Niacin deficiency is also commonly associated with diarrhea, which
advertisement

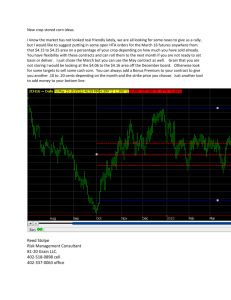
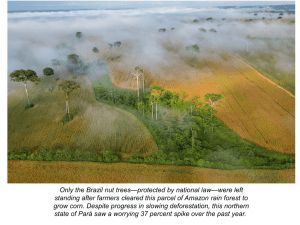
Corn and Pellagra Margaret Monfee October 18, 2000 Anthropology 570 Corn is a food eaten throughout the world. It is easy to produce and cheap so that in the past it has composed a large part of the diet of the poor who could not afford other foods. The consumption of corn as ones main food source can cause health problems due to a deficiency of the B vitamin niacin that if not treated can lead to insanity and even death. This paper will attempt to present a brief history of pellagra, concentrating primarily on the twentieth century American south, and discussing the causes of the disease, its progression in the human body and treatment. The first documented description of pellagra was 1735 in Europe by a Spanish physician, Gaspar Casal. He wrote, “Since I never saw a more disgusting indigenous disease, I thought I should explain its characteristics.”(Etheridge 9). Called mal de la rosa, this was a major source of sickness and death among the very poor. In the following years the disease was described many times by Italian physicians and was soon recognized throughout Europe, Egypt, and South Africa. In the early twentieth century it was common in the United States, especially in the south (Roe 1). The disease attacked the poor who were unable to afford only the cheapest diet that had little variety such as meal, molasses, and “fat back” (Harkness 434). Most of these poor were farmers, in the United States it was often found in sharecroppers (Roe 1) or those who lived in industrial communities with little income (Middleton 1209). Statistics indicate that pellagra was the most severe nutritional deficiency disease recorded in United States history (Park et al. 727). Pellagra is caused by a deficiency of the B vitamin niacin in the diet. Niacin refers to both nicotinic acid and nicotinamide. Nicotinamide is a component of two coenzymes, nicotinamide-adenine dinucleotide (NAD) and nicotinamide-adenine 2 trinucleotide (NADP) (Selhub 221). These coenzymes are involved in oxidationreduction reactions and are essential for metabolic processes in each cell in the body. A deficiency in niacin decreases the cellular function throughout the body. One symptom of niacin deficiency is diarrhea, which is one of the four D’s of pellagra-diarrhea, dermatitis, dementia, and death (Rhoads 7). Pellagra is both easy and difficult to diagnose. Symptoms can vary throughout a population, but once the characteristic symmetrical lesions appear it is fairly easy to diagnose. In early stages it might be confused with sunburn or poison oak, but it is not until the skin begins to peel that the diagnosis can be certain (Etheridge 7). Pellagra adversely affects all systems of the body with the most striking involvement occurring in the skin, nervous system and gastrointestinal tract. Patients are apathetic, anorexic, pale, and weak. The skin over exposed surfaces and pressure points becomes thickened, hyperkeratotic and hyperpigmented. This symmetric dermatosis is most apparent in areas exposed to the sun, which seems to trigger the lesions. Neurologic manifestations include peripheral neuropathy and encephalopathy with dementia in various degrees of severity. Involvement of the gastrointestinal tract is common including lesions around the angles of the mouth and atrophic changes in the tongue. Atrophic lesions of the stomach and bowel may cause severe diarrhea (Selhub 221). These clinical manifestations of pellagra are usually divided into four stages: (1) when the patient feels unwell but has no definite symptoms; (2) the stage of redness of the exposed areas of the skin and various digestive disturbances and some central and peripheral nervous disturbances; (3) stage of severe neurological disturbances; and (4) the cachectic stage, which is usually terminal (Roe 3). These stages usually follow a 3 seasonal pattern with the first vague symptoms occurring after Christmas and more definite symptoms usually appearing in mid-February, gradually growing worse until May or June and then began to lessen (Etheridge 3). Chronic suffers may endure this annual cycle for many years. The first stage is characterized by indefinite symptoms such as loss of appetite, abdominal pain, flatulence and usually diarrhea. Constipation may occur instead but diarrhea is more common although in some cases the individual may alternate between the two. There may be some nervous symptoms at this stage such as headache, pain in the neck and back, hypersensitivity to touch, dizziness, and muscle weakness, especially of the legs. This first stage may last for a few weeks or it may last several years. During the second stage the mouth becomes extremely sore and the tongue becomes glossy and inflamed (Etheridge 7). Next appear a redness of exposed skin, which is an important characteristic for diagnostic purposes. These skin lesions appear on portions of the body exposed to light such as on the hands and arms, on the tops of the feet and around the ankles, on the back of the neck or in a butterfly-shaped design across the nose (Etheridge 7). They are characterized by redness and symmetry that can first be confused with sunburn, which it closely resembles during the first few days. The skin soon begins to peel leaving a border of brownish pigmentation where the lesions were (Roe 4). In the United States two types of skin lesions were recognized: wet and dry. The wet lesions were accompanied by an exudation of serum (Roe 4). These symptoms generally last from three to four months and nervous symptoms have usually already developed at the peak of this stage. The skin of the affected areas may remain darker in color and sometimes rough and dry for some time. The symptoms 4 seem to disappear completely but more outbreaks will occur without treatment and with each reoccurrence the severity of the symptoms increases (Roe 4). The third stage is characterized by severe cerebrospinal disturbances. Abnormal sensations in the skin such as itching on the backs of hands and occasionally feet, burning in the stomach, shoulder region, feet, hands and arms are observed. A dull headache and dizziness are common complaints. It is during this stage that that it psychological symptoms occur such as depression, interference with thought, slowness of ideas, and mild irritability. Sometimes weakness of the muscles is found and spasms and painful cramps. The muscle weakness may progress to partial paralysis (Roe 5). The fourth stage shows increasing weight loss, disappearance of subcutaneous fat, diminished strength and an inability to resist infection. The patient may become bedridden because of weakness. There is usually severe diarrhea. Without treatment death occurs during this phase, due to a weakened heart, tuberculosis, which individual with pellagra are very susceptible to, or the inability of the body to fight infections. These are the basic symptoms and progression of pellagra. Symptoms can vary because of the complexity of the disease. It has been said that the deficiency of niacin “creates a number of secondary deficiencies and that the symptoms are compounded of the multiple deficiencies” (Roe 7). It is because of the many possible secondary symptoms that the skin lesions are essential to diagnosis. In addition to the physical effects, psychological effects also occur. Sometimes so severely that institutionalization is necessary. Individuals could suffer melancholy or delusions of persecution, where their neighbors were trying to assassinate them. They were frequently confused and had hallucinations; illusions of pregnancy were common 5 among women. Some had destructive tendencies; they might pull out their eyebrows or try to set their houses on fire. Suicides were common in this stage. Nurses in asylums had to watch to prevent patients from drowning themselves in the bathtub, this method seemed especially common with women. Some suicides attributed to pellagra were of a man who threw himself under a train, another who drank carbolic acid and a third who beat his head against a wall. Pellagra was so frequently associated with suicide that in 1915, the year when the number of cases of pellagra in Mississippi reached its highest peak, the 120 percent increase in the number of suicides that year was attributed to the sharp jump in the incidence of pellagra (Etheridge 8). It is interesting to note that while many individuals ended up in institutions because of pellagra that the institutions themselves caused pellagra in its previously healthy inhabitants because of poor diet. At a mental institution in Illinois in 1909, where there was no previous incidences of pellagra, the superintendent admitted that there were one hundred and thirty well-defined cases that had caused forty-five deaths (Etheridge 6). With a change in the diet of the inhabitants no new cases of pellagra were reported. Reports similar to these not only came from mental institutions but also from orphanages, mill villages, and prisons (Etheridge 6). There was a great deal of controversy over the cause of pellagra. It had been blamed on eating spoiled and unspoiled corn, the buffalo gnat, housefly, or mosquito and attempts to treat it ranged from arsenic compounds to electric shock (Etheridge). It had long been thought that pellagra was infectious. Not until the twentieth century was the true cause of pellagra discovered. 6 In the early 1900’s pellagra was present to some extent in every state in the United States but it was in the south where it was most prevalent (Park et al. 727). In many southern states during the years of 1928 and 1929, when pellagra was at its peak, it was the eight or ninth highest cause of death excluding accidents in the south (Park et al. 727). One of the reasons that it was so serious in the south was that most available land was used for nonfood crops such as tobacco and cotton so that corn was a major part of the diet, especially of poor farmers (Park et al. 727). One of the most important figures in discovering the cause of and eliminating pellagra in the United States was Joseph Goldberger. He was an epidemiologist and a member of the United States Public Health Service and was appointed to evaluate the pellagra problem. He made his first report in June of 1914, after an inquiry into incidences of the disease in mental hospitals. He reported that if pellagra were infectious there would have been a high change of attendants contracting the disease but this did not occur. Looking for environmental factors that might distinguish the nurses from the patients he found that the nurses were able to select the best food in the institutions and supplemented their diets by buying food when they were off duty. He did not believe that corn or corn products caused pellagra but that an abundance of corn with other cereals could be harmful. He urged that hospitals limit the amount of grains and increase the amount of fresh animal foods, such as meat, eggs and milk (Roe 101-102). One study conducted by Goldberger on the nutritional basis of pellagra was at the Rankin Prison Farm. He received permission from Mississippi Governor Earl Brewer for this study and Brewer announced to the approximately eighty convicts that a pardon could be obtained by agreeing to submit to a diet of white flour, corn meal, hominy grits, 7 cornstarch, white rice, cane sugar, cane syrup, sweet potatoes, pork fat, cabbage, collards, turnips, turnip greens, and coffee. No milk, lean meat, eggs, or legumes were allowed. There were many volunteers for the study and Goldberger chose twelve, all of whom were white, half of them serving life sentences for murder (Harkness 464). The twelve men, who became known as the “Pellagra squad”, were isolated and placed under special guard so they could be kept under close observation. They were on this special diet from April 19, 1915 to October 31, 1915 and during this same time thirty-five convicts at the same institution were kept under observation but were fed from the “farm” kitchen as they were accustomed to (Roe 104). Eleven members of the “pellagra squad” remained on the special diet for the complete period with seven developing distinctive skin lesions. Some of the skin changes beginning on the scrotum suggests that some of the subjects had a diet induced riboflavin deficiency which are now known to cause such lesions. Goldberger was convinced that the early skin changes and other symptoms of illness such as weight loss, weakness, and abdominal discomfort were symptoms of pellagra. In retrospect, the experiment did induce pellagra but was probably limited to those who late in the study developed more characteristic pellagrous dermatosis (Roe 104). The control group showed no signs of pellagra (Roe 104). Goldberger though that the experimental diet lacked some essential protein component, probably an amino acid, and that it might also be vitamin deficient. These concepts could not be proven then but were later found to be close to the truth. He was cautious about claiming that the situation in the prison reproduced the situation occurring in endemic pellagra because the diets of pellagrins and prisoners were somewhat different (Roe 104). 8 Despite Goldberger’s studies it was still not completely accepted that pellagra was induced by a dietary deficiency. In an effort to disprove that pellagra was infectious Goldberger persuaded sixteen other members of the American Public Health Service to join him and his wife in an experiment to assess its transmissibility. Each had inoculations of skin squames from people with pellagra, had nasal excretions applied to the mucosa of their noses, and ingested stool samples on rice cakes (Middleton) or mixed with flour and administered in pill form (Roe 103). Blood samples were also injected intramuscularly (Roe 103). Immediate side effects were diarrhea after eating the “pills” and pain at the injection site but during a period of observation lasting seven months none of the subjects developed pellagra (Roe 103). It was assumed that this disease could no longer be considered infectious and supporters of the theory that it was contagious lapsed. Corn is a staple in many cultures and not all of them are infested with pellagra. Mexico is an example of this, corn consumption is high with much less wheat, milk, and meat being eaten but there is no pellagra problem. One factor was the greater consumption of beans in Mexico but another is the method of processing the corn (Carpenter). The corn is soaked in an alkaline solution of lime that softens the corn, and splits the niacin from its bound form and makes it nutritionally available (Carpenter). This in combination with the tryptophan, an amino acid that the human body can convert to niacin, present in the germ prevents development of pellagra (Carpenter). There were few reported cases of death from pellagra reported each year in the first decade of the twentieth century but by the mid 1910’s the annual number of death passed one thousand with the peak being about seven thousand in 1928 when it began to decline (Parks et al. 732). Studies of dietary patterns in the proceeding decades show no 9 major dietary changes except for the methods by which corn was processed. Before 1905 corn was stone-ground, the problem with this method was that the germ of the corn contained a great deal of oil that made corn meal go rancid quickly during storage (Carpenter). The development of the Beall degerminator at the beginning of the century allowed production of a more stable de-germed corn meal and allowed the farmers to gain an additional income from the oil produced from the germ. The germ composed only about 10% of the grain but it contained 60% of the tryptophan. Much of the niacin remained in the de-germed meal but as corn matures most of the niacin is in a form that is traditionally unavailable (Carpenter). Because of this change in corn production the body could not absorb sufficient niacin to prevent pellagra. There are two main causes for the eradication of pellagra in the United States. The first is the inclusion of more meat, milk, eggs, and yeast in the diet as a result of nutritional studies. Goldberger had discovered the effects of using yeas by treating blacktongue, a form of pellagra in dogs, and confirmed the results at a mental institution in Georgia (Etheridge 178-179). The American Red Cross distributed brewer’s yeast in areas where pellagra was endemic and it had an almost immediate positive effect (Carpenter). The decline in mortality from pellagra from 1928 through 1932 was probably due to these dietary changes (Park et al. 736) The second and most effective cause of the decline in pellagra was fortification of grain products. In 1938, bakers voluntarily began enriching their bread with high-vitamin yeast and a large decline in pellagra deaths occurred the following year (Parks et al. 736). Synthetic niacin became available to physicians in late 1938, and it contributed to the decrease in pellagra but the production of synthetic vitamins was too low and the cost to 10 high to contribute a significant decrease (Parks et al. 737). During the 1940’s the Food and Drug Administration began formulating guidelines for enriched grain products and various states implemented mandatory enrichment laws. By the end of the decade 26 states had enrichment laws for flour and bread and five states had enrichment laws for cornmeal and corn grits (Parks et al. 733). Pellagra deaths decreased steadily with enrichment of food. Mississippi is an example of the effectiveness of the mandatory enrichment programs. In 1946 the pellagra morbidity rate in the state was 101 per 100,000 with the mandatory enrichment of bread, flour, cornmeal and corn grits in place the morbidity rate dropped to 1 per 100,000 in 1947 (Parks et al. 736). [See Chart] This is a dramatic change in a short period of time and the rate of pellagra continued to be low although the consumption of animal-derived foods decreased during this time (Parks et al 736). Pellagra is a disease of poverty and malnutrition. Through the works of Joseph Goldberger and others like him a body of knowledge has been complied that has almost completely eradicated the disease in the United States. This easily preventable disease will no longer cause illness, insanity and death in the lives of even the poorest of our citizens. 11 (Park et al 736) 12 Works Cited Carpenter Kenneth J. 1999 Vitamin deficiencies in north america in the 20th century. Nutrition Today, 39:233. Etheridge Elizabeth W. 1972. The butterfly caste: a social history of pellagra in the south. Westport, Connecticut: Greenwood Publishing Company. Harkness Jon M. 1996. Prisoners and pellagra. Public Health Reports, 111:463-468. Middleton John. 1999. The blues and pellagra: a public health detective story. British Medical Journal, 319;1209. Park Youngmee K., Christopher T. Sempos, Curtis N. Barton, John E. Vanderveen, and Elizabeth A. Yetley. 2000. Effectiveness of food fortification in the united states: the case of pellagra. American Journal of Public Health, 90:727-738. Rhoads Jonathan E. 1984. The history and development of nutritional assessment of the hospitalized patient. In Wright Richard A., Heymsfield, Steven and McManus, Clifford B., editors. Nutritional Assessment. Boston, Oxford: Blackwell Scientific Publications, Inc. p3-11. Roe Daphne A. 1973. A plague of corn: the social history of pellagra. Ithaca, London: Cornell University Press. Selhub Jacob, and Irwin H. Rosenberg. 1984. Assessment of vitamin depletion. In Wright Richard A., Heymsfield, Steven and McManus, Clifford B., editors. Nutritional Assessment. Boston, Oxford: Blackwell Scientific Publications, Inc. p209-238. 13