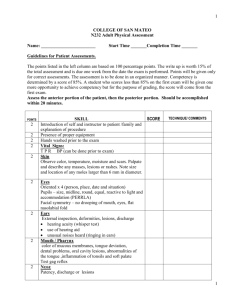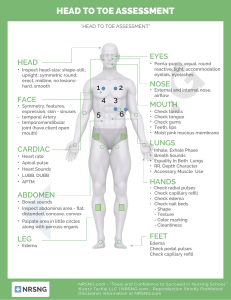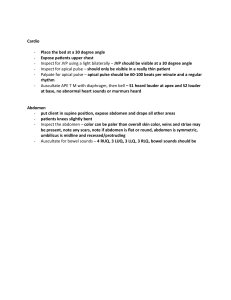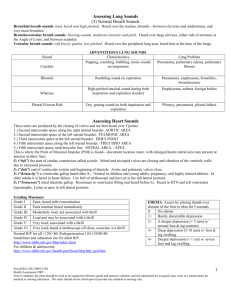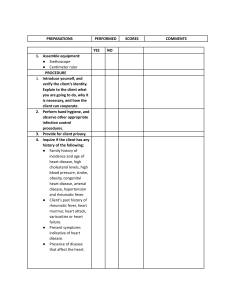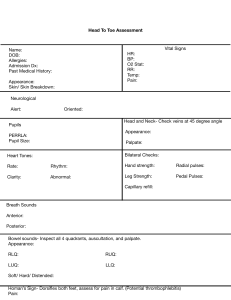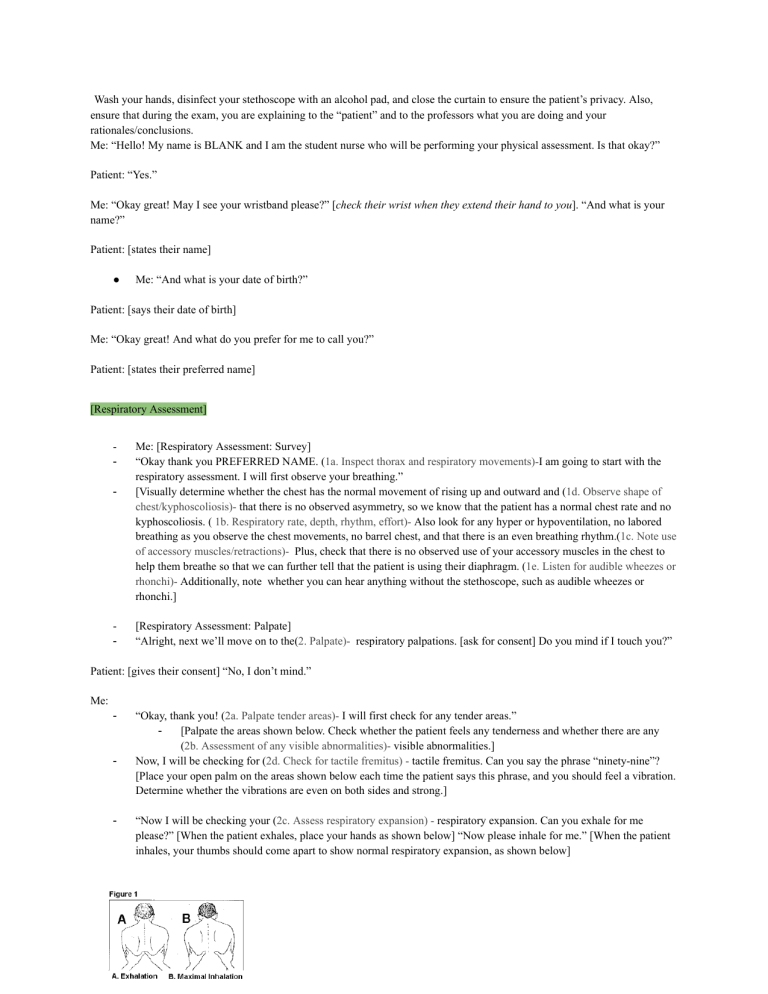
Wash your hands, disinfect your stethoscope with an alcohol pad, and close the curtain to ensure the patient’s privacy. Also, ensure that during the exam, you are explaining to the “patient” and to the professors what you are doing and your rationales/conclusions. Me: “Hello! My name is BLANK and I am the student nurse who will be performing your physical assessment. Is that okay?” Patient: “Yes.” Me: “Okay great! May I see your wristband please?” [check their wrist when they extend their hand to you]. “And what is your name?” Patient: [states their name] ● Me: “And what is your date of birth?” Patient: [says their date of birth] Me: “Okay great! And what do you prefer for me to call you?” Patient: [states their preferred name] [Respiratory Assessment] - - Me: [Respiratory Assessment: Survey] “Okay thank you PREFERRED NAME. (1a. Inspect thorax and respiratory movements)-I am going to start with the respiratory assessment. I will first observe your breathing.” [Visually determine whether the chest has the normal movement of rising up and outward and (1d. Observe shape of chest/kyphoscoliosis)- that there is no observed asymmetry, so we know that the patient has a normal chest rate and no kyphoscoliosis. ( 1b. Respiratory rate, depth, rhythm, effort)- Also look for any hyper or hypoventilation, no labored breathing as you observe the chest movements, no barrel chest, and that there is an even breathing rhythm.(1c. Note use of accessory muscles/retractions)- Plus, check that there is no observed use of your accessory muscles in the chest to help them breathe so that we can further tell that the patient is using their diaphragm. (1e. Listen for audible wheezes or rhonchi)- Additionally, note whether you can hear anything without the stethoscope, such as audible wheezes or rhonchi.] [Respiratory Assessment: Palpate] “Alright, next we’ll move on to the(2. Palpate)- respiratory palpations. [ask for consent] Do you mind if I touch you?” Patient: [gives their consent] “No, I don’t mind.” Me: - - - “Okay, thank you! (2a. Palpate tender areas)- I will first check for any tender areas.” [Palpate the areas shown below. Check whether the patient feels any tenderness and whether there are any (2b. Assessment of any visible abnormalities)- visible abnormalities.] Now, I will be checking for (2d. Check for tactile fremitus) - tactile fremitus. Can you say the phrase “ninety-nine”? [Place your open palm on the areas shown below each time the patient says this phrase, and you should feel a vibration. Determine whether the vibrations are even on both sides and strong.] “Now I will be checking your (2c. Assess respiratory expansion) - respiratory expansion. Can you exhale for me please?” [When the patient exhales, place your hands as shown below] “Now please inhale for me.” [When the patient inhales, your thumbs should come apart to show normal respiratory expansion, as shown below] Me: “Alright, next I will be performing (3/3a. Percuss all fields: dullness/hyperresonance)- respiratory percussions.” Or - [Percuss anteriorly and posteriorly at the points shown below. When percussing anteriorly, have the patient keep their arms at their sides, but when percussing posteriorly, ask the patient to cross their arms in front of them. Place the knuckle closest to the fingertip of the middle finger of the non-dominant hand on each place that is being percussed and use the tip of the middle finger of the dominant to strike the knuckle of the other hand to percuss as shown below. Use the stepladder pattern as shown in the picture below on the right because you are testing for symmetry on both sides of the lungs.] [A great video on percussions: https://www.youtube.com/watch?v=48nzLXnEHvg&t=96s] [A great list of what you are listening for and abnormalities: https://www.physio-pedia.com/Respiratory_Assessment-_Percussion] Me: Alright next, we will be listening to your chest sounds with the (4. Auscultate) -stethoscope. [Place your stethoscope over the areas below and observe the patient’s breathing sounds. Use this link to help https://www.os=osis.org/answers/auscultation] - (4c. i & ii Assess transmitted sounds: egophony and whispered pectoriloquy)- Assess Egophony and Whispered Pectoriloquy Listen to the same points used in the posterior auscultating picture shown above bUse this link https://www.you tube .com/watch?v=wb15Dex0EFI [Cardiovascular Assessment] - - (1a. BP both arms (obtain palp pressure first)- Take the BP (both arms?) ,link https://www.registered nurse rn.com/how-to-take-blood-pressure-manually-clinical-nursing-skills/ Obtain the palp pressure first: https://www.youtube.com/watch?time_continue=6&v=8eB48Nosykw&feature=emb_title (1b. Heart rate and rhythm) -Heart rate and rhythm Take the pulse for 30 seconds and look for a regular rhythm - 2. Palpate all peripheral pulses 3/3 scale (also, what did they mean by "3/3 scale"?))- Palpate all peripheral pulses 3/3 scale - - (Palpate carotid pulse)- Palpate carotid pulse Palpate both, but not at the same time (4. Evaluate for jvd)- Evaluate JVD (jugular vein distension) JVD looks like this, and either the patient has it or they don’t. Jvd is abnormal To assess whether the patient has it, have them tilt their head back and to the left, and if JVD is present, then it would be on the right side of the patient’s neck next song disregard Boulevard - (5. Identify pmi)- Identify PMI (Point of Maximal Impulse) The patient’s left side anteriorly, mid clavicle, fifth intercostal space (palpate each intercostal space to count to the fifth) The first 30 seconds of this video explains this process https://www.youtube.com/watch?v=hKYmbwKZRss - (6. Assess capillary refill)- Assess capillary refill Watch from the 2:30 mark to the 3 minute mark in this video https://www.youtube.com/watch?v=EwaDSZRH1LE - (7. Auscultate heart sounds at the aortic, pulmonic, erbs, tricuspid, and mitral areas. Note amplitude of s1, s2)Auscultate heart sounds at the aortic, pulmonic, erbs, tricuspid, and mitral areas. Note the amplitude of s1 and s2 (lub and dub, respectively) [Abdominal/Gastrointestinal Assessment] https://www.registerednursern.com/abdominal-assessment-nursing/ https://nurseslabs.com/ultimate-guide-to-head-to-toe-physical-assessment/ - (1a. Inspect: abdomen, skin, umbilicus, contour, pulsations, peristaltic waves) - Inspect: abdomen, skin, umbilicus, contour, pulsations, peristaltic waves: https://pressbooks.library.torontomu.ca/assessmentnursing/chapter/abdomen-inspection/ (1a. Inspect abdomen)- Inspect abdomen: “The abdomen should be symmetrical and the umbilicus should be midline. Note the location of any asymmetry. If you suspect asymmetry, you can ask the client to take a deep breath in and out; this can accentuate any asymmetry or potential bulges.” (1a. Inspect skin) - Inspect skin: “Skin colour varies based on a client’s racial background and should be lk.’consistent across the abdomen and the umbilicus. If you observe a discolouration (e.g., redness), describe it and the location. No swelling should be present and the skin should be intact; describe and note the location of any swelling or damaged skin (e.g., an open ulcer). Examine the umbilicus, which may become infected from a piercing. Note any scars, which may indicate past surgeries.” (1a. Inspect umbilicus)- Inspect umbilicus: “Inspect the for bulging, which can sometimes appear as an everted umbilicus. Normally, an umbilicus is inverted. Although an everted umbilicus can be normal, so always inquire if it is new. If you observe bulging, ask the client if they have noticed it, when it began, whether they know what it is, and ask about any associated pain. At the end of the overall inspection, you can gently palpate it to assess its consistency (soft or hard) and the presence of pain.” Inspect contour (the abdominal curve) The normal contour of the abdomen is typically flat or rounded. A concave contour (inward curve of the abdomen that looks sunken in) is concerning because it can be associated with dehydration and malnutrition, and sometimes with anorexia nervosa and cancer A distended abdomen is an enhanced outward contour. The outward contour of the abdomen is typically enhanced when a client has increased air, fluid, and/or content inside the intestines, or outside the intestines within the peritoneal cavity. Distension may be associated with constipation, bowel obstruction, or irritable bowel syndrome. Inspect pulsations: Generally noted in thin patients, but the aortic pulsation can be noted above the umbilicus Inspect peristaltic waves “Observe the profile view (side view) while standing on the client’s right side. Standing on this side will help you visualize any peristaltic movement, which will move away from you. These movements are the waves caused by the gastrointestinal tract (e.g., large intestine contractions). .,Peristalsis movement is usually not observable on the abdomen. You may see it in a client who is thin; otherwise, visible peristalsis is a cue that should act as a concern and can suggest an intestinal blockage.” (2. Auscultate bowel sounds and bruits)- Auscultate: Bowel sounds and bruits Bowel sounds: start in the RIGHT LOWER QUADRANT and go clockwise in all the 4 quadrants should hear 5 to 30 sounds per minute…if no, bowel sounds are noted listen for 5 full minutes Listen to each quadrant for 30 seconds and double the number of sounds that you hear so that you get the # of sounds/minute Documents as: normal, hyperactive, or hypoactive Bruits (USE THE BELL OF THE STETHOSCOPE) - Bruit sounds are abnormal and have a blowing, whooshing sounds in the areas shown below Auscultate using the stethoscope’s bell at the points shown below https://www.youtube.com/watch?v=1Xc7RYkz-CE&t=299s - (3. Percuss: tympany and dullness, liver borders)- Percuss: Tympany and dullness, liver borders Tympany and dullness Percuss several areas in each of the four quadrants to determine presence of tympany and dullness. Use a systematic pattern: begin in the lower right quadrant, proceed to the upper right quadrant, the upper left quadrant, and the lower left quadrant. Liver borders Percuss the liver to determine its size. Begin in the right midclavicular line below the level of the umbilicus. Percuss upward over tympanic areas until a dull percussion sound indicates the lower liver border. Then percuss downward at the right midclavicular line, beginning from an area of resonance and progressing downward until a dull percussion sound indicates the upper liver border. - (4. Palpate: lightly and assess for guarding, full bladder)- Palpate: lightly and assess for guarding, full bladder Palpate lightly: It is a gentle exploration performed while the client is in supine position. With the examiner’s hands parallel to the floor. The fingers depress the abdominal wall, at each quadrant, by approximately 1 cm without digging, but gently palpating with slow circular motion. This method is used for eliciting slight tenderness, large masses, and muscles, and muscle guarding. Tensing of abdominal musculature may occur because of: The client is ticklish or guards involuntarily, presence of subjacent pathologic condition. Normal findings: No tenderness noted. With smooth and consistent tension. No muscles guarding. Palpate full bladder: Gently palpate from the umbilicus downward toward the pelvis, feeling for a full bladder. Once you have found the bladder, continue to palpate outlining the bladder. You are noting the shape and contour of the bladder. An empty bladder is not palpable. A bladder is firm and non-tender. A bladder that is full is usually palpated at a higher level on the abdomen. A full bladder will feel firm. https://www.nurseslearning.com/courses/nrp/NRP-1616/Section2/index.htm https://thoracickey.com/conduct-and-interpretation-of-the-basic-chest-exam/ air, fluid, and/or content inside the intestines, or outside the intestines within the peritoneal cavity