Tori Espersen-Sturges genetics and depression
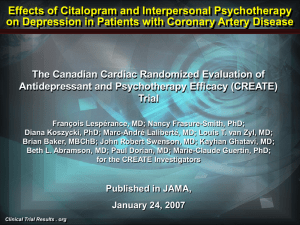
advertisement

Victoria Espensen-Sturges Biology 303 Dr. Ely November 8, 2007 The Genetic Basis for the Effects of Citalopram Treatment of Depression When prescribing medication, physicians must take many things into consideration. It is not enough merely to factor in symptoms and diagnoses, but they must also take into account other medications and family history. This is particularly true in the case of anti-depressants, which have an incredible impact on neurological processes that can, in turn, have a huge holistic effect on the person. Because of the connection between family history and reaction to anti-depressants, research is being done into whether there is a genetic tie between the two. Major depressive disorder is currently the fourth greatest disease burden worldwide.1 It affects five to eight percent of the American adult population and is accompanied by sadness, changes in energy, difficulty concentrating, lack of interest in activities once enjoyed, and thoughts of death or suicide.2 Researchers have been trying to determine what genes contribute to the variations in the level of success of the antidepressant citalopram, commonly marketed as Celexa, as well as what genes contribute to the severity of various side effects associated with the drug. Citalopram belongs to the most common family of anti-depressants, selective serotonin reuptake inhibitors (SSRIs). SSRIs work by controlling the amount and number of serotonin molecules that are absorbed by serotonin receptors to be available for use in the serotonin pathway. Most studies in the past few years have been based on the Sequenced Treatment Alternatives for Depression (hereafter referred to as STAR*D), a study involving thousands of patients who have been diagnosed with major depressive disorder as a database for research into a variety of aspects of depression including causes and treatments. One of the early studies using the STAR*D cohort as a participant base selected 68 candidate genes based on pathways that have been proven to play a role in depression: serotonin, dopamine, dopamine, norepinephrine, and neurotrophins, as well as a few other selected genes. Genes that might play a role but were already being investigated in other studies were disregarded. From these 68 candidate genes, the researchers selected 768 SNPs for examination. In this study, researchers were not looking for genetic links to the cause of depression; rather, they were looking only at a connection between genetic markers and the success rate of citalopram. After DNA analysis of 1,953 participants, statistically significant data related two SNPs on the HTR2A gene to high response and remission rates. Of these two SNPs, the researchers determined that a much stronger correlation was associated with the rs7997012 SNP, and concluded that this played a greater role in determining response to citalopram. HTR2A codes for the serotonin 2A receptors, which help regulate the uptake of serotonin in the brain, thus contributing to how complete, and therefore functional, the serotonin pathway is.2 Interestingly, the allele associated with better treatment outcomes occurred six times more frequently in white participants than in black participants. Overall, the black participants had a much less favorable reaction to the citalopram, leading researchers to question if there was a connection to race or ethnicity and the presence of this allele.1 A subsequent study, published in 2007, cited the original study’s use of association only in the first wave of genotypes to be a substantial flaw. This second study sought to apply a more powerful analysis by utilizing a second wave of genotypic results, hopefully allowing them to definitively address whether groups defined by treatment outcome and a comparative control group differ genetically. Other than this, the methods, phenotypic definitions, and genotyping companies were kept identical to the first study. The same 768 SNPs on 68 candidate genes were studied in 1,816 STAR*D individuals and 634 psychiatrically healthy controls. This time, the results not only yielded a response to the original SNP on the HTR2A gene, rs7997012, but also indicated an association between both total remission and response rate and the rs1954787 SNP on the GRIK4 gene. GRIK4 codes for KA1, the kainic acid-type glutamate receptor. These receptors have recently been found to be crucial to brain plasticity, which then contributes to the development of new pathways and the integration of these new pathways with old pathways.3 The association was most pronounced when an individual was a homozygous carrier of both treatment-response alleles, in which case they were 23% more like to response positively to treatment than were individuals who did not carry the marker alleles. This was the first study done indicating a connection between the GRIK4 gene and outcome of antidepressant treatment, although a concurrent study reported the gene as playing a role in other psychiatric disorders. This result led researchers to question not only the role of GRIK4 in the outcome of treatment, but also the role of the gene in the causes of depression, something that has not been looked at before.4 A few months after this study, a new study emerged that examined the emergence of suicidal ideation in patients on citalopram. This study also utilized the STAR*D database and again examined the same 68 candidate genes and 768 SNPs. In this case, instead of observing how many patients achieved remission or reported fewer, less frequent symptoms of depression, researchers were studying how many patients reported increased thoughts of suicide after a normal course of citalopram treatment. After genotyping these participants, two markers were discovered that had a significant level of association. One of the markers was the rs2518224 SNP on the GRIK2 gene. This gene is from the same family as the GRIK4 gene that played a role in citalopram response in the previous study and also codes for the kainic glutamate receptors. The second SNP, rs4825476 on the GRIA3 gene, codes for the AMPA3 glutamate receptor, suggesting that something in the glutamate pathway is responsible for anti-depressant induced suicidal ideation.5 The implications of this group of studies are astounding for the psychiatric community. Getting psychiatric disorders under control through the right balance of medications as quickly as possible is imperative for the health and safety of the patient. Years of trying different combinations of medications can have a huge impact on the patient’s life, because until they are stable, they cannot continue their lifestyle as it once was. The side effects experienced by the patient can also be an impediment to their once normal routine. The years of psychiatric visits and multiple medications it can take to find the right combination of medication can be incredibly financially draining. If doctors can look at genetic information to determine if these markers are present, they can prescribe medication that is more likely to work immediately as opposed to after trying several other drugs. If the patient has the genetic markers for citalopram induced suicidal ideation, the doctor can avoid suggesting citalopram as a possible treatment approach, again saving the patient’s time, money, and possibly life. References: 1) McMahon, Francis J. et al. "Variation in the Gene Encoding the Serotonin 2A Receptor is Associated with Outcome of Antidepressant Treatment." The American Journal of Human Genetics 78 (2006). 2) Lopez, Juan F. "The Neurobiology of Depression." The Doctor Will See You Now. 2007. Psychiatry and Mental Health Research Institute, University of Michigan. 2 Nov. 2007 <http://www.thedoctorwillseeyounow.com/articles/behavior/depressn_5/>. 3) "Kainate Receptors." Centre for Synaptic Plasticity. 27 Sept. 2005. University of Bristol. 5 Nov. 2007 <http://www.bristol.ac.uk/Depts/Synaptic/info/kainate/kainate_1.htm>. 4) Paddock, Sylvia, et al. "Association of GRIK4 with Outcome of Antidepressant Treatment in the STAR*D Cohort." American Journal of Psychiatry 164:8 (2007). 5) Laje, Gonzalo, et al. "Genetic Markers of Suicidal Ideation Emerging During Citalopram Treatment of Major Depression." American Journal of Psychiatry 164:10 (2007).