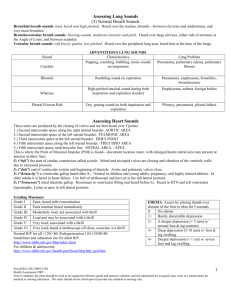
Assessing Lung Sounds (3) Normal Breath Sounds Bronchial breath sounds: loud, harsh and high pitched. Heard over the trachea, bronchi—between clavicles and midsternum, and over main bronchus. Bronchovesicular breath sounds: blowing sounds, moderate intensity and pitch. Heard over large airways, either side of sternum, at the Angle of Louis, and between scapulae. Vesicular breath sounds: soft breezy quality, low pitched. Heard over the peripheral lung area, heard best at the base of the lungs. Crackles ADVENTITIOUS LUNG SOUNDS Characteristics Popping, crackling, bubbling, moist sounds on inspiration Rhonchi Rumbling sound on expiration Pneumonia, emphysema, bronchitis, bronchiectasis High-pitched musical sound during both inspiration and expiration (louder) Emphysema, asthma, foreign bodies Wheezes Dry, grating sound on both inspiration and expiration Pleurisy, pneumonia, pleural infarct Sound Pleural Friction Rub Lung Problem Pneumonia, pulmonary edema, pulmonary fibrosis Assessing Heart Sounds These tones are produced by the closing of valves and are best heard over 5 points: 1.) Second intercostals space along the right sternal boarder. AORTIC AREA 2.) Second intercostals space at the left sternal boarder. PULMONIC AREA 3.) Third intercostals space at the left sternal boarder. ERB’S POINT 4.) Fifth intercostals space along the left sternal boarder. TRICUSPID AREA 5.) Fifth intercostals space, midclavicular line. MITRAL AREA—APEX This is where the Point of Maximal Impulse (PMI) is found—document location (note: with enlarged hearts mitral area may present at anterior axillary line) S1 (“lub”) the start of cardiac contraction called systole. Mitral and tricuspid valves are closing and vibration of the ventricle walls due to increased pressure. S2 (“dub”) end of ventricular systole and beginning of diastole. Aortic and pulmonic valves close. S3 (“Kentucky”) a ventricular gallop heard after S2. Normal in children and young adults, pregnancy, and highly trained athletes. In older adults it is heard in heart failure. Use bell of stethoscope and have pt in the left lateral position. S4 (“Tennessee”) atrial diastolic gallop. Resistance to ventricular filling and heard before S1. Heard in HTN and left ventricular hypertrophy. Listen at apex in left lateral position. EDEMA: Assess by placing thumb over Grading Murmurs dorsum of the foot or tibia for 5 seconds Grade I Faint; heard with concentration 0 No edema Grade II Faint murmur heard immediately 1+ Barely discernible depression Grade III Moderately loud, not associated with thrill 2+ A deeper depression (< 5 mm) w/ normal foot & leg contours Grade IV Loud and may be associated with a thrill 3+ Deep depression (5-10 mm) w/ foot & Grade V Very loud; associated with a thrill leg swelling Grade VI Very loud; heard w/stethoscope off chest, associate w/a thrill 4+ Deeper depression (> 1 cm) w/ severe foot and leg swelling Normal B/P for all <120/<80; Prehypertension 120-139/80-89 Guidelines/education site for adult B/P http://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017 For children & adolescents: http://pediatrics.aappublications.org/content/pediatrics/140/3/e20171904.full.pdf Formula to convert from Fahrenheit to Celsius: (5/9)*(deg F-32) PULSES: Peripheral pulses to convert from Celsius to Fahrenheit: (1.8*deg C)+32 should be compared for rate, 95º F = 35ºC 96ºF = 35.5ºC 98.6ºF = 37ºC 100ºF = 37.7ºC 101ºF = 38.3ºC rhythm, and quality. 102ºF = 38.8ºC 103ºF = 39.4ºC 104ºF = 40ºC 105ºF = 40.5ºC 0 Absent Symptom Analysis: This assists the client in describing the problem. +1 Weak and thready P Provocate/Palliative: What caused it? What makes it better/worse? +2 Normal Q Quality/Quantity: How does it feel, sound, look, how much? R Region/Radiation: Where is it and does it spread? +3 Full S Severity Scale: Rate on appropriate pain scale. Does it interfere with ADLs? +4 Bounding T Timing: When did it start? Sudden/gradual? How often? How long does it last? 231216216 5 P’s of Circulatory Checks Pain Pallor Paralysis Paresthesia Pulse AGE Preemie Term NB 6 Months 1 yr 3 yrs 5 yrs 6 yrs 8 yrs 12 yrs 16 yrs Adult Female Adult Male Averages for Age Grouping WGT (kg) PULSE RESP 1-2 140 < 60 3 125 < 60 7 120 24-36 10 120 22-30 15 110 20-26 18 100 20-24 20 100 20-24 25 90 18-22 40 85-90 16-22 > 50 75-80 14-20 50-75 60-100 12-20 75-100 60-100 12-20 B/P (syst.) 50-60 70 90 ± 30 96 ± 30 100 ± 25 100 ± 20 100 ± 15 105 ± 15 115 ± 20 120 ± 20 90 + age 100 + age Symptom Analysis: This assists the client in describing the problem. Provocate/Palliative: What caused it? What makes it better/worse? Quality/Quantity: How does it feel, sound, look, how much? Region/Radiation: Where is it and does it spread? Severity Scale: Rate on appropriate pain scale. Does it interfere with ADLs? Timing: When did it start? Sudden/gradual? How often? How long does it last? P Q R S T 4 Primary Assessment Techniques: INSPECT, PALPATE, PERCUSS, AUSCULATE What to Observe General appearance and behavior, mood, affect, posture, gait, hygiene, speech, mental status, height, weight, hearing and visual acuity, VS, nutritional status Head and Neck Skull size, shape, symmetry, hair & scalp, clenched jaws, puff cheeks, inspect teeth and gums, swallowing, PERRLA, inspect ROM neck, shrug shoulders, palpate trachea for symmetry, palpate carotid pulses Upper Extremities Inspect skin, cap refill, fingernails, palpate peripheral pulses, rate muscle strength, assess ROM Assessment Area General Survey Posterior Thorax Inspect spine for alignment, inspect skin especially at boney prominences, assess anteroposterior to lateral diameter, assess thoracic expansion, auscultate breath sounds Anterior Thorax Observe respirations. Effort, pattern, excursion, auscultate breath sounds, auscultate heart sounds, inspect jugular veins, Abdomen Inspect, auscultate for bowel sounds, light palpation for tenderness, palpate the kidneys, blunt percussion over CVA (posterior thorax) for tenderness Lower Extremities Inspect skin, palpate peripheral pulses, inspect and palpate joints for swelling, assess for pedal and ankle edema, assess ROM General Neurologic Inspect gait and balance, assess recent and remote memory, Assess alertness and orientation x 4 (person, place, time and situation), Glasgow Coma Scale Wound/Skin abnormality Documentation: 1. Location of the abnormality. Use your anatomical terms (lateral, medial, ventral, distal, etc… to olecranon process, ischium, patella, etc…) and each abnormality is addressed separately. 2. Surgical lines (approximated) length documented in cm. a. List the # of sutures or staples if present. b. Redness, Swelling, Warmth, Induration, Drainage. Be specific where. 3. Any open area. Length X width documented in cm. Depth in cm if applicable. a. Wound Bed: Color, Slough/Eschar, Drainage, Tunneling if present: Use percentages and clock face if appropriate. 4. Staging (if pressure) *cannot downstage a wound nor stage a wound that the wound bed cannot be seen. 5. Surrounding Skin: Redness, Swelling, Warmth, Induration, Drainage. Glasgow Coma Scale Eye Verbal Motor 231216216 1 Does not open eyes Makes no sounds Makes no movements 2 Opens eyes in response to painful stimuli Incomprehensible sounds 3 Opens eyes in response to voice Utters incoherent words 4 Opens eyes spontaneously Confused, disoriented Extension to painful stimuli (decerebrate response) Abnormal flexion to painful stimuli (decorticate response) Flexion / Withdrawal to painful stimuli 5 N/A 6 N/A Oriented, converses normally Localizes to painful stimuli N/A Obeys commands