Table 12-1
advertisement

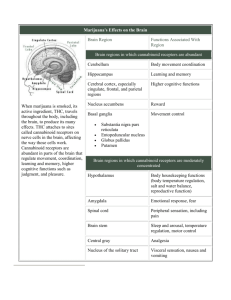
Table 12-1. Specificity of Innate and Adaptive Immunity Innate immunity Adaptive immunity Specificity For structures shared by classes of microbes ("molecular patterns") For structural detail of microbial molecules (antigens); may recognize nonmicrobial antigens Receptors Encoded in germline; limited diversity Encoded by genes produced by somatic recombination of gene segments; greater diversity Distribution of Nonclonal: identical receptors on all cells of the same lineage receptors Clonal: clones of lymphocytes with distinct specificities express different receptors Discrimination Yes; host cells are not recognized or they may express molecules of self and that prevent innate immune reactions nonself Yes; based on selection against self-reactive lymphocytes; may be imperfect (giving rise to autoimmunity) Table 12-2. Examples of Molecular Patterns of Microbes and Pattern Recognition Receptors of Innate Immunity Molecular pattern of Source microbe Pattern recognition receptor of innate immunity Principal innate immune response dsRNA Replicating viruses Toll-like receptor? Type I interferon production by infected cells LPS Gram-negative bacterial cell wall Toll-like receptor/CD14 Macrophage activation Unmethylated CpG nucleotides Bacterial DNA Toll-like receptor Macrophage activation N-formylmethionyl peptides Bacterial proteins N-formylmethionyl peptide receptors Neutrophil and macrophage activation Mannose-rich glycans Microbial glycoproteins or glycolipids 1. Macrophage mannose receptor 2. Plasma mannose-binding lectin 1. Phagocytosis 2. Opsonization, complement activation Phosphorylcholine and related molecules Microbial membranes Plasma C-reactive protein Abbreviations: dsRNA, double-stranded RNA; LPS, lipopolysaccharide. Opsonization, complement activation Table 12-3. Components of Innate Immunity Components Principal functions Barriers Epithelial layers Prevent microbial entry Defensins Microbial killing Intraepithelial lymphocytes Microbial killing Circulating effector cells Neutrophils Early phagocytosis and killing of microbes Macrophages Efficient phagocytosis and killing of microbes, secretion of cytokines that stimulate inflammation NK cells Lysis of infected cells, activation of macrophages Circulating effector proteins Complement Killing of microbes, opsonization of microbes, activation of leukocytes Mannose-binding lectin (collectin) Opsonization of microbes, activation of complement (lectin pathway) C-reactive protein (pentraxin) Opsonization of microbes, activation of complement Coagulation factors Walling off infected tissues Cytokines TNF, IL-1, chemokines Inflammation IFN-α,-β Resistance to viral infection IFN-γ Macrophage activation IL-12, IL-18, IL-23 IFN-γproduction by NK cells and T cells IL-15 Proliferation of NK cells IL-10, TGF-β Control of inflammation BOX 12-1 Toll-like Receptors The Toll-like receptors (TLRs) are a family of membrane proteins that serve as pattern recognition receptors for a variety of microbe-derived molecules and stimulate innate immune responses to the microbes expressing these molecules. The first protein to be identified in this family was the Drosophila Toll protein, which is involved in establishing the dorsal-ventral axis during embryogenesis of the fly as well as mediating antimicrobial responses. Ten different mammalian TLRs have so far been identified on the basis of sequence homology to Drosophila Toll, and they are named TLR 1 to 10, but more members of the family may exist. All these receptors contain leucine-rich repeats flanked by characteristic cysteine-rich motifs in their extracellular regions and a Toll/IL-1 receptor (TIR) homology domain in their cytoplasmic region, which is essential for signaling. TIR domains are also found in the cytoplasmic tails of the IL-1 and IL-18 receptors, and similar signaling pathways are engaged by TLRs, IL-1, and IL-18. The TLRs are expressed on many different cell types that are important components of the innate immune system, including macrophages, dendritic cells, neutrophils, mucosal epithelial cells, and endothelial cells. Mammalian TLRs are involved in responses to widely divergent types of molecules that are commonly expressed by microbial but not mammalian cells (see Figure). The innate immune response to one species of microbe may reflect an integration of the responses of several TLRs to different molecules produced by the microbe. Some of the microbial products that stimulate TLR signals include gram-negative bacterial lipopolysaccharide (LPS), grampositive bacterial peptidoglycan, bacterial lipoproteins, lipoteichoic acid, lipoarabinomannan, zymosan, the bacterial flagellar protein flagellin, heat shock protein 60, respiratory syncytial virus fusion protein, unmethylated CpG motifs, and double-stranded RNA. In many cases, a single TLR is responsible for stimulating inflammatory responses to a particular microbial ligand, such as TLR9-mediated responses to CpG. However, the repertoire of specificities of the TLR system is apparently extended by the ability of TLRs to heterodimerize with one another. For example, dimers of TLR2 and TLR6 are required for responses to peptidoglycan. In some cases, one of the TLRs of a heterodimer may confer ligand-binding specificity, and the other TLR may be required for signaling. Specificities of the TLRs are also influenced by various non-TLR accessory molecules. This is most thoroughly understood for TLR4 and its ligand LPS. LPS first binds to soluble LPS-binding protein (LBP) in the blood or extracellular fluid, and this complex serves to facilitate LPS binding to CD14, which exists as both a soluble plasma protein and a glycophosphatidylinositollinked membrane protein on most cells except endothelium. Once LPS binds to CD14, LBP dissociates, and the LPS-CD14 complex physically associates with TLR4. An additional extracellular accessory protein called MD2 also binds to the complex with CD14. LPS, CD14, and MD2 are all required for efficient LPSinduced signaling, but it is not yet clear if direct physical interaction of LPS with TLR4 is necessary. Different combinations of accessory molecules in TLR complexes may serve to broaden the range of microbial products that can induce innate immune responses. For example, both CD14 and MD2 are associated with complexes of other TLRs (e.g., TLR2), and TLR4 may form complexes with other accessory molecules, such as MD1 and RP105, in certain cell types, such as B lymphocytes. The predominant signaling pathway used by TLRs results in the activation of NF-κB (see Figure). In this pathway, ligand binding to the TLR at the cell surface leads to recruitment of several cytoplasmic signaling molecules through specific domain-domain interactions. The first protein to be recruited is a cytoplasmic adapter protein that probably binds to the TIR domain of the TLR. The adapter protein that binds to most TLRs is called MyD88, but some TLRs may recruit other proteins and trigger MyD88-independent signaling pathways. The second protein to be recruited into the signaling complex is called IL-1 receptor-associated kinase (IRAK). IRAK contains a domain that mediates interactions with MyD88 and a serine/threonine protein kinase domain. On recruitment, IRAK undergoes autophosphorylation, dissociates from MyD88, and activates TNF-R-associated factor-6 (TRAF-6). TRAF-6 then activates the IκB kinase cascade, leading to NF-κB activation. This same pathway is involved in IL-1-and IL-18-induced activation of NF-κB. In some cell types, certain TLRs also engage other signaling pathways, such as the MAP kinase cascade, leading to activation of the AP-1 transcription factor. The relative importance of these additional pathways of TLR signaling and the way the "choice" of pathways is made are not well understood. The genes that are expressed in response to TLR signaling encode proteins important in many different components of innate immune responses. These include inflammatory cytokines (TNF-α, IL-1, and IL-12), endothelial adhesion molecules (E-selectin), and proteins involved in microbial killing mechanisms (inducible nitric oxide synthase). The particular genes expressed will depend on the responding cell type. Killing of Phagocytosed Microbes BOX 12-2 Physiologic and Pathologic Responses to Bacterial Lipopolysaccharide Bacterial lipopolysaccharide (LPS or endotoxin) is a product of gram-negative bacteria, and a potent stimulator of innate immune responses that enhance killing of the bacteria, but it may also cause significant pathologic changes in the host. LPS is a mixture of fragments of the outer cell walls of gram-negative bacteria and contains both lipid components and polysaccharide moieties. The polysaccharide groups can be highly variable and are the major antigens of gram-negative bacteria recognized by the adaptive immune system. The lipid moiety, by contrast, is highly conserved and is an example of a molecular pattern recognized by the innate immune system. LPS induces local and systemic inflammation, and many of the features of tissue injury observed in infection by gram-negative bacteria can be mimicked by administration of LPS. LPS is a potent activator of macrophages, and the cellular response involves the LBP/CD14/mammalian Toll-like receptor 4 system, as described in Box 12-1. Macrophages, which synthesize and express CD14, can respond to minute quantities of LPS, as little as 10 pg/mL, and cells that lack CD14 are generally unresponsive to LPS. However, some CD14 is shed and circulates as a plasma protein. Addition of soluble CD14 to cells that are normally unresponsive to LPS, such as vascular endothelial cells, allows such cells to respond to LPS, but usually at 100-to 1000-fold higher concentrations than CD14+ macrophages. The genes in macrophages that are induced by LPS encode cytokines and enzymes of the respiratory burst. The functions of these proteins in innate immunity are described in the text. page 285 page 286 The systemic changes observed in patients who have disseminated bacterial infections, sometimes called the systemic inflammatory response syndrome (SIRS), are reactions to cytokines whose production is stimulated by LPS. In mildly affected patients, the response consists of neutrophilia, fever, and a rise in acute-phase reactants in the plasma. Neutrophilia is a response of the bone marrow to circulating cytokines, especially G-CSF, resulting in increased production and release of neutrophils to replace those consumed during inflammation. An elevated circulating neutrophil count, especially one accompanied by the presence of immature neutrophils prematurely released from the bone marrow, is a clinical sign of infection. Fever is produced in response to substances called pyrogens that act to elevate prostaglandin synthesis in the vascular and perivascular cells of the hypothalamus. Bacterial products such as LPS (called exogenous pyrogens) stimulate leukocytes to release cytokines such as IL-1 and TNF (called endogenous pyrogens) that increase the enzymes, especially cyclooxygenase-2, that convert arachidonic acid into prostaglandins. Nonsteroidal anti-inflammatory drugs, including aspirin, reduce fever by inhibiting cyclooxygenase-2 and thus blocking prostaglandin synthesis. An elevated body temperature has been shown to help amphibians ward off microbial infections, and it is assumed that fever does the same for mammals, although the mechanism is unknown. One hypothesis is that fever may induce heat shock proteins that are recognized by some intraepithelial lymphocytes, promoting inflammation. Acute-phase reactants are plasma proteins, mostly synthesized in the liver, whose plasma concentrations increase as part of the response to LPS. Three of the best known examples of these proteins are C-reactive protein, fibrinogen, and serum amyloid A protein. Synthesis of these molecules by liver hepatocytes is up-regulated by cytokines, especially IL-6 (for C-reactive protein and fibrinogen) and IL-1 or TNF (for serum amyloid A protein). During the SIRS, serum amyloid A protein replaces apolipoprotein A, a component of high-density lipoprotein particles. This may alter the targeting of high-density lipoproteins from liver cells to macrophages, which can use these particles as a source of energy-producing lipids. The rise in fibrinogen causes erythrocytes to form stacks (rouleaux) that sediment more rapidly at unit gravity than do individual erythrocytes. This is the basis for measuring erythrocyte sedimentation rate as a simple test for the systemic inflammatory response due to any number of stimuli including LPS. When a severe bacterial infection leads to the presence of organisms and LPS in the blood, a condition called sepsis, circulating cytokine levels increase and the form of the host response changes. High levels of cytokines produced in response to LPS can result in disseminated intravascular coagulation (DIC), caused by mechanisms described below. Multiple organs show inflammation and intravascular thrombosis, which can produce organ failure. Tissue injury in response to LPS can also result from the activation of neutrophils before they exit the vasculature, thus causing damage to endothelial cells and reduced blood flow. The lungs and liver are particularly susceptible to injury by neutrophils. Lung damage in the SIRS is commonly called the adult respiratory distress syndrome (ARDS) and results when neutrophil-mediated endothelial injury allows fluid to escape from the blood into the airspace. Liver injury and impaired liver function result in a failure to maintain normal blood glucose levels due to a lack of gluconeogenesis from stored glycogen. The kidney and the bowel are also injured, largely as a result of reduced perfusion. Overproduction of nitric oxide by cytokine-activated cardiac myocytes and vascular smooth muscle cells leads to heart failure and loss of perfusion pressure, respectively, resulting in hemodynamic shock. The clinical triad of DIC, hypoglycemia, and cardiovascular failure is described as septic shock. This condition is often fatal. TNF produced by LPS-activated macrophages is a major mediator of LPSinduced injury. This is known because many of the effects of LPS can be mimicked by TNF and in mice, anti-TNF antibodies or soluble TNF receptors can attenuate or completely block responses to LPS. IL-12 and IFN-γ also contribute to LPS-induced injury because IL-12 stimulates IFN-γ production by NK cells and T cells, and IFN-γ increases TNF secretion by LPS-activated macrophages and synergizes with TNF in effects on endothelium. Because septic shock is the result of cytokine overproduction, many clinical trials have been introduced to neutralize cytokines, such as TNF and IL-1, with antibodies, soluble receptors, or natural antagonists. The results of these trials have been disappointing, probably because of cytokine redundancy (i.e., the fact that many cytokines contribute to the systemic response in fulminant sepsis). It remains to be seen whether "cocktails" of multiple cytokine antagonists will be more effective. The mechanisms by which LPS induces tissue injury were extensively studied in the rabbit initially by Robert Shwartzman, who had observed that when a rabbit is given a low-dose (subinjurious) intravenous injection of LPS, it will succumb to a second low-dose injection of LPS administered intravenously 24 hours later. The dead animal shows evidence of multiorgan injury and widespread intravascular thrombus formation, a condition that mimics clinical DIC. Thrombosis results from a simultaneous initiation of coagulation by LPSinduced tissue factor (TF) expression and from a down-regulation of natural anticoagulation mechanisms, including a decrease in expression of tissue factor pathway inhibitor (TFPI) and endothelial cell thrombomodulin. A localized form of LPS-mediated tissue injury may be induced by injecting a small dose of LPS into a skin site on a rabbit, followed 24 hours later by a second low dose of LPS administered intravenously. This causes hemorrhagic necrosis of the skin at the site of the first injection. On histologic examination, the tissue shows intravascular thrombosis as well as neutrophil influx, endothelial damage, and hemorrhage. In the local Shwartzman model of skin injury in the mouse, TNF can replace the second dose of LPS, and TNF antagonists prevent tissue injury, further supporting the central role of this cytokine in responses to LPS. Interestingly, the first description of TNF (and the origin of its name) was as an LPS-induced serum factor that mediated hemorrhagic necrosis of experimental tumor implants. TNF-mediated necrosis of tumors histopathologically resembles the local Shwartzman reaction. The current interpretation of these data is that tumors release a factor or factors that act on local endothelium to produce the same changes as the first injection of LPS does in the localized Shwartzman reaction. Intravenous administration of TNF then replaces the second intravenous injection of LPS, invoking a Shwartzman reaction with vascular thrombosis in the tumor and subsequent tumor necrosis. BOX 12-3 Inhibitory and Activating Receptors of NK Cells NK cells recognize and kill infected or malignantly transformed cells, but they do not usually harm normal cells. This ability to distinguish potentially dangerous targets from healthy self is dependent on the expression of both inhibitory and activating receptors. Inhibitory receptors on NK cells recognize class I MHC molecules, which are constitutively expressed on most healthy cells in the body but are often not expressed by cells infected with virus or cancer cells. For the most part, activating receptors on NK cells recognize structures that are present on both NK-susceptible target cells and normal cells, but the influence of the inhibitory pathways dominates when class I MHC is recognized. Some activating receptors recognize class I MHC-like molecules that are expressed only on stressed or transformed cells. Different families of NK cell receptors exist, and many of these receptors have evolved recently, as indicated by their absence in rodents and their structural divergence between chimpanzees and humans. The following discussion focuses on the properties of human NK cell inhibitory and activating receptors, with only brief consideration of murine NK receptors. Numerous human NK inhibitory receptors have been identified, all of which have immunoreceptor tyrosine inhibitory motifs (ITIMs) in their cytoplasmic tails (see Figure). ITIMs recruit cytoplasmic protein tyrosine phosphatases SHP-1 and SHP-2, which dephosphorylate and thereby inactivate signaling intermediates generated by activating receptors on the same cell. Inhibitory NK receptors fall into three main families. The first family to be discovered is called the killer Ig-like receptor (KIR) family because its members contain two or three extracellular Ig-like domains. The KIRs recognize different alleles of HLA-A,-B, and-C molecules. Structural and binding studies indicate that the sequence of the peptides bound to the MHC molecules is important for KIR recognition of MHC molecules. HLA molecule binding to KIRs is characterized by very fast on-rates and off-rates, which would be consistent with the ability of NK cells to rapidly "test" for the presence of MHC expression on many cells in a short time. Furthermore, the inhibitory signals generated in an NK cell by KIR recognition of an MHC molecule are not long-lived, and the same NK cell can quickly go on to kill an MHC-negative target cell. Some members of the KIR family have short cytoplasmic tails without ITIMs, and these function as activating receptors, as discussed in more detail below. Mice do not express KIRs but instead use the Ly49 family of proteins, which have similar class I MHC specificities and ITIMs in their cytoplasmic tails. A second family of inhibitory receptors consists of the Ig-like transcripts (ILTs), which also contain Ig-like domains. One member of this family, ILT-2, has a broad specificity for many class I MHC alleles and contains four ITIMs in its cytoplasmic tail. Interestingly, cytomegalovirus encodes a molecule called UL18 that is homologous to human class I MHC and that can bind to ILT-2. This may represent a decoy mechanism by which the virus engages an inhibitory receptor and protects its cellular host from NK cell-mediated killing. The third NK inhibitory receptor family consists of heterodimers composed of either of the C-type lectins NKG2A or NKG2B covalently bound to CD94. NKG2A and NKG2B have two ITIMs in their cytoplasmic tails. The CD94/NKG2 receptors bind HLA-E, a nonclassical MHC molecule. Stable expression of HLA-E on the surface of cells depends on the binding of signal peptides derived from HLA-A,-B,-C, or-G. Therefore, the CD94/NKG2 inhibitory receptors perform a surveillance function for the absence of HLA-E, classical class I MHC, and HLA-G molecules. As is the case for the KIR receptors, some CD49/NKG2 receptors do not have cytoplasmic ITIM motifs, and these function as NK-activating receptors, as discussed below. The activating receptors on NK cells include several structurally distinct groups of molecules, and only some of the ligands they bind are known. A shared feature of these receptors is their association with signaling molecules that contain immunoreceptor tyrosine-based activation motifs (ITAMs), including FcεRIγ, ζ, and DAP12 proteins. The activating NK receptors engage signaling pathways involving protein tyrosine kinases Syk and ZAP-70 and adapter molecules that are also part of the signaling pathways associated with lymphocyte antigen receptors and Ig Fc receptors (see Chapter 8). CD16, one of the first activating receptors identified on NK cells, is a low-affinity IgG Fc receptor that associates with FcεRIγ and ζ proteins and is responsible for NK cell-mediated antibody-dependent cellular cytotoxicity. A more recently discovered group of human NK-activating receptors, called natural cytotoxicity receptors, includes NKp46, NKp30, and NKp44. These are members of the Ig superfamily; they associate with FcRγ and ζ proteins and are expressed exclusively on NK cells. Although their ligands are not yet known, antibodyblocking studies suggest that they play a dominant role in NK-mediated killing of various tumor target cells. Ligand binding to activating NK cell receptors leads to cytokine production, enhanced migration to sites of infection, and killing activity against the ligand-bearing target cells. page 291 page 292 As mentioned, some members of the KIR and CD94/NKG2 families of MHCspecific receptors do not contain ITIMs but rather associate with ITAM-bearing accessory molecules (such as DAP12) and deliver activating signals to NK cells. These include KIR2DS, CD94/NKG2C, CD94/NKG2E, and CD94/NKG2H. All these receptors are known to recognize normal class I MHC molecules, and it is not clear why these potentially dangerous receptors exist on NK cells. These activating receptors bind class I MHC molecules with lower affinities than the structurally related inhibitory receptors, and it is possible that the activating receptors actually bind MHC-related molecules specifically associated with pathological conditions. This is the case for NKG2D, which is expressed on NK cells, as well as on T cells, and is distantly related to the other NKG2 proteins. NKG2D associates with DAP10, a molecule homologous to DAP12, which contains a PI-3 kinase-binding motif in its cytoplasmic tail rather than an ITAM motif. This receptor recognizes the MICA, MICB, and ULBP molecules in humans and the RAE-1 and H-60 molecules in mice, all of which are encoded in the MHC, have domains homologous to class I MHC α and β domains, but do not display peptides or associate with β2-microglobulin. These NKG2 ligands are not abundantly expressed on normal cells but are upregulated by stress and are often found on tumor cells. Thus, NK cells may use these receptors to eliminate stressed (injured) host cells and tumor cells.