IT 111205 WAO frew
advertisement

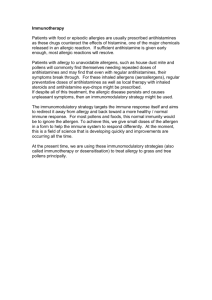
Subcutaneous Immunotherapy: clinical aspects Anthony J Frew MD FRCP Professor of Allergy & Respiratory Medicine, Royal Sussex County Hospital, Brighton BN2 5BE UK Introduction Specific allergen immunotherapy (SIT) involves administration of allergen extracts to patients with allergic conditions in order to modify or abolish their symptoms. SIT is specific, in that it targets those allergens identified by the patient and physician as responsible for symptoms, but does not affect sensitivity to unrelated allergens. While the precise mechanisms involved remain uncertain, there is a substantial body of clinical evidence and practice to support the use of SIT. Before deciding to use SIT, the patient’s condition needs to be carefully assessed, with particular regard to allergic triggers. In addition, since the course of treatment is lengthy and relatively expensive, there must also be an assessment of the risks and costs as compared to symptomatic treatment with antihistamines and topical corticosteroids. Immunotherapy was first developed at St Mary's Hospital London 100 years ago [1] and many of the basic principles described by Noon and Freeman remain valid today. In standard subcutaneous immunotherapy (SCIT), patients receive a course of injections, starting with a very low dose of allergen, and building up gradually until a plateau or maintenance dose is achieved. Maintenance injections are then given at 46 weekly intervals, usually for 3 years. The updosing phase is usually given as a series of weekly injections, but several alternative induction regimes have been tried, some giving several doses on each day then waiting a week before giving a further series of injections (cluster protocol), while others give the whole series of incremental injections in a single day (rush protocol). Mechanisms of immunotherapy Several mechanisms have been proposed to explain the beneficial effects of immunotherapy. Whether given by injection or sublingually, SIT induces changes in Tcell and antibody responses. The challenge for clinical scientists has been to work out which of the observed changes drive the clinical benefit, and which are just epiphenomena. Allergen-specific IgE levels rise temporarily during the initial phase of SIT, but fall back to pre-treatment levels during maintenance therapy [2]. The immediate weal and flare response to skin testing usually reduces during the initial phases of SIT but this effect is relatively small compared to the degree of clinical benefit. In contrast, the late-phase response to skin testing is virtually abolished after successful SIT. Similar patterns are observed for late-phase responses in the nose and airways [3]. SIT also induces allergen-specific IgG antibodies, particularly antibodies of the IgG4 subclass. In most studies IgG correlates better with the dose of allergen that has been given, rather than with the degree of protection achieved. There has been a recent resurgence of interest in a possible inhibitory role of specific IgG antibodies in grass pollen immunotherapy [4], in particular, the timecourse of this effect raises the possibility of sIgG antibodies interfering with IgE-dependent cytokine secretion from mast cells or facilitated antigen presentation to T cells. 1 In nasal and skin allergen challenge models, successful SIT is accompanied by a reduction in T-cell and eosinophil recruitment in response to allergen. In parallel, there is a shift in the balance of Th1 and Th2 cytokine expression in the allergenchallenged site. Th2 cytokine expression is not affected but there is an increased proportion of T-cells expressing the Th1 cytokines IL-2, IFN- and IL-12 [5-7]. After venom SIT, there is induction of allergen-specific CD4+ T-regulatory cells which express CD25, Fox p3 and IL-10, as well as a shift in Th1:Th2 balance [8,9]. Similar findings have also been reported following SIT with inhalant allergens [10]. IL-10 has several relevant actions, including downregulation of T-cells and induction of allergen-specific IgG4 antibodies, which may explain the IgG4 response to SIT. The IgG4 response should probably be viewed as a surrogate marker of IL-10 induction, rather than the beneficial mechanism of SIT [11]. Overall, it is clear that SIT has a modulatory effect on allergen-specific T-cells, and this is probably why clinical and late-phase responses are attenuated without suppressing allergen-specific antibody levels or immediate allergic responses. CLINICAL INDICATIONS SIT for venom hypersensitivity Anaphylaxis to hymenoptera venom is relatively rare, but can be fatal. Precise figures are hard to come by, but a figure of at least 40 deaths per year in the USA has been cited. Venom immunotherapy can reduce the risk of fatality and improve the patient’s quality of life by allowing them to go out and work or play without worrying about the possibility of a serious allergic reaction. Given the relatively small number of fatalities, the main impact of VIT is on people’s quality of life. After completing VIT, there is a residual risk of systemic reactions of approximately 10%, but when reactions do occur to stings after VIT, they are typically mild. Patients who receive VIT should be supplied with anti-allergic medication for use in the event of a sting during or after therapy. Some allergists recommend providing injectable epinephrine during therapy, but this is not necessary once the patient has reached the maintenance dose of SIT. SIT for allergic rhinitis SIT is a useful treatment for allergic rhinitis, especially when the range of allergens responsible is narrow. The allergic basis of the rhinitis should be carefully assessed both on history and on skin tests or blood tests, and other causes of nasal symptoms should be excluded. In patients with persistent non-seasonal rhinitis, it can be extremely difficult to determine whether the patient’s symptoms are truly due to allergy, or whether they have non-allergic rhinitis, and just happen to be sensitised to an allergen that is not clinically relevant. This difficulty in determining clinical relevance contributes to the reported lower degree of efficacy in SIT trials with perennial allergens, as compared to SIT for seasonal allergies. The effectiveness of SIT in intermittent (seasonal) allergic rhinitis has been confirmed in many trials, using grass, ragweed and birch pollen extracts [12]. Importantly, SIT is effective even in patients whose severe seasonal rhinitis is resistant to conventional drug therapy [13]. Importantly, patients with multiple allergic sensitisation respond at least as well as those who were monosensitised to grass pollen. 2 The benefits of one year’s treatment wear off quickly [14], but three years therapy gives lasting benefit [15]. Less well controlled data show that the effects of SIT can persist for many years after discontinuing therapy [16]. This contrasts with conventional drugs, whose effects wear off very soon after discontinuing therapy. The benefits of SIT for perennial rhinitis are less than for seasonal rhinitis, but clinical trials have shown a definite benefit in appropriately selected subjects. SIT for asthma Immunotherapy has been widely used to treat allergic asthma, although the introduction of effective inhaled therapies has changed the general pattern of asthma care. Concern over adverse reactions, including a small number of fatalities, has led some countries (e.g. UK) to restrict the use of SIT for asthma treatment, although asthma remains a common indication for SIT in many parts of North America and continental Europe [17,18]. Current drug therapies for asthma aim to suppress airways inflammation and relieve bronchospasm. None of these treatments are curative and asthma recurs rapidly on ceasing treatment. However, SIT remains controversial as a treatment for asthma because of its potential for adverse effects. The efficacy of SIT in adult asthma has been assessed in many trials over the last 65 years. The results of these studies have often been difficult to interpret, either because poor quality allergen extracts were used or because of poor study design. The main drawback in using SIT to treat asthma is the risk of serious adverse reactions. The vast majority of fatal reactions to SIT have occurred in patients with asthma, and while asthma is not an absolute contraindication, it is clear that patients with unstable asthma should not be offered SIT, and caution should be exercised in anyone with an increased level of asthma symptoms or transiently reduced peak flow rates. Effects on natural history of allergic disease Children often start with a limited range of allergic sensitivities and progress over time to develop IgE against a wider range of inhaled allergens. Treatment with SIT may limit this tendency to acquire new sensitisations [19] although the clinical benefit of this preventive effect is not clear. A proportion of patients with allergic rhinitis develop asthma each year. This annual rate of progression has been estimated at 5% in college students [20] but this is perhaps surprisingly an area of considerable ignorance. SIT may modify the natural history of asthma in children who are known to be atopic but have not yet developed asthma. Only limited data is available to support this proposition. In the key study, a group of 205 children aged 6-14, without previously diagnosed asthma, were treated with SIT for birch or grass pollen allergy in an open randomised design. Three years after completing treatment 45% of the untreated group had developed asthma while only 26% of the treated group had asthma. These results have been sustained out to seven years after completing therapy [21]. SIT may also modify the progression of established asthma. An early open study using uncharacterised mixed allergen extracts supported this view, with about 70% of treated children losing their asthma after four years therapy, compared to about 19% of untreated controls, a result which was sustained up to the age of 16 years [22]. In contrast, there is no current evidence that SIT influences the evolution of established 3 asthma in adults. Safety of SIT The most obvious risk of SIT is provocation of systemic allergic reactions. In the UK twenty-six fatal reactions due to SIT were reported between 1957 and 1986 [23]. In almost all cases these patients were receiving SIT to treat their asthma. Similarly, in the AAAAI inquiry into SIT-associated deaths, asthma appeared to be the cause of death in most of the fatal cases [24,25]. The incidence of systemic reactions in patients receiving SIT for asthma has been reported to range from 5% to 35%. Separately, there is some concern about the use of immunomodulatory treatments in patients with autoimmune disorders, immunodeficiency syndromes or malignant disease. While there is no hard evidence that SIT is actually harmful to these patients, some clinicians feel uncomfortable about manipulating the immune system in such patients, not least because of the risk that spontaneous and unrelated variations in the autoimmune disorder or cancer may be blamed on SIT. Future directions There is scope to improve conventional SIT. Possible avenues include the use of recombinant allergens, various forms of allergenic molecules folding variants and other modifications of the physical structure which may also improve the safety of SIT [26]. Since the epitopes recognised by IgE molecules are usually threedimensional whereas T-cell epitopes are short linear peptide fragments of the antigen, it should be possible to use peptide fragments of allergens to modulate T cells without risking anaphylaxis. Alternatively, DNA vaccines may be used, either by a general approach, using CpG oligodeoxynucleotides which mimic bacterial DNA, and stimulate Th1-type cytokine responses, or a more specific approach using allergen-specific naked DNA sequences as vaccines. Conclusions SCIT has been used for over a century, and is clinically effective in patients with rhinitis or asthma whose symptoms are clearly driven by allergic triggers. Although we are still unsure exactly how SIT works, it induces regulatory T cells that damp the response to allergen exposure in sensitised subjects. When used in appropriately selected patients, SCIT is effective and safe, but care is needed to recognise and treat adverse reactions. Future directions in SIT will include the development of better standardised vaccines, and the use of recombinant allergens, both of which should improve the safety profile of SIT. References 1. Freeman J. Vaccination against hay fever: report of results during the first three years. Lancet 1914; 1:1178. 2. Creticos PS, Van Metre TE, Mardiney MR, Rosenberg GL, Norman PS, Adkinson NF . Dose-response of IgE and IgG antibodies during ragweed immunotherapy. J.Allergy Clin.Immunol. 1984; 73:94-104. 3. Iliopoulos O, Proud D, Adkinson NF, Creticos PS, Norman PS, Kagey-Sobotka A, Lichtenstein LM, Naclerio RM. Effects of immunotherapy on the early, late and rechallenge nasal reaction to provocation with allergen: changes in 4 inflammatory mediators and cells. J.Allergy Clin.Immunol. 1991; 87:855-866. 4. Francis J, James L, Paraskevopoulos G et al. Grass pollen immunotherapy: IL-10 induction and suppression of late responses precedes IgG4 inhibitory antibody activity. J Allergy Clin Immunol 2008; 121:1120-1125 5. Durham SR, Ying S, Varney VA, Jacobson MR, Sudderick RM, Mackay IS, Kay AB, Hamid QA. Grass pollen immunotherapy inhibits allergen-induced infiltration of CD4+ T-lymphocytes and eosinophils in the nasal mucosa and increases the number of cells expressing mRNA for interferon-gamma. J.Allergy Clin.Immunol. 1996;97:1356-65. 6. McHugh SM, Deighton J, Stewart AG, Lachmann PJ, Ewan PW. Bee venom immunotherapy induces a shift in cytokine responses from a Th2 to a Th1 dominant pattern: comparison of rush and conventional immunotherapy. Clin.Exp.Allergy 1995; 25:828-38. 7. Ebner C, Siemann U, Bohle B, Willheim M, Wiedermann U, Schenk S, Klotz F, Ebner H, Kraft D, Scheiner O. Immunological changes during specific immunotherapy of grass pollen allergy: reduced lymphoproliferative responses to allergen and shift from Th2 to Th1 in T-cell clones specific for Phl p1, a major grass pollen allergen. Clin.Exp.Allergy 1997; 27:1007-15. 8. Jutel M, Akdis M, Blaser K, Akdis CA. Mechanisms of allergen specific immunotherapy--T-cell tolerance and more. Allergy 2006; 61:796-807. 9. Nasser SM, Ying S, Meng Q, Kay AB, Ewan PW. IL-10 levels increase in cutaneous biopsies of patients undergoing wasp venom immunotherapy. Eur.J.Immunol. 2001;31:3704-13. 10. Akdis CA, Blesken T, Akdis M, Wuthrich B, Blaser K. Role of IL-10 in specific immunotherapy. J.Clin.Invest. 1998;102:98-106. 11. Bellinghausen I, Knop J, Saloga J. The role of IL-10 in the regulation of allergic immune responses. Int.Arch.Allergy Appl.Immunol. 2001;126:97-101. 12. Calderon MA, Alves B, Jacobson M, Hurwitz B, Sheikh A, Durham S. Allergen injection immunotherapy for seasonal allergic rhinitis. Cochrane Database Syst Rev. 2007 Jan 24;(1):CD001936. 13. Frew AJ, Powell RM, Corrigan CJ, Durham SR. Efficacy and safety of specific immunotherapy with SQ allergen extract in treatment-resistant seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006; 117:319-25. 14. Naclerio RM, Proud D, Moylan B, Balcer S, Freidhoff L, Kagey-Sobotka A, Lichtenstein LM, Creticos PS, Hamilton RG, Norman PS. A double blind study of the discontinuation of ragweed immunotherapy. J Allergy Clin Immunol 1997;100:293-300. 15. Durham SR, Walker SM, Varga EM, Jacobson MR, O'Brien F, Nobel W, Till SJ, Hamid QA, Nouri-Aria K. Long-term clinical efficacy of grass pollen immunotherapy. N.Engl.J.Med. 1999;341:468-75. 16. Eng PA et al . 12 year follow-up after discontinuation of preseasonal grass pollen immunotherapy in childhood. Allergy 2006; 61:198-201. 17. Bousquet J, Lockey RF, Malling HJ. WHO position paper. Allergen immunotherapy: therapeutic vaccines for allergic disease. Allergy 1998;53(S44):1-42. 18. Abramson M, Puy R, Weiner J. Immunotherapy in asthma: an updated systematic review. Allergy 1999;54:1022-41. 19. Des Roches A, Paradis L, Menardo JL, Bouges S, Daures JP, Bousquet J. 5 Immunotherapy with a standardised Dermatophagoides pteronyssinus extract. VI. Specific immunotherapy prevents the onset of new sensitisations in children. J.Allergy Clin.Immunol. 1997;99:450-3. 20. Horak F. Manifestation of allergic rhinitis in latent sensitised patients. A prospective study. Arch. Otorhinolaryngol. 1985; 242:242-249. 21. Niggemann B, Jacobsen L, Dreborg S, Ferdousi HA, Halken S, Host A et al. Fiveyear follow-up on the PAT study: specific immunotherapy and long-term prevention of asthma in children. Allergy 2006; 61:855-9. 22. Johnstone DE, Dutton A. The value of hyposensitization therapy for bronchial asthma in children. A 14 year study. Pediatrics 1968; 42:793-. 23. Committee on the Safety of Medicines. CSM update: immunotherapy. Br.Med.J. 1986; 293:948. 24 Stewart GE, Lockey RF. Systemic reactions from allergen immunotherapy. J.Allergy Clin.Immunol. 1992; 90:567-578. 25 Bernstein DI, Wanner M, Borish L, Liss GM. Twelve-year survey of fatal reactions to allergen injections and skin testing: 1990-2001. J Allergy Clin Immunol 2004:113:1129-36 26 Purohit A, Niederberger V, Kronqvist M et al. Clinical effects of immunotherapy with genetically modified recombinant birch pollen Bet v1 derivatives. Clin.Exp.Allergy 2008; 38:1514-25 6