Standard Infection Control Precautions Policy
advertisement

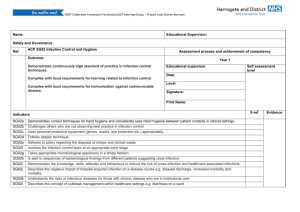
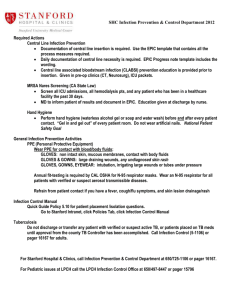
Standard (Infection Control) Precautions Policy Version 5 Name of responsible (ratifying) committee Infection Prevention Management Committee Date ratified 13 May 2015 Document Manager (job title) Infection Prevention Management Committee Date issued 07 August 2015 Review date 06 August 2017 Electronic location Infection Control Policies Related Procedural Documents Infection Control Policies / Occupational Health Key Words (to aid with searching) Risk Assessment; Standard Precautions; Universal precautions potentially contaminated; HIV infections; Staff; Visitor; Patient; Locum; Personal protection equipment; (PPE): Risk assessment; Body fluids; Occupational health and safety; Gloves; Aprons; Clinical waste; Training; Infection control; Waste disposal; Clinical guidelines; blood borne viruses Version Tracking Version Date Ratified 5 13/05/2015 Brief Summary of Changes Author Update to standard infection control precautions to include decontamination of medical devices, cough and respiratory hygiene IPCT Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 1 of 16 CONTENTS 1. INTRODUCTION ......................................................................................................................... 4 2. PURPOSE ................................................................................................................................... 4 3. SCOPE ........................................................................................................................................ 4 4. DEFINITIONS .............................................................................................................................. 4 5. DUTIES AND RESPONSIBILITIES .............................................................................................. 4 6. PROCESS ................................................................................................................................... 5 7. TRAINING REQUIREMENTS .................................................................................................... 14 8. REFERENCES AND ASSOCIATED DOCUMENTATION .......................................................... 15 9. EQUALITY IMPACT STATEMENT ............................................................................................ 15 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS ........................................ 16 Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 2 of 16 QUICK REFERENCE GUIDE 1. Standard Infection Control Precautions are the basic infection prevention and control measures necessary to reduce the risk of transmission of infectious agents from both recognised and unrecognised sources of infection. 2. Standard Infection Control Precautions are to be used by all staff, in all care settings, at all times, for all patients whether infection is known to be present or not. 3. The main elements of SICP’s are: Hand Hygiene – refer to Hand Hygiene Policy Personal Protective Equipment & Risk Assessment Respiratory and Cough Hygiene Occupational Safety: Prevention and Exposure Management including Sharps - refer to NSI and contamination incidents policy Management of blood and body fluid spillage Safe use of Medical Devices (inc. Decontamination) - refer to Decontamination policy Aseptic technique – refer to Asepsis policy Management of Linen – refer to Linen Handling and Laundry policy Management of Healthcare Waste – refer to Waste Handling policy 4. The type of PPE worn is based on the assessed risk of the clinical intervention to be undertaken. 5. All PPE should be: single-use only items unless specified by the manufacturer single patient use (only be used for one patient episode) donned and removed in an order that minimises the potential for cross-contamination Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 3 of 16 1. INTRODUCTION Standard Infection Control Precautions (SICP) (previously known as Universal Precautions) are the basic infection prevention and control measures necessary to reduce the risk of transmission of infectious agents from both recognised and unrecognised sources of infection. Sources of (potential) infection include blood and other body fluids secretions or excretions (excluding sweat), non-intact skin or mucous membranes and any equipment or items in the care environment that could have become contaminated. 2. PURPOSE The purpose of this policy is to provide guidance for staff within Portsmouth Hospitals NHS Trust about the requirements and processes for implementing Standard Infection Control Precautions. 3. SCOPE Standard Infection Control Precautions are to be used by all staff, in all care settings, at all times, for all patients whether infection is known to be present or not to ensure the safety of those being cared for, staff and visitors in the care environment. This Policy applies to all staff employed by Portsmouth Hospitals NHS Trust (the Trust) or Carillion, and also to all visiting staff including staff from external agencies (e.g. CCG or other Trusts), tutors, students, agency/locum staff and contractors. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Standard Infection Control Precautions (SICP) (previously known as Universal Precautions) are the basic infection prevention and control measures necessary to reduce the risk of transmission of infectious agents from both recognised and unrecognised sources of infection. 5. DUTIES AND RESPONSIBILITIES Chief Executive Ensure that infection prevention and control is a core part of clinical governance and patient safety programmes Promote compliance with infection prevention and control policies in order to reduce health care associated infections Awareness of legal responsibilities to identify, assess and control risk of infection Director of Infection Prevention Control (DIPC) Oversee infection prevention and control policies and their implementation Responsible for infection prevention and control team Report directly to the Chief Executive and Trust Board Challenge inappropriate hygiene and infection prevention and control practice Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 4 of 16 Infection Prevention Team: Review and update he Standard Infection Control Precautions policy Give additional advice regarding SICP’s and risk assessments Include SICP’s in all induction and update training for clinical staff Promote good practice and challenge poor practice Conduct audit and inspection of SICP with feedback to clinical staff Matrons / Ward Managers: Must establish a cleanliness culture across their units and promote compliance with infection prevention guidelines, including SICP Promote good practice and challenge poor practice All Healthcare Staff: Must be familiar with and adhere to the relevant infection prevention policies to reduce the risk of cross infection of patients Must adhere to the full terms and conditions of SICP’s documented in this policy Must use the risk assessment process to identify the appropriate level of SICP for each situation Promote good practice and challenge poor practice Refer to the infection prevention team if unable to follow the policy guidelines 6. PROCESS 6.1 To be effective in protecting against infection risks, SICPs must be used continuously by all staff. The application of SICPs during care delivery is determined by an assessment of risk to and from individuals and includes: the task; level of interaction; and/or the anticipated level of exposure to blood and/or other body fluids. The main elements of SICP’s are: Hand Hygiene – refer to Hand Hygiene Policy Personal Protective Equipment & Risk Assessment Respiratory and Cough Hygiene Occupational Safety: Prevention and Exposure Management including Sharps - refer to NSI and contamination incidents policy Management of blood and body fluid spillage Safe use of Medical Devices (inc. Decontamination) - refer to Decontamination policy Aseptic technique – refer to Asepsis policy Management of Linen – refer to Linen Handling and Laundry policy Management of Healthcare Waste – refer to Waste Handling policy Last Offices – refer to When an Adult Dies Policy 6.2 HAND HYGIENE The decontamination of hands is shown to significantly reduce the carriage of potential pathogens and decrease the risk and occurrence of Healthcare Associated Infections. Hands must be decontaminated when visibly dirty / contaminated, at the 5 key moments and immediately after the removal of gloves: Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 5 of 16 All staff must be ‘naked below the elbow’ before entering a clinical area and for the duration of their work. The two main products for hand decontamination are: alcohol-based hand rub for clean hands, or liquid soap and water for visibly dirty hands or when caring for patients with vomiting or diarrhoeal illness. All clinical staff must use a seven-step technique to systematically decontaminate hands and aseptic hand hygiene must be performed prior to invasive procedures e.g. central line insertion, dressing etc. Staff should follow recommended hand hygiene techniques to prevent damage or cracking to hands and regularly use emollient hand cream to maintain skin patency when hands are at rest. All clinical staff are responsible for completing, and remaining up to date with annual hand hygiene training. Refer to the Hand Hygiene Policy. 6.3 PERSONAL PROTECTIVE EQUIPMENT & RISK ASSESSMENT. Personal Protective Equipment (PPE) is additional to normal clothing and uniforms and is used to protect both the patient and health care worker from the risk of cross infection. PPE should be available for all staff and may include aprons and fluid repellent gowns/suits, gloves (sterile and non-sterile latex free), masks and eye protection (goggles and face visors). Before undertaking any procedure staff should assess any likely exposure and ensure PPE is worn that provides adequate protection against the risks associated with the procedure or task being undertaken. All PPE should be: located close to the point of use stored to prevent contamination in a clean/dry area until required for use (expiry dates must be adhered to) single-use only items unless specified by the manufacturer disposed of after use into the correct waste stream i.e. offensive or infectious waste. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 6 of 16 Gloves must be: Worn when exposure to blood and/or other body fluids is anticipated/likely Changed immediately after each patient and/or following completion of a procedure or task on the same patient Changed if a perforation or puncture is suspected Well-fitting to avoid excessive sweating and interference with dexterity (sized sterile gloves may be used for clinical procedures if required). Gloves are not impervious to infection but reduce penetration of blood and body fluids on to the hands Gloves should not be worn unnecessarily as their prolonged and indiscriminate use may cause adverse reactions and skin sensitivity. The gloves themselves also become a source of infection/contamination Gloves should be non-powdered and not made of latex Gloves should not be washed or sanitised with alcohol gel Gloves are not a replacement for hand hygiene Sized sterile gloves should be available and used for all aseptic procedures. Double gloving is recommended during some Exposure Prone Procedures (EPPs) or when attending major trauma incidents. Aprons must be: Worn to protect uniform or clothes when contamination is anticipated/likely e.g. when in direct care contact with a patient Changed between patients and/or following completion of a procedure or task. Staff are to wear a YELLOW (or colour coded) apron when caring for infectious patients nursed in isolation or with transmission precautions. Full body gowns/Fluid repellent coveralls must be: Worn where there is a risk of extensive splashing of blood, body fluids, secretions and excretions, with the exceptions of sweat, onto the skin of health care workers. These may be sterile or non-sterile in nature depending on the intended use Changed between patients and/or following completion of a procedure or task. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 7 of 16 Eye/face protection (including full face visors) must be: Worn if blood and/or body fluid contamination to the eyes/face is anticipated/likely. If reusable equipment is used it should be decontaminated appropriately (refer to the Decontamination policy) Single use / single patient use items should be disposed of immediately Goggles and visors should fit the wearer well Hands should be washed with soap and water on removal. Fluid repellent surgical face masks must be: Worn if splashing or spraying of blood, body fluids, secretions or excretions onto the respiratory mucosa (nose and mouth) is anticipated/likely e.g. for influenza cases, bacterial meningitis, diphtheria Worn to help prevent particles being expelled into the environment or onto the sterile field by the wearer in order protect patients from the operator as a source of infection e.g. during surgery Well fitting and fit for purpose (fully covering the mouth and nose) (recognizing that such masks are not necessarily designed for filtration efficiency, or to seal tightly to the face) Be handled as little as possible and changed between patients or operations. Removed or changed; at the end of a procedure/task; if the integrity of the mask is breached, e.g. from moisture build-up after extended use or from gross contamination with blood or body fluids; and in accordance with specific manufacturers instructions (including disposal). Respirator FFP3 masks must be: Worn to provide protection from exposure to airborne particles Made to defined national European standard EN149:2001+A1:2009 FFP3 respirator Fit tested to ensure that an adequate seal is achievable Worn correctly to seal firmly to the face, thus reducing the risk of leakage Only be used when clinically indicated and should be disposed of by the wearer on leaving the infected environment. Indications include airborne respiratory pathogens e.g. Open Pulmonary Tuberculosis, where high level protection is needed e.g. Viral Haemorrhagic Fevers or during potentially infectious Aerosol Generating Procedures in patients with specific pathogens e.g. influenza, SARS Aerosol Generating Procedures are defined as: Intubation, extubation and related procedures, e.g. manual ventilation/open suctioning Cardiopulmonary resuscitation Bronchoscopy Surgery and post mortem procedures in which high-speed devices are used Non Invasive Ventilation (NIV) e.g. Bilevel Positive Airway Pressure Ventilation (BiPAP) and Continuous Positive Airway Pressure Ventilation (CPAP) High Frequency Oscillatory Ventilation (HFOV) Induction of sputum. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 8 of 16 Removal of Personal Protective Equipment must be: Performed in an order that minimises the potential for cross-contamination. On completion of a task/procedure, gloves, gown and eye goggles should be removed (in that order) and disposed of as clinical waste. If wearing a mask, this should be removed last, to minimise contamination of the face. 1. Gloves Grasp the outside of the glove with the opposite gloved hand; peel off Hold the removed glove in gloved hand Slide the fingers of the ungloved hand under the remaining glove at the wrist Peel the second glove off over the first glove and discard 2. Gown or apron Unfasten or break ties Pull gown/apron away from the neck and shoulders, touching the inside of the gown only Turn the gown/apron inside out, fold or roll into a bundle and discard 3. Goggles or face shield To remove, handle by the headband or earpieces and discard 4. Respirator or surgical mask Untie or break bottom ties, followed by top ties or elastic and remove by handling ties only and discard directly into an infectious waste bin. To minimise cross-contamination, the order outlined above should be applied even if not all items of PPE have been used. On completion hand hygiene should be undertaken. 6.4 RESPIRATORY AND COUGH HYGIENE Correct respiratory hygiene and cough etiquette is effective in decreasing the risk of transmission of pathogens contained in large respiratory droplets e.g. influenza virus. Cover the nose and mouth with a disposable tissue when sneezing, coughing, wiping and blowing the nose Dispose of all used disposable tissues promptly into a waste bin Wash hands with non-antimicrobial liquid soap and warm water after coughing, sneezing, using tissues, or after contact with respiratory secretions or objects contaminated by these secretions Keep contaminated hands away from the eyes nose and mouth. Staff should promote respiratory and cough hygiene helping those (e.g. elderly, children) who need assistance with this e.g. providing patients with tissues and hand hygiene facilities. It may be appropriate for some respiratory pathogens (e.g. influenza) for patients to wear a standard surgical face mask in the presence of others to prevent droplet transmission through coughing. 6.5 OCCUPATIONAL SAFETY: PREVENTION AND EXPOSURE MANAGEMENT INCLUDING SHARPS A significant occupational exposure is: a percutaneous injury e.g. injuries from needles, instruments, bone fragments, or bites which break the skin; and/or exposure of broken skin (abrasions, cuts, eczema, etc); and/or Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 9 of 16 exposure of mucous membranes including the eye from splashing of blood or other high-risk body fluids. The majority of inoculation injuries involve sharps. All contaminated sharps carry a risk of injury and blood borne infection. Extreme care should be taken when handling all sharp objects. Where possible the sharps provided by the Trust will have a safety mechanism built into their design. The safety mechanism must be used to prevent the risk of inoculation injuries. The emphasis on preventing contaminated inoculation injury must focus on ensuring safe handling practices are in place. Staff must: Use appropriate PPE Used closed vacuum blood collection systems for blood collection or cultures Always discard used sharps into a sharps container at the point of use Ensure that needles are not re-sheathed, Use a clean plastic tray to carry sharps; never carry loose sharps in your hands Ensure that sharps containers are not filled above the mark indicating they are full Use temporary closure mechanisms when sharps boxes are not in use Locate sharps containers in safe positions, e.g. secured to a wall Not work alone using sharps with confused or disoriented patients Report all incidents (including near misses) involving contaminated sharps at the time of occurrence, or as soon as possible afterwards, to Occupational Health. Refer to Sharps Policy (NSI and contamination incidents policy) 6.6 SAFE MANAGEMENT OF BLOOD AND BODY FLUID SPILLAGES Spillages of blood and other body fluids may transmit blood borne viruses. Spillages must be decontaminated immediately by clinical staff trained to undertake this safely to prevent further contamination and protect staff and patients. Follow the spillage algorithm. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 10 of 16 Blood and/or body fluid spillage Adapted from Health Protection Scotland National Infection Prevention and Control Manual. Wear appropriate PPE e.g. non-sterile disposable gloves/apron +/- face/eye protection Is the spillage on soft furnishing e.g. fabric seats, carpets? Is it a spill of blood or body fluid as specified in Box 1? Place disposable paper towels over spillage to absorb and contain it applying solution of 10,000 parts per million available chlorine (Actichlor Plus® 10 x 1.7g tablet in one litre of cold water) to the towels Leave for 3-5 minutes Discard the gross contamination into a healthcare waste bag Spill contains ONLY urine/faeces/vomit/sputum Do NOT use a chlorine releasing agent directly on a urine spill Soak up spillage/gross contamination using disposable paper towels Decontaminate area with a solution of 1,000 parts per million available chlorine (Actichlor Plus® 1 x 1.7g tablet in one litre of cold water) to the towels Leave for 3-5 minutes Discard the gross contamination into a healthcare waste bag Allow area to air dry Dispose of PPE into a healthcare waste bag Perform hand hygiene Box 1 Cerebrospinal fluid Peritoneal fluid Pleural fluid Synovial fluid Amniotic fluid Semen Vaginal secretions Any other body fluid with visible blood (excluding urine) Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Discuss with IPCT and consider If furnishing is heavily contaminated it may need to be discarded If furnishing can withstand chlorine, follow the appropriate spills pathway If it is safe to clean with detergent alone then follow appropriate procedure Consider steam cleaning / external decontamination Page 11 of 16 6.7 SAFE USE OF MEDICAL DEVICES (INCLUDING DECONTAMINATION) Medical devices and equipment may become easily contaminated with blood, other body fluids, secretions, excretions and infectious agents. Consequently it is easy to transfer infectious agents from communal care equipment during care delivery. Medical devices and equipment are classified as either: Single Use: equipment which is used once on a single patient and then discarded. This equipment must never be reused even on the same patient. The packaging carries this symbol. Needles and syringes are single use devices. They should never be used for more than one patient or reused to draw up additional medication Never administer medications from a single-dose vial or intravenous (IV) bag to multiple patients. Single Patient Use: equipment which can be reused on the same patient Reusable Invasive Equipment - used once then decontaminated e.g. surgical instruments. Reusable non-invasive equipment (often referred to as communal equipment) reused on more than one patient following decontamination between each use e.g. commode, patient transfer trolley. Before using any sterile equipment check that: the packaging is intact there are no obvious signs of packaging contamination the expiry date remains valid. Decontamination of reusable non-invasive care equipment must be undertaken: between each use after blood and/or body fluid contamination at regular predefined intervals as part of an equipment cleaning protocol before inspection, servicing or repair. Adhere to manufacturers’ guidance for use and decontamination of all care equipment. Refer to the Decontamination policy or NHS Cleaning manual for specific cleaning instructions. 6.8 ASEPTIC TECHNIQUE Refer to Asepsis policy 6.9 MANAGEMENT OF LINEN Used linen is a potential source of infection as it is likely to be contaminated with potentially pathogenic organisms. Gloves and aprons must be worn when dealing with soiled, wet or blood stained linen Linen should be bagged by the bedside, never carried through a clinical area by hand Linen bags must be 2/3 filled only. They must not be overfilled Linen from infected patients or blood stained must be placed in an inner red alginate bag, and then placed into an outer white plastic bag When removing soiled linen avoid the production of aerosols If patient’s clothing is being laundered at home, place soiled laundry in a clear plastic bag inside an outer patient’s property bag. Inform visitors that laundry is awaiting collection in the patient locker. Refer to Linen Handling and Laundry policy Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 12 of 16 6.10 MANAGEMENT OF HEALTHCARE WASTE All Healthcare Workers have a ‘duty of care’ to ensure that waste is segregated, handled, transported and disposed of in an appropriate manner to ensure it does not harm staff, patients, the public or the environment. General Principles Waste should be disposed of at point of care in nearest appropriate bin Waste bags must be changed before ¾ full Waste bags must be swan necked or secured with a plastic tie to produce a fluid tight seal when closed Holding waste bags slightly away from the body will reduce risk if accidentally containing sharp object The waste storage/collection area should be inaccessible to animals and the public with waste being stored in locked bins provided by the waste contractor. Colour Waste type and description BLACK Domestic (municipal) waste Paper hand towels Tissues Food waste No hazardous waste in this waste stream. Recycling options should be considered. TIGER Offensive Non-infectious waste Contaminated items from non-infectious source e.g. dressings Incontinence pads Nappies Non-infectious disposable PPE e.g. gloves, aprons ORANGE Infectious waste (not containing chemicals or medicinal contamination) Contaminated items from known or suspected infectious patients Infectious disposable PPE e.g. gloves, aprons, face masks Infectious outbreak waste CLEAR Recycled waste plastic bottles drinks cans paper cardboard YELLOW lid sharps box Medicinally contaminated mixed sharps and pharmaceutical waste (not cytotoxic and cytostatic) This may include associated vials, bottles and ampoules of medicine ORANGE lid sharps box Non medicinally contaminated sharps PURPLE lid sharps box Items contaminated with cytotoxic and cytostatic medicines This may include associated vials, bottles and ampoules of cytotoxic and cytostatic medicines Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 13 of 16 RED lid Anatomical waste Anatomical waste for incineration (chemically and non-chemically preserved) e.g. podiatory anatomical waste BLUE lid Medicinal waste Medicinal waste (not cytotoxic and cytostatic) with or without original packaging Includes Prescription Only Medicines (POM) and Over the Counter (OTC) medications Refer to Waste Handling policy 6.11 LAST OFFICES When carrying out the last offices the following should be implemented. Wear PPE; gloves and apron Contain leakage from wounds and line sited by ensuring they are covered with a waterproof dressing After carrying out last offices a body bag must be used in the following circumstances: When a body is leaking body fluids or there is gross external contamination with blood Staff must ensure that mortuary staff are aware of the reason for using a body bag When a patient has or is strongly suspected of having one of the following biohazard conditions: Anthrax Classic or variant Creutzfeldt-Jakob disease (CJD) Diphtheria Hepatitis B, C HIV Meningococcal septicaemia / meningitis if death occurs before 48 hours of appropriate antibiotic therapy being completed Rabies virus Invasive β-haemolytic Streptococcus Group A disease if death occurs before 48 hours of appropriate antibiotic therapy being completed Tuberculosis Typhoid/ Paratyphoid Viral Haemorrhagic fever Any soiled patient’s clothing must be placed in a water soluble clothing bag which must be secured and placed inside a property bag. Any itemised list of contents must be attached. If in doubt contact the Infection Prevention and Control Team - Bleep 0064 Refer to When an Adult Dies Policy 7. TRAINING REQUIREMENTS All Trust staff clinical and non-clinical must be aware of the contents of this policy. Infection prevention and control is a key essential training course. All clinical staff are required to attend annual infection prevention and control updates, which would include practical and theoretical training. Staff must have dedicated time to maintain infection control competencies through education and peer support. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 14 of 16 Infection prevention and control training is available in number of formats including formal taught sessions, e learning and local training via the local infection control link advisor. Non-attendance at infection prevention and control training will be monitored via the quarterly reports to CSC Governance Groups. CSC leads will be required to develop action plans to target non-attendance and report the outcomes (quarterly) to the Strategic Learning and Development Committee. 8. REFERENCES AND ASSOCIATED DOCUMENTATION Department of Health (2008) The Health and Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance. Department of Health, December 2010. London. HMSO Department of Health. Safe Management of Healthcare Waste version: 2.0:England, DH. Loveday et al (2014). epic3: National Evidence-Based Guidelines for Preventing HealthcareAssociated Infections in NHS Hospitals in England. Journal of Hospital Infection 86S1 (2014) S1–S70 National Clinical Guideline Centre (2012). Infection: prevention and control of healthcareassociated infections in primary and secondary care. NCGC, London (partial update of NICE CG2) Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 2000;356:1307–1312. World Health Organization. WHO Patient Safety. WHO guidelines on hand hygiene in health care. Geneva: World Health Organization; 2009. 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together No waste This policy should be read and implemented with the Trust Values in mind at all times. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 15 of 16 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS Minimum requirement to be monitored Hand Hygiene/PPE Compliance Lead CSC Sharps / Innoculation Injury Occupational health Waste Compliance Contracts team Tool Frequency of Report of Compliance Hand Hygiene Monthly Audit Monthly DATIX Quarterly Reporting arrangements Policy audit report to: Infection Prevention Management Committee Lead(s) for acting on Recommendations Caroline Mitchell / CSC HoN Policy audit report to: Occupational health Health and Safety Audit Annual Policy audit report to: Estates / Monitoring Team This document will be monitored to ensure it is effective and to assurance compliance. Standard Infection Control Precautions Policy Version: 5 Issue Date: 07 August 2015 Review Date: 06 August 2017 (unless requirements change) Page 16 of 16