Urology
advertisement
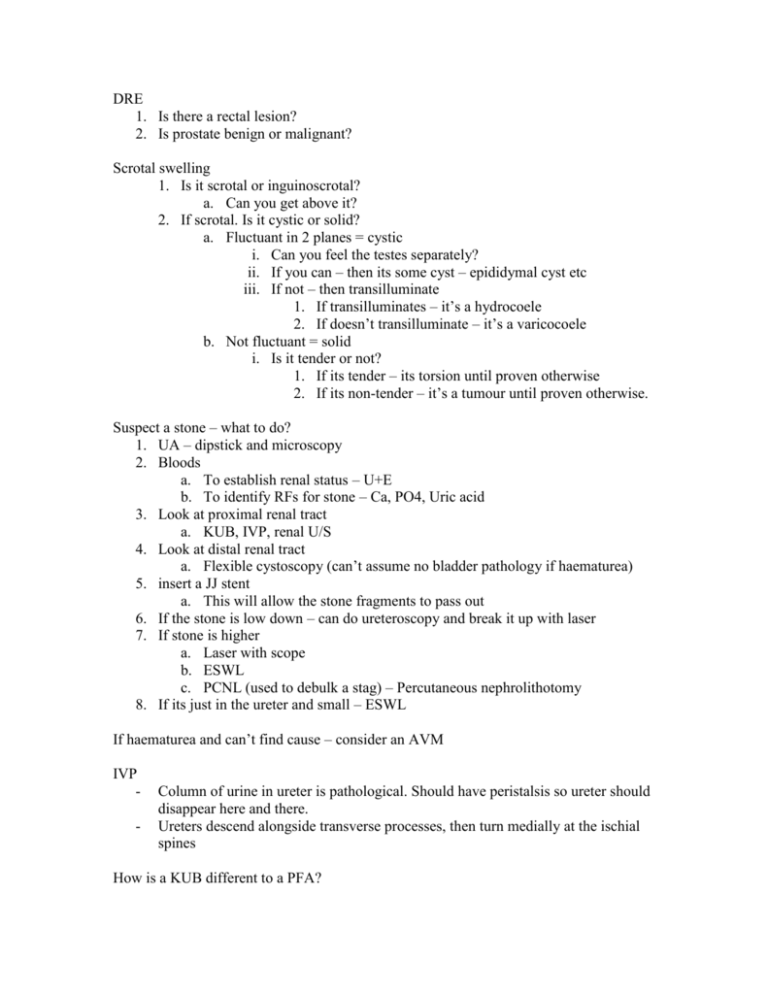
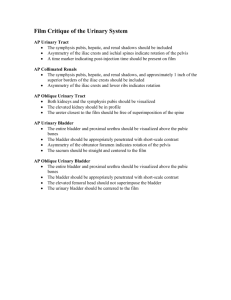
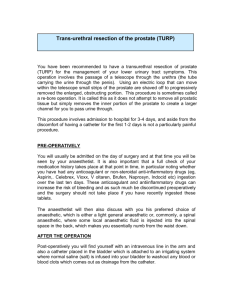
DRE 1. Is there a rectal lesion? 2. Is prostate benign or malignant? Scrotal swelling 1. Is it scrotal or inguinoscrotal? a. Can you get above it? 2. If scrotal. Is it cystic or solid? a. Fluctuant in 2 planes = cystic i. Can you feel the testes separately? ii. If you can – then its some cyst – epididymal cyst etc iii. If not – then transilluminate 1. If transilluminates – it’s a hydrocoele 2. If doesn’t transilluminate – it’s a varicocoele b. Not fluctuant = solid i. Is it tender or not? 1. If its tender – its torsion until proven otherwise 2. If its non-tender – it’s a tumour until proven otherwise. Suspect a stone – what to do? 1. UA – dipstick and microscopy 2. Bloods a. To establish renal status – U+E b. To identify RFs for stone – Ca, PO4, Uric acid 3. Look at proximal renal tract a. KUB, IVP, renal U/S 4. Look at distal renal tract a. Flexible cystoscopy (can’t assume no bladder pathology if haematurea) 5. insert a JJ stent a. This will allow the stone fragments to pass out 6. If the stone is low down – can do ureteroscopy and break it up with laser 7. If stone is higher a. Laser with scope b. ESWL c. PCNL (used to debulk a stag) – Percutaneous nephrolithotomy 8. If its just in the ureter and small – ESWL If haematurea and can’t find cause – consider an AVM IVP - Column of urine in ureter is pathological. Should have peristalsis so ureter should disappear here and there. Ureters descend alongside transverse processes, then turn medially at the ischial spines How is a KUB different to a PFA? - a KUB is longer because it includes the kidneys, ureters and bladder - get a neurogenic bladder This can cause 1. OAB/detrusor instability/urge incontinence o Treat with anticholinergics 2. Retention and overflow incontinence o Treat with CISC 3. a bit of both to decide which one – can do urodynamics MS - Urinary bypass – this is when you have a catheter and OAB – the strength of contraction of the detrusor muscle is so strong that urine sprays past the catheter and can even spit out the catheter, balloon and all. Treatment options include botox. CISC – Clean Intermittent Self-Catheterisation 1. How often do you do it? – 4-6 times per day is normal 2. What volume is passed each time? Sting procedure – this is for reflux (eg in a child) – you move the angle of the ureters to get rid of the reflux. Can also inject botox around the ureters. Undescended testes 1. Is it in the scrotum? 2. If not, is this maldescent or is it retractile 3. Oar’s test – squat – a retractile testes will go down Orchidoplexy – to bring down a maldescended to testes – incision in groin, incision in scrotum. Ideally do before age 2. BPH Investigations: - urinalysis – UTI?, +/- urine culture - FBC, U+E (renal function), creatinine - Post void residual volume – normal is <100ml - Urodynamics? - Transrectal prostate US – to determine size? - IVP? - Cystoscopy Management – medical and surgical - Medical o Alpha1-receptor blockers – tamsolusin – omnic/tamnic o Antiandrogens acting selectively on prostate- finasteride o Intermittent self-catheterisation o Balloon dilatation and stenting of prostate - Surgical o TURP – transurethral resection of prostate o Open prostatectomy Cystoscopy should be done before TURP. TURP. Very common procedure for BPH. Involves removal of the adenomatous portion of the prostate. Complications are acute and late. Acute complications are: - Post-op haemorrhage - Failure to void - Urinary retention due to clots - UTI - TURP syndrome – occurs in 2% of patients. During TURP, about 900ml of fluid is used for irrigation, and this is absorbed into the extra/intravascular space through open venous sinuses in the prostatic capsule. This fluid is electrolyte-free. Usually the absorption is well tolerated, but occasionally patients can develop TURP syndrome – a hyponatraemic, hypochloraemic metabolic acidosis. Late complications are: - impotence - incontinence - retrograde ejaculation - bladder neck contractures/ urethral stricture. TRBP – Trans rectal biopsy of the prostate carries a 2% risk of fatal sepsis. Only do if truly indicated. Causes of U/L ureteric obstruction: 1. Intra-luminal a. stone b. clot 2. Mural a. Stricture b. Tumour c. PUJ obstruction d. VUJ obstruction 3. Extra-mural a. Retroperitoneal fibrosis (idiopathic, secondary to malignancy or irradiation, or drugs like beta-blockers) b. Pregnancy c. Vascular d. Pelvic tumours Causes of B/L ureteric obstruction 1. bladder outlflow obstruction – prostate, stricture, clot… 2. pelvic tumours 3. extensive bladder tumour 4. retroperitoneal tumours 5. retroperitoneal fibrosis. Causes of haematuria can be general and local. General – anticoagulants, bleeding disorders Local – work from top of system down. GN, RCC, pyelonephritis… stone…bladder tumour, UTI… What investigations to do? - UA + microscopy (red cells, white cells, casts, crystals, bacteria), Bloods (FBC, U+E, coag), image proximal renal tract (renal US, +/- IVP) and distal tract (flexible cystoscopy) RFs for UTI: - urinary tract obstruction - instrumentation of the urinary tract – eg catheter - neurogenic bladder - diabetes mellitus - vesicoureteric reflux - immunosuppression - pregnancy UTI’s can be caused by an ascending infection (e.coli), or by haematogenous spread (IV drug users, TB, infective endocarditis) RFs for pyelonephritis: - vesicoureteric reflux - obstruction – congenital (PUJ obstruction) or acquired (stricture, stone) - anatomical – short urethra in females - neurogenic bladder - Diabetes mellitus - Haematogenous spread from skin or GIT Most common organism involved in acute pyelonephritis? – e.coli. Proteus mirabilis and Klebsiella also cause pyelonephritis. These are urease-splitting organisms that create an alkaline urine secondary to the release of ammonia, and this allows the precipitation of struvate stones in the renal pelvis and calyces. Chronic pyelonephritis results in parenchymal scarring of the kidney. It is often the consequence of reflux and infections in childhood. Adults typically present with azotemia or hypertension. Do renal US, IVP. If a single kidney only is involved, the contralateral kidney will often show compensatory hypertrophy. Acute bacterial prostatitis Features include pyrexia, rigors, low back pain, perineal discomfort, dysuria, urinary frequency, urgency. Causes are e.coli in 80% of cases, other common causes are pseudomonas and enterococcus. O/E, prostate will be tender, swollen, warm and firm. Often accompanied by acute cystitis. Chronic bacterial prostatitis is the most common cause of relapsing urinary tract infection in men. May be asymptomatic, or varying degrees of irritative urinary symptoms. Symptoms of lower urinary tract obstruction: - weak stream – hows the flow? - Hesitancy do you ever have trouble starting the flow? - Intermittency ever have to start and stop? - Dribbling – any dribbling afterwards? - straining to void – ever have to strain a lot? Irritative symptoms: - Frequency – how often do you go? - Urgency - Nocturia – ever have to get up at night? How many times? - Dysuria – any burning or stinging or passing water? - urge incontinence – do you ever not make it to the loo? DDx of lower urinary tract obstruction: The problem can be structural or functional. Working from the top down… Structural causes include… - carcinoma of the bladder - stricture of bladder neck - BPH or prostates ca - Posterior urethral valves (young boy) - Urethral stricture (long-term catheter) - Meatal stricture - Phimosis Functional causes include… - Neurogenic bladder dysfunction - Psychogenic voiding difficulties - Cystitis - Prostatitis, prostatic abscess - Balanitis