Accounts Receivable Specialist
advertisement
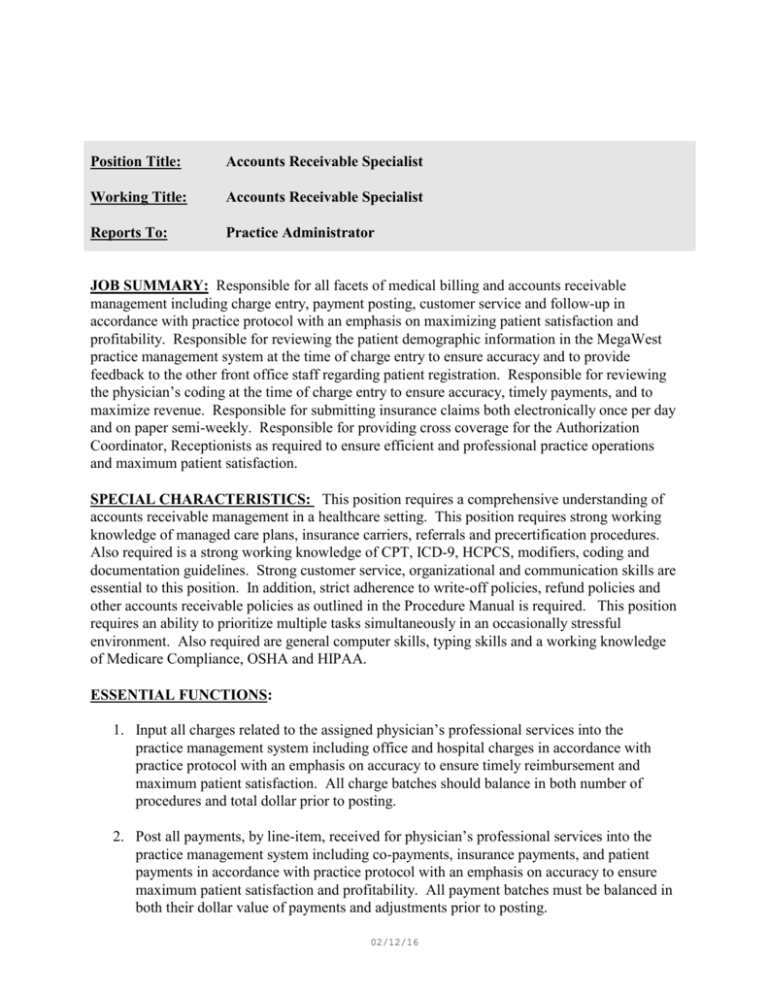
Position Title: Accounts Receivable Specialist Working Title: Accounts Receivable Specialist Reports To: Practice Administrator JOB SUMMARY: Responsible for all facets of medical billing and accounts receivable management including charge entry, payment posting, customer service and follow-up in accordance with practice protocol with an emphasis on maximizing patient satisfaction and profitability. Responsible for reviewing the patient demographic information in the MegaWest practice management system at the time of charge entry to ensure accuracy and to provide feedback to the other front office staff regarding patient registration. Responsible for reviewing the physician’s coding at the time of charge entry to ensure accuracy, timely payments, and to maximize revenue. Responsible for submitting insurance claims both electronically once per day and on paper semi-weekly. Responsible for providing cross coverage for the Authorization Coordinator, Receptionists as required to ensure efficient and professional practice operations and maximum patient satisfaction. SPECIAL CHARACTERISTICS: This position requires a comprehensive understanding of accounts receivable management in a healthcare setting. This position requires strong working knowledge of managed care plans, insurance carriers, referrals and precertification procedures. Also required is a strong working knowledge of CPT, ICD-9, HCPCS, modifiers, coding and documentation guidelines. Strong customer service, organizational and communication skills are essential to this position. In addition, strict adherence to write-off policies, refund policies and other accounts receivable policies as outlined in the Procedure Manual is required. This position requires an ability to prioritize multiple tasks simultaneously in an occasionally stressful environment. Also required are general computer skills, typing skills and a working knowledge of Medicare Compliance, OSHA and HIPAA. ESSENTIAL FUNCTIONS: 1. Input all charges related to the assigned physician’s professional services into the practice management system including office and hospital charges in accordance with practice protocol with an emphasis on accuracy to ensure timely reimbursement and maximum patient satisfaction. All charge batches should balance in both number of procedures and total dollar prior to posting. 2. Post all payments, by line-item, received for physician’s professional services into the practice management system including co-payments, insurance payments, and patient payments in accordance with practice protocol with an emphasis on accuracy to ensure maximum patient satisfaction and profitability. All payment batches must be balanced in both their dollar value of payments and adjustments prior to posting. 02/12/16 3. Post all credit and debit adjustments to patient accounts with strict adherence to the guidelines in the Procedure Manual. 4. File all charge, payment and adjustment batches in the appropriate format by batch date for quick reference. 5. Review the physician’s coding at charge entry to ensure compliance with Medicare guidelines and to ensure accurate and timely reimbursement. 6. Provide customer service both on the telephone and in the office for all patients and authorized representatives regarding patient accounts in accordance with practice protocol. Patient calls regarding accounts receivable should be returned within 2 business days to ensure maximum patient satisfaction. 7. Verify all demographic and insurance information in patient registration of the practice management system at the time of charge entry to ensure accuracy, provide feedback to other front office staff members and to ensure timely reimbursement. 8. Follow-up on all outstanding insurance claims at 60-days from the date of service in accordance with practice protocol with an emphasis on maximizing patient satisfaction and practice profitability. 9. Follow-up on all outstanding patient account balances at 90-days from the date of service in accordance with practice protocol with an emphasis on maximizing patient satisfaction and practice profitability using the A/R aged reports. 10. Provide information pertaining to billing, coding, managed care networks, insurance carriers and reimbursement to physicians, managers and subordinates. 11. Follow-up on all returned claims, correspondence, denials, account reconciliations and rebills within five working days of receipt to achieve maximum reimbursement in a timely manner with an emphasis on patient satisfaction. 12. Submit primary and secondary insurance claims electronically each day and on HCFA semi-weekly to ensure timely reimbursement. 13. Attendance at relevant seminars to remain abreast of current issues regarding obstetric and/or gynecology accounts receivable, Medicare Compliance and HIPAA. 14. Recommend accounts for outside collection when internal collection efforts fail in accordance with practice protocol. 15. Process refunds to insurance companies and patients in accordance with practice protocol. 16. Reconcile the incoming lockbox deposits in accordance with practice protocol as required to ensure timely payment posting. 17. Monitor reimbursement from managed care networks and insurance carriers to ensure reimbursement consistent with contract rates. 02/12/16 18. Monitor the supply and quality of forms, envelopes and supplies as required to perform job functions. 19. Proficiency with all facets of the medical practice management system including patient registration, charge entry, insurance processing, advanced collections, reports and ledger inquiry. 20. Provide cross coverage for the switchboard operator as required to ensure efficient and professional practice operation including lunch and break coverage. 21. Proficiency with WebMD, a web-based program for eligibility verification and claim status, to efficiently conduct accounts receivable follow-up and to maximize revenue. 22. Maintain information regarding coding, insurance carriers, managed care networks and credentialing in an organized easy to reference format. 23. Maintain an organized, efficient and professional work environment. 24. Adhere to all practice policies related to OSHA, HIPAA and Medicare Compliance. 25. Other duties as assigned. SUPERVISES: This position has no supervisory responsibilities. EDUCATION: High school diploma or GED is required. A college degree is preferred. EXPERIENCE: Requires a minimum of 3 years of accounts receivable experience preferably in an obstetrics and/or gynecology setting. SKILLS: 1. The jobholder must demonstrate current competencies applicable to the job position. 2. Requires excellent written and verbal communication skills and strong customer service skills. 3. Requires strong basic mathematical skills. 4. Requires a minimum typing speed of forty (40) words per minute and ten-key by touch. 5. Requires an extensive working knowledge of managed care networks and insurance carriers. 6. Requires an extensive working knowledge of accounts receivable functions including CPT and ICD-9 coding. 7. Requires proficiency in general office automation including operation of fax machines, copy machines, adding machines, postage machines, and multi-line phone systems. 8. Requires proficiency in working with a PC, the Internet, and MS Windows. 9. Requires a good understanding of the current Medicare Compliance, OSHA, and HIPAA regulations. 10. Requires a high degree of organization. 02/12/16 ABILITIES: 1. Ability to establish/maintain cooperative working relationships with staff and providers. 2. Ability to communicate effectively and in a professional manner with patients using interpersonal skills. 3. Ability to communicate effectively and in a professional manner with all staff, managers and physicians. 4. Ability to prioritize and multi-task. PHYSICAL/MENTAL DEMANDS: 1. Combination of sitting, standing, bending, light lifting and walking. 2. Requires a full range of body motion including manual and finger dexterity and hand-eye coordination. 3. Requires corrected vision and hearing to a normal range. 4. Requires the ability to manage stressful situations. 5. Occasional stress from varying demands. OTHER REQUIREMENTS: 1. 2. 3. 4. 5. 6. 7. Restriction of personal phone calls to break and lunch periods. Overtime as authorized by supervisor. Attendance at monthly front office staff meeting. Attendance at monthly all staff meeting. Attendance at training sessions. Adherence to the front office uniform policy. Adherence to practice policies, procedures and protocol. This description is intended to provide basic guidelines for meeting job requirements. Responsibilities, knowledge, skills, and working conditions may change as needs evolve. 02/12/16