbon monoxide administered during the test quite readily. Question 3.4: A series of flow volume loops are shown below, with volume on the X axis and flow on the Y axis. The expiratory phase is represented by the top portion (flow is positive) and the inspiratory phase is represented by the bottom portion (flow is negative). A B Question 3.4 Which of the flow volume loop above is most consistent with the pulmonary function test results provided earlier in this case A. Figure A correct and explanation B. Figure B incorrect, please try again Question 3.4 Explanation The patient in this case has severe obstruction, characterized by an FEV1 between 30% and 50%. The expiratory phase is represented by the top portion of the graph (positive flow and volume). The flow volume loop in obstructive lung disease typically has a “scooped out” appearance due to prolongation of the expiratory phase. Panel B shows the typical pattern seen in patients with restrictive defects. The curve often has a short, “stubby” appearance (or convex pattern2) and expiration ends after a small volume has been expired. Case 4 A 25 year-old man presents to his physician with complaints of dyspnea and wheezing. He is a non-smoker. Two years ago, he was in a major motor vehicle accident and was hospitalized for 3 months. He had a tracheostomy placed because he remained on the ventilator for a total of 7 weeks. His tracheostomy was removed 2 months after his discharge from the hospital. His pulmonary tests are as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) Actual 4.73 2.56 54 Pre-Bronchodilator (BD) Predicted % Predicted 4.35 109 3.69 69 85 Question 4.1 How would you characterize the results of his pulmonary function tests? A. Normal spirometry incorrect, please try again B. Consistent with a restrictive process incorrect, please try again C. Mild obstructive defect incorrect, please try again D. Moderate obstructive defect > correct & explanation E. Severe obstructive defect incorrect, please try again Question 4.1 Explanation The patient has a low FEV1 and FVC and a low FEV1/FVC ratio, consistent with an obstructive process. The FEV1 is 69% of predicted, indicating that the patient has a moderate obstructive defect. Question 4.2 The flow-volume loop for this patient is provided below. Based on this flow-volume loop, how can you further characterize this patient’s pulmonary function abnormality: A. B. C. D. E. No upper airway obstruction incorrect, please try again Variable intrathoracic upper airway obstruction incorrect, please try again Variable extrathoracic upper airway obstruction incorrect, please try again Fixed upper airway obstruction correct & explanation Unilateral mainstem bronchus obstruction incorrect, please try again Question 4.2 Explanation When interpreting pulmonary function tests, it is important to look at the flow volume loops and not just look at the numbers. The reason for doing so is that occasionally the flow volume loop will take on a characteristic appearance suggestive of a particular diagnosis that might not be apparent from looking at the numbers alone. In addition to the patterns typically seen in obstructive and restrictive processes described in the previous case, there are four patterns that might appear on flow volume loop in patients with obstructive physiology that would change your differential diagnosis and affect your further diagnostic work-up. • Variable Intrathoracic Obstruction (Panel ___): This is caused by lesions within the intrathoracic airways (i.e., within the chest cavity) that obstruct the lumen of the airway but move in response to airway pressure changes during the respiratory cycle. In such cases, there is flattening of the expiratory portion of the flow-volume loop. An example of such a process would be tracheobronchomalacia in which there is breakdown of the cartilaginous rings that support the airway structure leading to airway collapses on exhalation. • Variable Extrathoracic Obstruction (Panel ___): This pattern is caused by lesions within the extrathoracic airways (i.e., outside the chest cavity) that obstruct the lumen of the airway but move in response to airway pressure changes during the respiratory cycle. In such cases, there is flattening of the inspiratory portion of the flow-volume loop. An example of a process that could cause this problem would be a mobile thyroid mass compressing the trachea. • Fixed Airway Obstruction (Panel ___): This pattern is caused by either an intrathoracic or extrathoracic lesion that obstructs the airway lumen but does not move in response to airway pressure changes during the respiratory cycle. In such cases, there is flattening of both the inspiratory and expiratory limbs of the flowvolume loop. An example of a process that could cause this abnormality would be tracheal stenosis or bulky lymphadenopathy encasing the trachea. • Differential Emptying From The Two Lungs (Panel ___): In some cases, one lung empties normally on exhalation, while emptying of the other lung is delayed due to some process occluding the airway. In such cases, the flow volume loop will appear to have two phases: (1) a rapidly descending portion of the expiratory limb representing emptying of the normal lung and (2) a flat portion of the expiratory limb represents the delayed emptying on the obstructed side. Such a pattern might be seen with a tumor obstructing one of the mainstem bronchi. This patient’s flow volume loop shows flattening of both the inspiratory and expiratory limbs, indicating that he has some process obstructing the airway that does not move with the respiratory cycle. This would be consistent with a fixed airflow obstruction (Panel ___ above). Given that he previously had a tracheostomy, this pattern would raise suspicion that he might have tracheal stenosis due to granulation tissue formation at the tracheostomy site. He needs further work-up including bronchoscopy to evaluate this issue. This case illustrates why it is important to look at the flow-volume loops when interpreting pulmonary function tests. If all one did was look at the numerical results, the patient would be labeled as having airflow obstruction and, given his age, would in all likelihood be given the diagnosis of asthma. With this diagnosis, he would be started on inhaled corticosteroids and bronchodilators which, given the likely diagnosis, would not improve his symptoms and, instead, would only serve to delay definitive diagnosis. Identifying the true problem by analyzing the flow volume loop will ensure he gets the appropriate work-up and treatment. Case 5 A 41 year-old woman presents to the General Internal Medicine Clinic complaining of dyspnea with mild exertion. She has a 10 pack-year history of smoking and a history of using intravenous drugs including heroin and Ritalin (methylphenidate). Her pulmonary function tests are as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 0.90 3.09 29 0.49 2.57 19 54 83 3.83 1.49 257 4.78 4.44 108 80 33 0.75 24.85 3 Post- BD Actual % Change 0.74 - 17 0.44 -10 59 8 Question 5.1 How would you classify the pattern of test results for this patient? A. Normal spirometry and lung volumes incorrect, try again B. Obstructive pattern correct & explanation C. Restrictive pattern incorrect, try again D. Mixed obstructive and restrictive patterns incorrect, try again Question 5.1 Explanation She has air flow obstruction as seen by reduced FEV1/FVC in addition to a reduced FEV1 and FVC. TLC is within normal limits, so she does not have either restriction or a mixed obstructive and restrictive pattern. Her FEV1 is 19% predicted and therefore her airflow obstruction would be classified as “very severe”. Question 5.2 Her pulmonary function tests reveal which of the following? A. Air trapping & bronchodilator response incorrect, please try again B. Air trapping & reduced DLCO correct & explanation C. Hyperinflation & bronchodilator response incorrect, please try again D. Hyperinflation & reduced DLCO incorrect, please try again E. Reduced DLCO & bronchodilator response incorrect, please try again Question 5.2 Explanation Her RV is 257% predicted and she therefore has air-trapping. Her TLC is 108% of predicted and does not meet criteria for hyperinflation. Her DLCO is reduced to 3% of the predicted value. She does not have a bronchodilator response as her FEV1 and FVC are both decreased following bronchodilator administration. Question 5.3 Her flow volume loop is as follows: Which of the following is true regarding her flow volume loop? A. Normal incorrect, please try again B. Airflow obstruction without airway obstruction correct, explanation C. Variable extrathoracic airway obstruction incorrect, please try again D. Variable intrathoracic airway obstruction incorrect, please try again E. Fixed airway obstruction incorrect, please try again Question 5.3 Explanation This flow volume loop represents airflow obstruction without airway obstruction. She has a concave expiratory limb consistent with the very severe airflow obstruction seen on her pulmonary function tests. The inspiratory and expiratory limbs are not flattened as would be seen if she had an obstructing lesion in her airway (e.g., a tumor) causing her airflow obstruction. Question 5.4 Her chest radiograph is below. Taking into account her history and physical pulmonary function test results (very severe obstruction, air trapping, reduced DLCO), flow volume loop showing airflow obstruction without airway obstruction, and her chest radiograph above, what is the most likely clinical diagnosis? A. Ritalin lung correct & explanation B. Chronic obstructive pulmonary disease due to tobacco use incorrect, please try again C. Idiopathic pulmonary fibrosis incorrect, please try again D. Hypersensitivity pneumonitis incorrect, please try again E. Pulmonary hypertension incorrect, please try again Question 5.4 Explanation Given her relatively young age and the fact that she has only a 10-pack-year history of smoking, COPD secondary to tobacco use (centrilobular emphysema) would be an unlikely diagnosis. These patients typically present later in life and often have a more significant history of tobacco use. The noteworthy feature of her chest radiograph is that the bibasilar lung fields are hyperlucent (i.e., there is a paucity of lung markings in those areas and illustrated by the white arrows). Additionally, the minor fissure on the right is shifted upward (black arrow), indicating that the lower lungs are hyper-inflated. These findings are distinct from those seen smoking-related centrilobular emphysema which tends to preferentially affect the upper lung zones more than the lower lung zones The presence of basilar predominant emphysematous changes should raise concern for two possible diagnoses that can cause precocious airflow obstruction and a basilar predominant pattern of emphysematous changes typical of paraseptal emphysema: α1 antitrypsin and Ritalin lung. The latter is a form of emphysema that has been described in intravenous drug users who injected methylphenidate and is caused by reaction to talc that is used in the preparation of the methylphenidate and is injected into the circulation along with the active drug.3,4 To distinguish between these two entities, you would rely on clinical history (in this case, the patient has a history of IV Ritalin use) as well as laboratory testing to rule out alpha-one antitrypsin deficiency. Case 6 A 30 year-old woman presents for evaluation of a two-month history of dyspnea on exertion. She is a life-long non-smoker with no prior history of asthma or other pulmonary problems. She works as a receptionist at a publishing company. She has two cats and several parakeets at home. Her pulmonary function testing is as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 1.73 4.37 40 1.57 3.65 43 91 84 1.01 1.98 51 2.68 6.12 44 38 30 5.13 32.19 16 Post- BD Actual % Change 1.79 4 1.58 0 88 -3 Her flow volume loop is as follows: Question 6.1 How would you classify the pattern of test results for this patient? A. Normal spirometry and lung volumes incorrect, try again B. Obstructive pattern incorrect, try again C. Restrictive pattern due to an intrinsic pulmonary process correct & explanation D. Restrictive pattern due to a problem extrinsic to the lung incorrect, try again E. Mixed obstructive and restrictive patterns incorrect, try again Question 6.1 Explanation Her results show reduced FEV1 (43% predicted), reduced FVC (40% predicted) but a preserved FEV1/FVC ratio. This pattern on spirometry is consistent with a restrictive lung process and the diagnosis of restriction is confirmed by the fact that she has a reduced TLC. The DLCO can be used to help sort out whether the restrictive process is due to something intrinsic to the lung, such as interstitial lung disease, or a process extrinsic to the lung, such as a neuromuscular disorder. When restriction is due to a process involving the lung parenchyma, the DLCO will be reduced, indicating that the surface area for gas exchange is impaired, as you would expect in a process affecting the lung parenchyma. If the restrictive process is due to something outside the lung, you would expect the pulmonary parenchyma and surface area for gas exchange to be normal, in which case the DLCO would be normal. This patient’s DLCO is markedly reduced suggesting that the cause of her restriction lies within the pulmonary parenchyma Question 6.2 How would you grade the severity of her restrictive process? A. Mild incorrect, please try again B. Moderate incorrect, please try again C. Severe correct & explanation D. Very Severe incorrect, please try again Explanation to Question 6.2 As noted earlier in Case 2, the severity of the restriction can be classified using the TLC. 65-80% mild restriction 50-65% moderate restriction <50% severe restriction There is no category for “very severe” restriction as there is with obstructive processes. This patient’s TLC is 44% of predicted prior to treatment and, as a result, she would be labeled as having a “severe” restrictive process. Question 6.3 What would be the next appropriate step in this patient’s diagnostic work-up? A. CT Pulmonary Angiogram incorrect, please try again B. High resolution Chest CT correct & explanation C. Upright and supine spirometry incorrect, please try again D. Maximum inspiratory and expiratory pressure measurements incorrect, please try again E. Echocardiogram incorrect, please try again Explanation to Question 6.3 When a patient has evidence of restriction with a reduced DLCO, you should always consider a process intrinsic to the lung as the cause of this abnormality. In particular, you should be concerned about some form of interstitial lung disease and the most appropriate diagnostic study to order would be a high resolution Chest CT. Such a study involves taking thinner slices of the lungs which provide greater detail in the images and allow better assessment of the parenchymal changes. This study also includes expiratory images which allow you to distinguish whether there is evidence of air-trapping and prone images which allow you to determine whether opacities seen in the dependent lung zones on the supine images are due to atelectasis or interstitial lung disease. A CT pulmonary angiogram would be used to rule out pulmonary embolism. Upright and supine spirometry can be used to determine if a patient has diaphragmatic weakness when you see a restrictive pattern with a normal DLCO while maximum inspiratory and expiratory pressures can be used to assess for respiratory muscle weakness when you see a restrictive pattern with a normal DLCO. Further evaluation including a high resolution Chest CT (shown below) revealed that this patient had hypersensitivity pneumonitis, likely secondary to her exposure to parakeets at home. The parakeets were removed from her home and she was given a course of oral corticosteroids. Following treatment, her repeat pulmonary function tests were improved as was the CT scan of her chest. The pre- and post-treatment pulmonary function tests and CT images are shown below: Pulmonary Function Tests Pre-Treatment Test Actual Predicted % Pred. FVC (L) 1.73 4.37 40 FEV1 (L) 1.57 3.65 43 FEV1/FVC 91 84 (%) RV (L) 1.01 1.98 51 TLC (L) 2.68 6.12 44 RV/TLC (%) 38 30 DLCO corr 5.13 32.19 16 Post-Treatment Actual Predicted % Pred. 3.00 4.35 69 2.40 3.63 66 80 83 0.70 3.70 19 13.61 1.99 6.11 30 32.04 35 61 42 CT Scan Images Single slices of the Chest CT in the pre- and post-treatment period. The pre-treatment image on the left shows extensive “ground glass” opacities. This is best appreciated by comparing the whiter dependent lung zones with the more normal-appearing anterior lung zones as well as the darker areas in the periphery of her lung. Ground glass opacities are a non-specific finding indicative of some type of alveolar-filling process. The alveoli can be filled with blood, edema fluid or an inflammatory process. The CT scan does not make that distinction and further diagnostic work-up would be necessary to determine the etiology of these opacities. The post-treatment image on the right shows resolution of the ground glass opacities. Case 7 A 73 year-old man presents with progressive dyspnea on exertion over the past one year. He reports a dry cough but no wheezes, sputum production, fevers or hemoptysis. He is a life-long non-smoker and worked as a lawyer until retiring 3 years ago. He likes to hunt and fish in his leisure time. His pulmonary function testing is as follows: His pulmonary function tests are shown below: Test FVC (L) FEV1 (L) FEV1/FVC (%) FRC RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 1.57 4.46 35 1.28 3.39 38 82 76 1.73 3.80 45 1.12 2.59 43 2.70 6.45 42 41 42 5.06 31.64 16 His flow-volume loop is as follows: Question 7.1 Taking into account his flow-volume loop and pulmonary function tests, what would you expect to see on plain chest radiography? A. Flattened diaphragms incorrect, please try again B. Bilateral interstitial opacities correct & explanation C. Narrow mediastinal contour incorrect, please try again D. Large lung volumes incorrect, please try again Question 7.1 Explanation The reduced DLCO, suggests that the restrictive defect is due to an intraparenchymal process rather than an extraparenchymal process. Choice B the pattern you would expect to see in idiopathic pulmonary fibrosis, a disease process that typically causes the pulmonary function test abnormalities seen in this case and the diagnosis this patient was ultimately found to have. His chest radiographs and images from his Chest CT scans are shown below. Flattened diaphragms, narrow mediastinal contour and large lung volumes are all findings that you would see on plain chest radiography in patients with chronic obstructive pulmonary disease. PA and Lateral Chest X-Ray PA and lateral chest radiographs show diffuse reticular markings bilaterally, mostly at the bases. Question 7.2 What would be the next appropriate step in this patient’s diagnostic work-up? A. Cardiopulmonary exercise test incorrect, please try again B. Dobutamine stress echocardiography incorrect, please try again C. High resolution Chest CT correct & explanation D. Bronchoscopy with bronchoalveoloar lavage incorrect, please try again E. Open lung biopsy incorrect, please try again Question 7.2 Explanation When patients are found to have a low total lung capacity and reduced DLCO on pulmonary function testing and the chest radiography findings shown above, suspicion is raised for interstitial lung disease. The appropriate next diagnostic step would include a high resolution CT scan of the chest. Depending on the findings on that study, the patient may or may not be referred for an open lung biopsy. In the hands of a trained pulmonologist, a typical history in conjunction with classic radiographic findings is enough to make the diagnosis of idiopathic pulmonary fibrosis, the diagnosis the patient in this case had. If there are any findings on CT imaging suggestive of an alternative diagnosis, then bronchoscopy with BAL and/or open lung biopsy will be pursued. Chest CT Images Two slices from a high resolution CT scan of the chest showing characteristic findings of idiopathic pulmonary fibrosis including septal thickening and traction bronchiectasis that are more prominent in the periphery (sub-pleural regions). Case 8 A 64 year-old woman presents with complaints of dyspnea and orthopnea. She is a lifelong non-smoker. Her pulmonary function testing is as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 1.00 2.51 40 0.81 2.00 41 81 80 1.15 1.55 74 2.08 4.04 52 55 39 24.06 30.8 80 Post- BD Actual % Change 1.02 3 0.69 13 67 10 Question 8.1 How would you classify the pattern of test results for this patient? A. Normal spirometry incorrect, please try again B. Obstructive pattern incorrect, please try again C. Restrictive pattern correct & explanation D. Mixed obstructive and restrictive pattern incorrect, please try again Question 8.1 Explanation Her pulmonary function tests are consistent with a restrictive pattern. The FEV1 and FVC are reduced with a normal FEV1/FVC ratio Her TLC is less than 80% predicted, confirming the finding of restriction. Question 8.2 Please grade the severity of her observed defect: A. Mild incorrect, please try again B. Moderate correct & explanation C. Severe incorrect, please try again D. Very severe incorrect, please try again Question 8.2 Explanation Restriction is graded by the decrement in TLC: • • • > 65% and < 80% predicted: mild restriction > 50% and < 65% predicted: moderate restriction < 50% predicted: severe restriction In this case, her TLC is 52% predicted which would be labeled as “moderate” in severity. Question 8.3 Her spirometry is repeated with her in the upright and supine positions: Test FVC (L) FEV1 (L) FEV1/FVC (%) Upright 0.49 0.82 0.60 Supine 0.37 0.68 0.54 Which of the following diagnoses could account for the findings on the upright and supine spirometry and her initial testing shown above? A. B. C. D. Pulmonary hypertension incorrect, please try again Congestive heart failure incorrect, please try again Interstitial lung disease incorrect, please try again Diaphragmatic weakness correct & explanation Question 8.4 Explanation This patients pulmonary function testing is most consistent with diaphragmatic weakness. She has a restrictive process with a preserved DLCO, which suggests that the cause of her restriction is an extra-parenchymal process such as diaphragmatic paralysis/weakness or some form of neuromuscular disorder. To help distinguish between these two possibilities, patients with this pattern of pulmonary function test results will typically undergo two additional tests: (1) repeat spirometry in the upright and supine positions, which helps identify diaphragmatic weakness and (2) measurement of maximum inspiratory and expiratory pressures, which helps identify neuromuscular weakness. When spirometry is performed in the upright and supine positions, a decrease in the FEV1 and FVC of more than 20%, in the supine position is consistent with diaphragmatic weakness. These parameters decrease when the patient assumes the supine position because gravity is no longer available to assist descent of the diaphragm on inspiration. The weakened diaphragm is unable to push against the abdominal contents. This prevents the patient from taking a full breath which, therefore, limits the amount of air the patient can exhale on a forced maneuver. In addition, when the abdominal muscles contract on exhalation the abdominal contents move in a cephalad direction. Without gravity and in a weakened state, the diaphragm cannot resist this movement, leading to a decrement in expiratory volumes. Case 9 A 35 year-old previously healthy man presents with a 2-month history of dyspnea, fevers, chills and night sweats. He is a non-smoker with no concerning habits or occupational exposures. His pulmonary function tests are as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) Pre-Bronchodilator (BD) Actual Predicted % Predicted 1.66 4.48 37 0.94 3.67 26 57 82 1.39 1.66 84 3.06 5.96 51 45 29 Question 9.1 How would you classify the pattern of test results for this patient? A. Normal spirometry incorrect, please try again B. Obstructive pattern incorrect, please try again C. Restrictive pattern incorrect, please try again D. Mixed obstructive and restrictive pattern correct & explanation Question 9.1 Explanation His FEV1 and FVC are both reduced with a reduced FEV1/FVC ratio, indicating the presence of an obstructive pattern. However, his TLC is also reduced, indicating that he also has a restrictive defect. This pattern would therefore be labeled as a “mixed obstructive and restrictive defect.” Question 9.2 Please grade the severity of the observed abnormality: A. Mild incorrect, please try again B. Moderate incorrect, please try again C. Severe incorrect, please try again D. Very severe correct & explanation Question 9.2 Explanation The severity of mixed obstructive-restrictive processes is graded by the decrement in the FEV1: • • • • > 80% predicted: mild > 50% and < 80% predicted: moderate > 30% and < 50% predicted: severe < 30% predicted: very severe His FEV1 is 26% of predicted and, as a result, this would be graded as a very severe mixed obstructive-restrictive process. Question 9.3 His flow volume loop is as follows: This flow-volume loop is most consistent with which of the following findings? A. No upper airway obstruction incorrect, please try again B. Variable intrathoracic upper airway obstruction incorrect, please try again C. Variable extrathoracic upper airway obstruction incorrect, please try again D. Fixed upper airway obstruction incorrect, please try again E. Unilateral mainstem bronchus obstruction correct & explanation Question 9.2 Explanation This patient’s flow-volume loop is consistent with a unilateral mainstem bronchus obstruction. Note that the expiratory limb has two components – a steep component in early exhalation and then a flatter component over the latter half of exhalation (see arrows in the diagram below). This pattern suggests that one lung is emptying faster than the other. Steep initial portion Flattening of the later portion of the expiratory limb This patient then underwent a chest radiograph which revealed a dense opacity in the right chest and shift of the mediastinal contents to the left. A follow-up CT scan revealed a large mass compressing the right mainstem bronchus (shown by the black arrow in his CT images below). The mass was so large that it caused shift of the mediastinal contents to the left side of the chest causing significant restrictive physiology in the left lung. Chest CT Case 10 A 53 year-old woman presents with increasing dyspnea on exertion. She denies cough, fevers, hemoptysis, weight loss or sweats. She was previously an active runner but has had to cut back significantly because of the worsening dyspnea. She does note occasional chest pain with exercise but has not had any syncope or palpitations. Her pulmonary function tests are as follows: Pre-Bronchodilator (BD) Test Actual Predicted % Predicted FVC (L) 2.38 2.87 83 FEV1 (L) 1.95 2.31 84 FEV1/FVC (%) 82 81 RV (L) 1.69 1.58 107 TLC (L) 4.26 4.36 98 RV/TLC (%) 40 36 DLCO corr 9.96 23.25 43 DLCO is measured in ml/min/mmHg Post- BD Actual % Change 2.23 -6 1.93 -1 87 Question 10.1 Based on the results of this testing, what would be the most appropriate next diagnostic or therapeutic step for this patient? A. Start an inhaled corticosteroid incorrect, try again B. Start a short-acting inhaled beta-agonist incorrect, try again C. Refer for bronchoscopy with bronchoalveolar lavage incorrect, try again D. Order a High Resolution Chest CT scan incorrect, try again E. Order an echocardiogram correct & explanation Question 10.1 Explanation Her FEV1/FVC ratio is above 0.8, her FEV1 and FVC are both above 80% and her TLC is normal. She therefore has no evidence of obstruction or restriction. She does, however, have an isolated decrease in her DLCO. An isolated decrease in the DLCO is highly suggestive of some form of pulmonary vascular disease, such as pulmonary arterial hypertension and the next most appropriate diagnostic test to work up this issue would, therefore, be an echocardiogram. Anemia is another process that can result in normal pulmonary function tests and flow-volume loops with reduced DLCO and this can be ruled out with appropriate laboratory testing.2 In terms of the other answer choices, the patient does not have any evidence of an obstructive process that would warrant either inhaled corticosteroids or inhaled bronchodilators. In the absence of a restrictive process, neither bronchoscopy or a CT scan would be indicated. This patient was referred for echocardiography and found to have pulmonary hypertension. Subsequent work-up revealed that she had chronic thromboembolic disease as the source of her elevated pulmonary artery pressures. Question 10.2 How would you characterize the severity of the reduction in her DLCO? A. Mild incorrect, try again B. Moderate correct & explanation C. Severe incorrect, please try again Question 11.2 Explanation The severity of abnormalities in DLCO can be characterized as follows2: Mild: 60% < DLCO < lower limit of normal (lower 5th percentile for reference population) Moderate: 50% < DLCO < 64% Severe: DLCO < 50% Her DLCO is 43% predicted and, therefore, is considered to be severely decreased. Case 11 A 36 year-old woman presents with a several month history of worsening dyspnea on exertion and exercise limitation. She is a life-long non-smoker and has no history of asthma or other known pulmonary diseases. She had to stop going out with her weekly running group because she can no longer keep up with her friends. Her pulmonary function testing is as follows: Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Pre-Bronchodilator (BD) Actual Predicted % Predicted 0.88 3.34 26 0.87 2.87 30 99 86 1.61 1.40 115 2.49 4.73 53 65 29 22 26.6 82 Question 11.1 How would you classify the pattern of test results for this patient? A. Normal spirometry incorrect, please try again B. Obstructive pattern incorrect, please try again C. Restrictive pattern correct & explanation D. Mixed obstructive and restrictive pattern incorrect, please try again Question 11.1 Explanation Her pulmonary function tests show a restrictive defect. The FEV1 and FVC are reduced with a preserved FEV1/FVC ratio. The reduced TLC confirms the presence of restriction. This patient was sent for further pulmonary function testing. She had a 17% drop in her FVC and a 12% decrease in her FEV1 when testing was performed in the supine position. Her maximum inspiratory pressures was – 35 cm H20 (normal ~ 100-120 cm H2O) and her maximum expiratory pressure was - 50 cm H20 (normal ~ 80-100 cm H2O). Her peak cough flow was 180 L/min (normal > 250 L/min). Question 11.2 Which of the following diagnoses would be consistent with the pattern of results in her pulmonary function testing? A. Neuromuscular weakness correct & explanation B. Idiopathic pulmonary fibrosis incorrect, please try again C. Pulmonary hypertension incorrect, please try again D. Hypersensitivity pneumonitis incorrect, please try again E. Diaphragmatic weakness incorrect, please try again Question 11.3 Explanation A restrictive pattern can be seen with neuromuscular weakness, diaphragmatic weakness, idiopathic pulmonary fibrosis or hypersensitivity pneumonitis. When it occurs in the absence of parenchymal lung disease, pulmonary hypertension is usually associated with normal lung volumes and spirometry and an isolated decrease in the DLCO. This patient has a normal diffusion capacity for carbon monoxide. The preserved diffusion capacity suggests that her restrictive pattern is probably due to an extraparenchymal process. Of the four choices that can cause a restrictive pattern, diaphragmatic weakness and neuromuscular disease are two extra-parenchymal processes that can cause such a pattern. When patients are found to have a restrictive defect due to an extra-parenchymal process, two additional sets of tests are indicated: • Upright and supine spirometry to assess the adequacy of diaphragm function • Maximum inspiratory and expiratory pressures and a peak cough flow measurement to assess the adequacy of respiratory muscle strength. (Expiratory flow during cough is highly dependent on having adequate inspiratory and expiratory muscle strength). The additional testing performed in her case suggests that of the two likely possible diagnoses, she most likely has some form of neuromuscular disease. Her FVC and FEV1 both decline by less than 20% when testing was repeated in the supine position, making diaphragmatic weakness less likely. The maximum inspiratory and expiratory pressures are reduced below normal, as is her peak cough flow. These results strongly suggest that she has weak respiratory muscles. She was subsequently referred to a neurologist and diagnosed with limb girdle muscular dystrophy. Case 12 A 44 year-old woman with cirrhosis secondary to chronic alcohol abuse and Hepatitis C presents with complaints of increasing dyspnea. She reports that her dyspnea is worse when she is sitting upright or walking but improves when she is lying flat. She is an active cigarette smoker. On exam, her oxygen saturation while breathing air is 88% in the standing position and 96% in the supine position. Her pulmonary function testing is as follows. Test FVC (L) FEV1 (L) FEV1/FVC (%) RV (L) TLC (L) RV/TLC (%) DLCO corr Actual 3.94 3.2 82 1.89 5.67 33 10.22 Pre-Bronchodilator (BD) Predicted % Predicted 3.69 107% 3.03 105% 82 1.86 102 5.40 105 33 28.22 36 Post- BD Actual % Change 3.86 -2 2.85 3 DLCO is measured in ml/min/mmHg Question 12.1 Which of the following is the most likely diagnosis? A. Chronic obstructive pulmonary disease incorrect, try again B. Hypersensitivity pneumonitis incorrect, try again C. Pulmonary vasculitis incorrect, try again D. Portopulmonary hypertension incorrect, try again E. Hepatopulmonary syndrome correct & explanation Question 12.1 Explanation Her FVC, FEV1, FEV1/FVC, and TLC are normal. Her DLCO is reduced. As discussed in Case 10, an isolated decrease in the DLCO is suggestive of a pulmonary vascular process. Of the items on this list, portopulmonary hypertension and hepatopulmonary syndrome are two pulmonary vascular processes that can be seen in patients with advanced cirrhosis. The latter is a disorder in which the patients develop small intrapulmonary shunts, referred to as intrapulmonary vascular dilatations. Both disorders can be associated with this pattern of results on pulmonary function testing. Further testing would be needed to confirm the diagnosis but certain features of her history and initial diagnostic work-up suggest that she has hepatopulmonary syndrome. She reports that her dyspnea is worse in the upright position, a symptom referred to as “platypnea”;while her oxygen saturation gets worse in the upright position, a sign referred to as “orthodeoxia.” These findings are seen in hepatopulmonary syndrome because the intrapulmonary vascular dilatations that are the hallmark of this disorder are typically present in the bases of the lungs. When the patients are in the upright position, more blood flow goes to the lower lung zones and, as a result, they have more shunt physiology in this position and, as a result, greater dyspnea and lower arterial oxygen tensions. The diagnosis of hepatopulmonary syndrome is confirmed by doing an arterial blood gas shunt study, perfusion scan or contrast echocardiography. A preliminary diagnosis of portopulmonary syndrome is usually made by measuring pulmonary artery pressures using echocardiography. References 1. Evans SE, Scanlon PD. Current practice in pulmonary function testing. Mayo Clin Proc. 2003;78(6):758 2. Pellegrino R, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26(5):948 3. Miller MR, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-338. 4. Stern EJ, et al. Panlobular pulmonary emphysema caused by i.v. injection of methylphenidate (Ritalin): findings on chest radiographs and CT scans. AJR Am J Roentgenol 1994;162(3):555-560. 5. Schmidt RA, et. al. Panlobular emphysema in young intravenous Ritalin abusers. Am Rev Respir Dis 1991;143(3):649-656.