PEDIATRIC ORGAN DONOR MANAGEMENT
advertisement

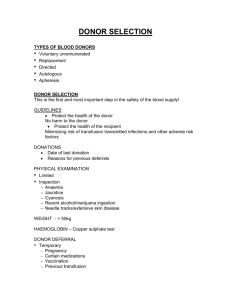
Number: DP-OR25 STANDARD OPERATING PROCEDURES Organ Recovery Services Title: PEDIATRIC ORGAN DONOR MANAGEMENT This document contains confidential and proprietary information and is the property of Donor Network of Arizona. Revision #: 06 Revision to Existing Document Annual Review Implementation Date: Effective Date: 1. Purpose: 1.1. 2. 3. Defines the expected management interventions for clinical organ donor management. Responsibilities: 2.1 Organ Recovery Coordinators (ORCs) are responsible for organ donor management and for consulting with the Medical Director about organ donor management. 2.2 The Organ Recovery Services Medical Director is responsible for giving clinical guidance as needed to ORCs and for approving variances from established guidelines on a case-by-case basis. 2.3 The Medical Executive Committee and the Medical Director are responsible for reviewing and approving donor management guidelines on an annual basis as part of the Medical Executive Committee meetings. Definitions: 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 4. New Obsolete STAT: mg: mcg: mEq/L: mmol: mmhg: hr: IV: Immediately Milligrams Micrograms Milliequivalents per liter Millimoles Millimeters of mercury Hour Intravenous References and/or Associated Documents: 4.1. 4.2. 4.3. United Network for Organ Sharing (UNOS), Policies 4.1.1. Policy 2.0: Minimum Procurement Standards for an Organ Procurement Organization. Association of Organ Procurement Organizations (AOPO), Standards 4.2.1. Standard CL 4A: Guidelines for Evaluation and Management of Potential Organ Donors Centers for Medicare and Medicaid Services (CMS), 42CFR486, Subpart G: Requirements for Certification and Designation and Conditions for Coverage: Organ Procurement Organizations DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 1 of 15 4.4. 4.5. 4.6. 4.7. 4.8. 5. Materials and Equipment as Needed: 5.1 6. 4.3.1. § 486.344 Condition: Evaluation and Management of Potential Organ Donors and Organ Placement and Recovery Powner, DJ et. al. Proposed Treatment Guidelines for Donor Care. Progress in Transplantation. 2004; 14:16-28 Lutz-Dettinger, N et. al. Care of the Potential Pediatric Organ Donor. Pediatric Clinics of North America. 2001: 48(3): 715-49 Zuppa, A et. al. The effect of a thyroid hormone infusion on vasopressor support in critically ill children with cessation of neurologic function. Critical Care Medicine. 2004; 32:2318–2322 DP-OR25 - Attachment I – Pediatric Donor Management Orders Checklist OP-CL01 – Hemodilution None Procedure: 6.1. General considerations 6.1.1. Guidelines for pediatric organ donor management are reviewed and approved annually by the Medical Executive Committee of Donor Network of Arizona (DNA). These guidelines are not intended to supplant the clinical decision-making of ORCs or physicians, including the Medical Director, on a case-by-case basis. 6.1.2. ORCs are encouraged to consult the Medical Director (or other available physician if the medical director is not available) for conditions not fully addressed within these guidelines, or if further guidance is needed. 6.1.3. ORCs are encouraged to call upon the physicians, registered nurses, respiratory care practitioners and other staff in the pediatric ICU setting (local, regional and national) for suggestions and advice. These individuals have vast experience caring for critically ill pediatric patients and their suggestions and advice should be considered at all times. 6.2. Guidelines for standard donor care 6.2.1. Upon assumption of donor care, the ORC will obtain a blood sample for serological testing according to OP-CL01 – Hemodilution and send it for STAT testing. 6.2.2. The ORC will order the following initial interventions, following established order procedures at the donor hospital: Note: The ORC may use DP-OR25 Attachment I – Pediatric Donor Management Orders Checklist and share it with the hospital staff to review plans for donor management. 6.2.2.1. Transfer care to DNA. 6.2.2.2. Monitor the following vital signs hourly: DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 2 of 15 6.2.2.2.1. Blood pressure (if arterial line no present, request placement) 6.2.2.2.2. Heart rate 6.2.2.2.3. Temperature 6.2.2.2.4. Oxygen saturation (SpO2) 6.2.2.2.5. Urine output 6.2.2.2.6. Central venous pressure (CVP) if a central line is present 6.2.2.2.6.1. 6.2.2.2.7. If a central line is not present, the ORC should request placement of a central line or (if patient is a potential heart or lung donor) a pulmonary artery catheter. Pulmonary artery (PA) pressures, including pulmonary artery occlusion pressures, if PA catheter is present. 6.2.2.3. Ventilator settings should be adjusted to optimize oxygenation of the organs. Recommended ventilator settings: 6.2.2.3.1. Tidal volume: 8-10 cc/kg of donor ideal body weight. 6.2.2.3.2. Ventilation rate: 16 breaths per minute. 6.2.2.3.3. Positive end-expiratory pressure (PEEP): 2.5 mmhg. 6.2.2.3.4. Fraction of inspired oxygen (FiO2): 40% (may adjust upwards or downwards to maintain PaO2 >100). 6.2.2.4. Elevate head of bed to 30 degrees. 6.2.2.5. Maintain temperature >36.5°C. 6.2.2.6. Continue routine pulmonary care including side-to-side positioning. 6.2.2.6.1 The ORC should consider the use of the intermittent mechanical pulmonary toilet devise commonly know as the “Link Vest” for additional pulmonary toilet maintenance. 6.2.2.7. Place nasogastric/orograstic tube, connect to low intermittent suction. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 3 of 15 6.2.2.8. If consent for cornea donation is obtained, administer 2 drops gentamycin ophthalmic solution and 0.6cm Lacrilube (or other corneal lubricant) to each eye, and tape eyelids shut (to prevent infection and corneal drying). 6.2.2.9. Continue vasoactive infusions at current settings. 6.2.2.9.1. The ORC should direct the titration of vasoactive infusions to maintain an age/size appropriate MAP and SBP following direction of pediatric intensivist / medical director should consider substituting medications for optimal perfusion of the organs. 6.2.2.10. Start levothyroxine protocol. 6.2.2.10.1. Administer 30mg/kg Solu-Medrol IV, with maximum dose of 2gms, every 12hrs. 6.2.2.10.2. Administer Levothyroxine bolus per age based protocol in table I. 6.2.2.10.3. Administer Levothyroxine IV infusion using the age appropriate rate per Table I. Age 0–6 months 6–12 months 1–5 years 6–12 years 12–16 years >16 years Table I Bolus 5 mcg/kg 4 mcg/kg 3 mcg/kg 2.5 mcg/kg 1.5 mcg/kg 0.8 mcg/kg Infusion 1.4 mcg/kg/hr 1.3 mcg/kg/hr 1.2 mcg/kg/hr 1 mcg/kg/hr 0.8 mcg/kg/hr 0.8 mcg/kg/hr 6.2.2.10.4. In the event the donor becomes tachycardic and hypovolemia is ruled out as the cause, discontinue levothyroxine therapy and consult medical director. 6.2.2.11. IV fluid: 5% Dextrose in 0.45 sodium chloride (D5½NS) with 20 mEQ potassium chloride (KCl) per liter is the recommended IV fluid. The ORC should choose fluids, rates and additives based on electrolyte levels and hypo/hypervolemic state. 6.2.2.12. Administer 8 mg/kg ciprofloxacin IV now and every 8 hours to prevent infection. If antibiotic therapy already in place, consult medical director as to suitability. If known sensitivity, substitute Vancomycin IV 10mg/kg every 6hrs, maximum dose 1gm/dose. 6.2.2.13. Order the following labs STAT (repeat PRN): 6.2.2.13.1. Comprehensive metabolic panel (CMP 6.2.2.13.2. Complete blood count (CBC) with differential 6.2.2.13.3. Prothrombin time (PT) and partial thromboplastin time (PTT) DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 4 of 15 6.2.2.13.4. Lipase 6.2.2.13.5. Amylase 6.2.2.13.6. Magnesium 6.2.2.13.7. Cardiac panel, to include Troponin-I, creatinine phosphokinase (CPK), and creatine-kinase (CKMB) 6.2.2.13.8. Cultures 6.2.2.13.8.1. Blood from two fresh sticks; do not draw from accesses >4 hours old 6.2.2.13.8.2. Sputum with stat gram stain 6.2.2.13.8.3. Urine 6.2.2.13.9. Urinalysis 6.2.2.14. Order a 12-lead electrocardiogram (EKG). 6.2.2.15. Order a portable chest x-ray (CXR)—indication: donor evaluation. 6.2.2.15.1. Consider delaying the CXR if central line placement is planned within one hour; the single CXR can then be used to check line placement as well. 6.2.2.16. If blood type (ABO) has not been determined, order ABO type and screen, to include subtyping if ABO=A. 6.2.2.17. Type and cross for two units of packed red blood cells (PRBCs) keep ahead two units throughout case. 6.2.2.18. Notify the ORC if any of the following situations occur: 6.2.2.18.1. Mean arterial pressure (MAP) or SBP drops below age appropriate parameters, as directed by pediatric intensivist/medical director. 6.2.2.18.2. Systolic blood pressure >170 mmhg 6.2.2.18.3. Heart rate <80 or >160 beats per minute 6.2.2.18.4. Temperature <36°C or >38°C 6.2.2.18.5. Urine output <1 cc/kg/hr 6.2.2.18.6. CVP or PAOP <6or >12 mmhg 6.2.2.19. Cardiac Donor Evaluation DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 5 of 15 6.2.2.19.1. Once donor SBP or MAP maintains at guidelines given in above with Dopamine <10mcg/kg/min and/or phenylephrine <60mcg/min, request cardiac consultation to include 2-dimensional echocardiography. 6.2.2.20. Pulmonary Donor Evaluation 6.2.2.20.1. Oxygen Challenge 6.2.2.20.1.1. Increase FiO2 to 100%; draw ABG at 30 minutes. 6.2.2.20.1.2. Decrease FiO2to 40%; draw ABG at 30 minutes. 6.2.2.20.1.3. Return FiO2to previous settings established in 6.2.2.3 of this SOP. 6.2.2.20.2. Bronchoscopy 6.2.2.20.2.1. If pO2 >300mmhg, request pulmonary consult, including CXR interpretation (including lung measurements) and fiber optic bronchoscopy. 6.2.2.20.2.2. Bronchoscopy should include separate bronchial washings from the right and left lung sent for culture, STAT gram stain and fungal smear. 6.2.2.20.3. Administer Albuterol nebulizer every 4 hours; consider adding Mucomyst nebulizer every four hours if secretions present. 6.2.2.20.4. Deep suction every two hours using one-time suction kit (including red rubber catheter if available, instead of in-line suction devise). 6.2.2.20.5. Give 30/kg Solu-Medrol (maximum dose 2 gm) IV 12hours after the dose given with the inception of the levothyroxine protocol. 6.2.2.20.6. Give Narcan 8mg IV pushonce. 6.2.2.20.7. Repeat oxygen challenge two hours after bronchoscopy and/or as requested by transplant center. 6.3. Guidelines for donors with hypertension 6.3.1. Because donor organs are at greater risk from hypotension than from hypertension, a conservative management approach to hypertension is DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 6 of 15 recommended. The goal for MAP should be less than 90 mmhg but greater than 50 mmhg. Therapy should be started if the MAP is sustained over 95 mmhg for a period of thirty minutes or longer. 6.3.2. Consider reducing vasoactive medications. 6.3.3. Consider a labetalol infusion at 0.4-1 mcg/kg/hr until a MAP of 65-70 mmhg is reached. 6.3.4. Consider a nitroprusside infusion at 0.1 mcg/kg/min; titrate slowly until a MAP of 65-70 mmhg is reached. Note: Consult medical director before using beta blockers in donors with a history of pulmonary disease. 6.3.5 6.4. If Nitroprusside fails to reduce the MAP, consult the Medical Director for further guidance. Guidelines for donors with hypotension 6.4.1. Hypotension in the brain-dead organ donor can be due to ongoing or preexisting conditions leading to hemorrhagic, cardiogenic, distributive, obstructive or other types of shock, but is more commonly due to the loss of vasomotor centers in the brain causing vasodilation, decreased contractility of the heart, or hypovolemia due to ongoing fluid loss due to diabetes insipidus. Hypotension in pediatric organ donors is defined as a MAP <50 mmhg. 6.4.2. Ensure that any signs of hemorrhage have been evaluated and treated. 6.4.3. Discontinue any anti-hypertensive medications. 6.4.4. Administer additional fluid such as 0.45% sodium chloride or Ringer’s lactate. Colloid solutions (5% albumin) may be added. 6.4.4.1. For CVP <5 mmhg, consider a 20 cc/kg fluid challenge. 6.4.4.2. For CVP 5-12 mmhg, consider a 15 cc/kg fluid challenge. 6.4.4.3. For CVP >12, no fluid challenge is indicated. 6.4.5. If a fluid challenge does not resolve the hypotension, consider the use of vasoactive medications. 6.4.5.1. Titrate dopamine to achieve MAP endpoints; maximum dose 20 mcg/kg/min, but consider use of other pressors if dopamine dose is >10mcg/kg/min or if donor becomes tachycardic. 6.4.5.2. Consider the use of vasopressin IV 0.00002-0.0003 U/kg/min especially if the patient is in diabetes insipidus. Monitor pt’s urine output closely and discontinue if the urine output is <1cc/kg/hr. 6.4.5.3. If dopamine is ineffective, add phenylephrine at 0.1-0.5 mcg/kg/min, Titrate to a maximum dose of 200 mcg/min. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 7 of 15 Maximum dose may be exceeded with medical director approval. 6.4.5.3.1. Alternately, the ORC may consider the use of epinephrine 0.05mcg/kg/min, titrate up to 1 mcg/kg/min. 6.4.6. If PA monitoring is available, obtain a cardiac/hemodynamic profile. 6.4.6.1. If the systemic vascular resistance index (SVRI) is <1400, consider the immediate use of a vasopressor such as phenylephrine, norepinephrine, or epinephrine. 6.4.6.2. If the left ventricular stroke work index is low (<35 g m/m2) consider the use of a positive inotropic agent such as dopamine or dobutamine. 6.4.7. Continue to monitor hemodynamic status and titrate all vasoactive drips to minimum levels. 6.5. Guidelines for glucose management 6.5.1. Monitor glucose level every 2 hours either by normal labs or by fingerstick. 6.5.2. Hypoglycemia 6.5.2.1. For hypoglycemia (glucose <75 mg/dL), administer 50 ml of 25% dextrose IV (in donors under 1 year of age, use a 10% dextrose solution). 6.5.2.2. Check glucose via fingerstick in 30 minutes and repeat 25% dextrose if the donor glucose level <75 mg/dL (in donors under 1 year of age, use a 10% dextrose solution). 6.5.2.3. If the glucose remains <75 mg/dL after the second 25% dextrose administration, consult the Medical Director. 6.5.3. Hyperglycemia 6.5.3.1. For hyperglycemia (glucose >300 mg/dL), ensure that all glucose is removed from fluids and infusions unless required by pharmacy. 6.5.3.2. Administer insulin 0.1 unit/kg IV and recheck glucose level 30 minutes after administration. 6.5.3.3. If glucose remains >300 mg/dl, repeat dose. 6.5.3.4. If glucose remains > 300 mg/dl after repeat dose, start insulin infusion 0.05-0.1 units/kg/hr; titrate based on hourly glucose levels. 6.5.3.5. When treating hyperglycemia with insulin, monitor serum glucose hourly via fingerstick. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 8 of 15 6.6. Guidelines for temperature management 6.6.1. Temperature should be monitored from a core site, such as a PA catheter, bladder catheter, or rectal temperature. Axillary and oral temperatures should not be used. 6.6.2. Hypothermia (donor temperature <36°C). 6.6.2.1. If the donor temperature is <36°C, use active surface warming, such as warm blankets, or hot air warming blanket with insulating thermal blankets. 6.6.2.2. Cover the donor’s head and other exposed body surfaces to minimize exposure to room temperature. 6.6.2.3. If the temperature remains <36°C after three hours of active rewarming, consult the Medical Director. 6.6.3. Hyperthermia (donor temperature >38°C) 6.6.3.1. Hyperthermia is rare in organ donors. 6.6.3.2. Remove additional blankets. 6.6.3.3. Administer 10 mg/kg acetaminophen per suppository every three hours. 6.6.3.4. Use cooling blanket. 6.6.3.5. If temperature remains >38°C after three hours of cooling, consult the Medical Director. 6.7. Guidelines for anemia (donor hematocrit <28%) 6.7.1. Review the medical record for evidence of bleeding sites, previous transfusion requirements, or other information about blood loss and/or hemolysis. 6.7.2. Observe for signs of bleeding from external wounds, IV sites, gastrointestinal (GI) tract (via gastric tube or bowel movements), and urinary tract. 6.7.3. Observe for abdominal distension and changes in abdominal firmness over time. 6.7.4. Refer to section 6.8 of this policy for coagulopathy treatment guidelines and obtain PT, PTT, fibrinogen and platelet count. Treat as indicated. 6.7.5. If hematocrit is < 28%, transfuse 5 cc/kg PRBC rapidly. Please give CMV negative blood if available. 6.7.6. Reassess the hematocrit level 30 minutes after the end of the transfusion and repeat the transfusion if the hematocrit remains <28%. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 9 of 15 6.7.7. If the hematocrit remains <28% after a total of 20 cc/kg of PRBCs, consult the medical director. 6.7.8. Administer 20mg/kg/dose of calcium chloride for every four pediatric RBC’s transfused. 6.8. Guidelines for treating coagulopathy and thrombocytopenia 6.8.1. Review the donor medical record for any anticoagulant medications that have been given. Consult with medical director if any anticoagulants have been administered within the past 48 hours, or if the patient has been on outpatient anticoagulant therapy. 6.8.2. Send PT, PTT, fibrinogen, d-dimer, and platelet count. 6.8.3. Platelets 6.8.3.1. If platelet count < 80,000/mL3, administer 30 cc/kg of pooled platelets rapidly. 6.8.3.1.1. If using single donor platelets, administer in doses of 10 cc/kg due to higher concentrations. 6.8.3.2. Recheck platelet count 30 minutes after infusion ends and repeat infusion if platelet count remains <80,000/ mL3. 6.8.3.3. If platelet count remains <80,000/ mL3after the second platelet infusion, consult medical director. 6.8.4. Coagulopathy with PT >15 seconds and/or PTT >38 seconds 6.8.4.1. If patient had been receiving IV heparin and PTT >75 seconds, consider protamine administration. Consult with the Medical Director. 6.8.4.2. Rapidly infuse 10-15 cc/kg fresh frozen plasma (FFP) and repeat PT/PTT 30 minutes after the end of the infusion. 6.8.4.3. Repeat the infusion if PT/PTT remain above the treatment ranges. 6.8.4.4. If PT/PTT remain elevated after second dose of FFP, consult the Medical Director. 6.8.5. Coagulopathy with fibrinogen <100 mg/dL. 6.8.5.1. Infuse 5 cc/kg cryoprecipitate rapidly. 6.8.5.2. Repeat fibrinogen 30 minutes after infusion ends; repeat infusion if fibrinogen level remains <100 mg/dL. 6.8.5.3. If fibrinogen level remains <100 mg/dL after the second infusion, consult the Medical Director. 6.9. Mechanical ventilation of donors DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 10 of 15 6.9.1. Volume-controlled ventilator settings 6.9.1.1. Tidal Volume (Vt): 8-10 cc/kg ideal body weight 6.9.1.1.1. If peak airway pressures >30 cm H20, reduce Vt to 6-8 cc/kg. 6.9.1.2. Adjust rate to maintain minute ventilation of approximately 8-10 L/minute or to maintain PaCO2 between 16-50 mmhg. 6.9.1.3. Adjust positive end-expiratory pressure (PEEP) to a minimum of 5 cm H20, titrate to maintain PaO2 > 100 mmhg. 6.9.1.4. Adjust FiO2 to maintain PaO2>100 mmhg. 6.9.2. Pressure-limited ventilator settings 6.9.2.1. Peak inspiratory pressure of 35-40 cm H20; consult with respiratory care practitioner for recommendations based on the specific ventilator model. 6.9.2.2. Adjust rate to maintain minute ventilation of approximately 4-6 L/minute or to maintain PaCO2 between 16-50 mmhg. 6.9.2.3. Adjust PEEP to a minimum of 5 cm H20, titrate to maintain PaO2 > 100 mmhg. 6.9.2.3.1. PEEP adjustments may change delivered Vt and minute volume during pressure-limited ventilation. 6.9.2.4. Adjust FiO2 to maintain PaO2 >100 mmhg. 6.9.3. General therapy 6.9.3.1. Ensure adequate suctioning/pulmonary toilet. 6.9.3.2. Consider use of Link Vest system. 6.9.4. Ventilator adjustments 6.9.4.1. Consult with pediatric intensivist and/or pediatric respiratory care practitioner for optimal ventilator management. 6.9.4.2. Goals for ventilatory management of pediatric organ donors: 6.9.4.2.1. SpO2 >95% 6.9.4.2.2. PaO2 90-110 mmhg 6.9.4.2.3. pH 7.35-7.45 6.9.4.2.4. pCO2 35-45 mmhg 6.9.4.3. Check ABG 30 minutes after each ventilator change. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 11 of 15 6.9.4.4. Maintain peak inspiratory pressures <35 cm H20. 6.9.4.5. Adjust tidal volume to 8-10 cc/kg. 6.9.4.6. Apply PEEP at 5 cm H20. Increase to maximum of 10 cm H20 for refractory hypoxemia. 6.9.4.7. Turn and bag suction every two hours. 6.9.5. Guideline for management of fluids and electrolytes 6.9.5.1. Hypernatremia (sodium >150 mmol/l) 6.9.5.1.1. In the presence of polyuria (>250ml urine output above intake per hour) see polyuria guideline in section 6.9.6 of this Standard Operating Procedure (SOP). 6.9.5.1.2. Without polyuria: 6.9.5.1.2.1. Give 10 cc/kg 0.2% sodium chloride with 20mEq KCL/L solution as rapid infusion. 6.9.5.1.2.2. Replace urine output mL/mL per hour with 0.2% sodium chloride solution with 20 mEq KCL/L or D5W. 6.9.5.1.2.3. Ensure that all medications are mixed in 0.45% sodium chloride solution or 0.2% sodium chloride solution if pharmaceutically possible, and that any maintenance IV fluid is changed to 5% dextrose in water (D5W) or 5% dextrose in 0.2% sodium chloride solution. 6.9.5.1.2.4. Avoid the use of diuretics. 6.9.5.2. Hyponatremia (sodium < 133 mmol/L) 6.9.5.2.1. Ensure that all medications are mixed in 0.9% sodium chloride solution if pharmaceutically possible, and that any maintenance IV fluid is changed to 5% dextrose 0.9% sodium chloride solution. 6.9.5.2.2. Correct hyperglycemia before addressing hyponatremia (see section 6.5.3 of this SOP). 6.9.5.2.3. If the sodium level remains <133 mmol/L after three hours, consult the Medical Director. 6.9.5.3. Hyperkalemia (potassium > 5.8 mmol/L) DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 12 of 15 6.9.5.3.1. Do not treat hyperkalemia if the lab reports the specimen as hemolyzed. Send a new specimen. 6.9.5.3.2. Ensure that all potassium is removed from infusions. 6.9.5.3.3. If hyperkalemia persists: 6.9.5.3.4. 6.9.5.3.3.1. Give 1 mL/cc 25% dextrose IV. 6.9.5.3.3.2. Give 0.1 units/kg regular human insulin IV. 6.9.5.3.3.3. Give 1 mEq/kg sodium bicarbonate (1 ampoule) IV. 6.9.5.3.3.4. Measure potassium level one hour after medication administration. If hyperkalemia persists, consult the Medical Director. 6.9.5.4. Hypokalemia 6.9.5.4.1. Delay diuretic administration. 6.9.5.4.2. Give 0.5-1 mEq/kg potassium chloride over 60-90 minutes (preferably via central catheter). 6.9.5.4.2.1. Alternately, consider the use of potassium acetate. Consult with pharmacist for dosing. 6.9.5.4.3. Repeat up to four doses if serum potassium remains <2.9 mmol/L. 6.9.5.4.4. If hypokalemia persists, consult the Medical Director. 6.9.5.5. Hypomagnesaemia (serum magnesium <1.5 mg/dL) 6.9.5.5.1. Consult the Medical Advisor. 6.9.5.6. Hypophosphatemia (serum phosphate <2.2 mg/L) 6.9.5.6.1. Consult the Medical Director. 6.9.5.7. Hypoionized calcemia (ionized calcium < 1.1 mmol/L or <4.4 mg/dL) 6.9.5.7.1. Consult the Medical Advisor. 6.9.6. Guidelines for treating polyuria DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 13 of 15 6.9.6.1. Evaluate for hyperglycemia and treat according to section 6.5.3 of this SOP. 6.9.6.2. Stop any prescribed diuretic therapy. 6.9.6.3. Calculate current intake and output for pt and consider boluses for deficit >250cc.Monitor serum sodium and glucose levels every two hours. 6.9.6.4. If the serum sodium level is between 135-147 mEq/L, continue to observe urine output and continue to monitor sodium and glucose. 6.9.6.5. If the serum sodium level >148 mEq/L: 6.9.6.5.1. If urine output >5 cc/kg/hr above IV intake over two hours, start IV vasopressin at 0.0005 unit/kg/minute. 6.9.6.5.2. Vasopressin may be titrated to a maximum dose of 0.01 units/kg/hr. Observe the donor for signs of hypertension. 6.9.6.5.3. If the urine output does not decrease below 3 cc/kg/hr after two hours at the maximum vasopressin dose, consult the Medical Director. 6.9.6.5.3.1. Alternatively, the ORC may consider the use of 0.05-0.1 mcg desmopressin IV if the patient is hypertensive. 6.9.6.5.3.2. The desmopressin dose may be repeated once if the urine output does not decrease over two hours. 6.9.6.5.3.3. If the urine output does not decrease after two doses, consult the Medical Director. 6.9.7. Guideline for acid-base management 6.9.7.1. Metabolic acidosis 6.9.7.1.1. If the arterial pH remains < 7.32 after the changes recommended in section 6.9.4 of this SOP, administer 1 mEq/kg sodium bicarbonate slow IV bolus. Recheck the ABG in 30 minutes. 6.9.7.1.1.1. If the serum sodium > 150 mEq/L at any time, consult the medical director before administering any sodium bicarbonate. DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 14 of 15 6.9.7.1.2. If the arterial pH remains < 7.32 30 minutes after the first dose, administer a second dose of sodium bicarbonate. 6.9.7.1.3. If the arterial pH remains < 7.32 after two doses, consult the Medical Director. 6.9.7.2. Metabolic alkalosis 6.9.7.2.1. If the arterial pH remains >7.45 after the treatment changes recommended in section 6.9.4 of this SOP, consult the Medical Director. 6.9.8. Guidelines for infection 6.9.8.1. If the donor has bacterimia confirmed by culture, consult with the Medical Director and/or hospital pharmacist for an organismspecific antibiotic. 6.9.8.2. If the donor has a depressed white blood cell (WBC) count and an elevated band count on differential, consult with the Medical Director for specific therapy. 6.9.8.3. If the donor is showing signs of systemic infection (hypoperfusion, elevated temperature, decreased SVRI) consult with the Medical Director for specific therapy. Changes since last revision: Changes originated by: PJ Geraghty Removed direct/indirect bilirubin and GGT requirements (no longer required by UNOS). Added references to CMS, AOPO and UNOS policies. Approval Signatures: Associate Director, Organ Recovery Services Date Director, Organ Recovery Services Date Director, Quality and Regulatory Affairs Date Medical Director, Organ Recovery Services Date DP-OR25.06 – PEDIATRIC ORGAN DONOR MANAGEMENT Page 15 of 15