word
advertisement

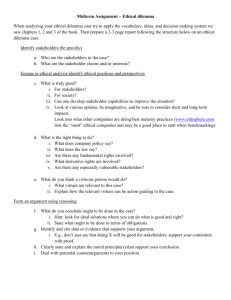
Professional judgement, best interests. The doctor meant to write this… A patient has a prescription for a drug dosage that you believe is unpractical to dispense. For example, the prescription recommends 18 mg and you know that it is more practical to dispense 20mg. In usual circumstances when you have a query about a dosage you contact the doctor to confirm it. The doctor is not contactable however and you are very busy. You know increasing the dosage will be safe for the patient. Should you go ahead and prescribe 20mg because you believe it will be in the patient’s best interests? TUTOR NOTES Responsibility to maintain personal integrity Dilemma: Whether or not to supply medicine considered to be in the best interests of the patient Some possible areas for discussion include: Duties and Responsibilities Patient - welfare/best interests prime concern Rights of Healthcare Professionals and Professionalism Distinction between legal responsibilities and ethical responsibilities Accountability Patient – civil law Society – criminal law Profession and peers – regulatory/disciplinary body Employer – contract of employment Other healthcare professionals Self – professional and personal integrity Professional judgement Acting ethically usually means acting legally, and vice versa Acts can be ethical but not legal and vice versa Ethical aspects o o o o o o Pharmacists primary responsibility the wellbeing and safety of patient and the public Protect rights and interests of patients Relationship between healthcare professional and patient Special obligations - professional-patient Duties of beneficence/non-maleficence Informed consent Principles o o Non-maleficience duty to patient to ensure no harm is done Beneficience - act to benefit patient o o paternalism Respect for autonomy Veracity - truthfulness Faithfulness – faithful to patient’s best interests Justice Deontology: assumes a duty of care to patients to protect from harm Consequentialism: considers consequences of actions for all parties involved Virtues: integrity, honesty, trustworthiness, veracity, courage, fortitude, respect for others, respects patient’s confidences, compassion, fairness, self-control, prudence, etc. Professional aspects Professional duties Professional guidance – professions self-imposed standards o GMC; BMA; RPSGB: NHS/DoH Professional misconduct Professional judgement and accountability Code of Ethics – o 15. Emergencies Risk-benefit analysis Prescription errors o risk management o protocols o audit Dispensing practice and procedures o NB “…and you are very busy.” Legal aspects Medicines Act 1968 and regulations Emergency supply regulations Criminal/civil liability Duty of care and negligence Pharmacist liability for dispensing errors Summary points Those involved in healthcare must be able to provide logical and sustainable explanations for why they acted in the way they did when carrying out their professional duties Accountability applies to all facets of a healthcare professionals work including ethical considerations and judgements Professionals must act within their personal expertise; self-awareness/recognise limits A pharmacist must use his/her professional judgement to decide what course of action is in the best interests of the patient ETHICAL DECISION-MAKING Is the question an ethical one? Legal and professional issues but also ethical issues: Avoiding harm, Doing good, Integrity Step 1 – Gather relevant information Step 2 – Identify type of ethical problem rights and best interests of patient avoiding harm/doing good personal and professional integrity Step 3 – Analyse problem principles of autonomy, non-maleficence; beneficence; virtues Step 4 – explore options/solutions deontological approach – weighing of conflicting principles/conflict of duties – which course of action best respects duties and rights? utilitarian approach – consider all potential consequences (to all parties involved) – what benefits and harms will each course of action produce and which will lead to best overall consequences? virtues approach – which course of action develops moral virtues? alternative courses of action, e.g. supply medication ↪ risks? ↪safety? ↪ quantity? ↪ legal consequences ↪ duty of care/assume greater liability ↪ extend depends on facts refuse to supply ↪ risks? ↪ judgment to determine lack of legitimacy ↪ dosage clue to prescription error? advise patient how to obtain medical care ↪ risks? make an emergency supply ↪ procedure, etc. contact another GP in the practice N.B. frequently, there are no definitive right answers, only answers that are more or less reasonable, more or less defensible: two people may come to an opposite decision using the same information - it depends on how important each consideration is to each person and also the degree to which an individual takes a “deontologist“ or a “consequentialist” approach. Step 5 – make decision Step 6 – assess and reflect Discussion review/links Pharmacist duties, responsibilities and accountability Controlled Drug legislation (and proposals post-Shipman Inquiry) Emergency Supply procedures Protocols Pharmacist’s civil liability and extended duty of care (Amoxil case etc) Prescription interpretation and dispensing Patient medication records