CASE REPORT PERFORATED GASTROINTESTINAL STROMAL
advertisement

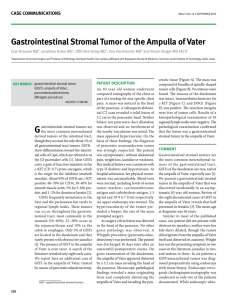
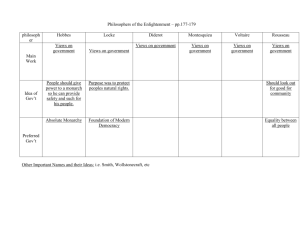
CASE REPORT PERFORATED GASTROINTESTINAL STROMAL TUMOUR OF JEJUNUM - A RARE CASE OF ACUTE ABDOMEN AND REVIEW OF LITERATURE R.D. Jaykar1, P. Kasabe2, S.C. Jadhav3, R.R. Ghule4 HOW TO CITE THIS ARTICLE: RD Jaykar, P Kasabe, SC Jadhav, RR Ghule. “Perforated gastrointestinal stromal tumour of jejunum - a rare case of acute abdomen and review of literature”. Journal of Evolution of Medical and Dental Sciences 2013; Vol2, Issue 51, December 23; Page: 9890-9894. ABSTRACT: A case of perforated gastrointestinal stromal tumour of jejunum causing acute abdomen is described with review of literature. A 58 years old male patient presented with symptoms of acute abdomen. Patient was diagnosed as acid peptic disease with perforation peritonitis. After evaluation exploratory laparotomy was performed, where it was a diverticulum from jejunum was perforated at its tip with gross peritoneal contamination. Diverticulectomy was performed. Histopathology examination showed that, diverticulum was benign gastrointestinal stromal tumour. Gastrointestinal stromal tumours are relatively rare and eventually rare to present with perforation. KEY WORDS: Gastrointestinal stromal tumour, diverticulum, perforation peritonitis INTRODUCTION: Gastrointestinal stromal tumors (GISTs) are very rare mesenchymal tumors of the GI tract with a frequency of approximately 10-20/1,000,000 population (1, 2). GISTs are the most common mesenchymal tumors of the GI tract. GIST is a rare visceral sarcoma arising in the GI tract, and usually occurs in the stomach (60-70%) or small intestine (25-35%). Colon, rectum, appendix (together 5%) and esophagus (2-3%) are rare sites (8%) (3). Velasco et al. reported that the jejunal GIST accounts for approximately 10% of all cases (4). The currently used diagnostic modalities include barium studies, computed tomography (CT) and angiography; however, none of these can establish a preoperative diagnosis with 100% certainty (5, 6). Hence we are presenting the case of ruptured GIST of jejunum which was diagnosed as jejunal diverticulum perforation CASE REPORT: A 58 years male patient admitted with pain in abdomen, vomiting and fever since 4 hours. On examination, his pulse rate was 96/min and blood pressure 110/70 mm Hg, body temperature was 37.8o C. Physical examination revealed, tenderness all over the abdomen with guarding. Laboratory investigations were normal. Plain X ray erect abdomen revealed free gas under diaphragm. Patient was operated with initial diagnosis of hallow viscus perforation with peritonitis. On exploration, there was contamination of peritoneal cavity with bile stained fluid with diverticulum like mass of size 3x2 cm on antimesenteric border of jejunum 15-20cm from duodenojejunal flexure. Diverticulum along with margins of normal healthy bowel excised and defect closed in double layer with inner absorbable and outer non absorbable suture material. Stomach, duodenum, rest of small bowel and colon inspected and were within normal limits. Histopathological examination of mass turned out as benign GIST lesion. Postoperative course of the patient was uneventful. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 51/ December 23, 2013 Page 9890 CASE REPORT Fig. 1: Diverticulum like mass Fig. 3: After first layer Fig 2: After diverticulectomy & excision of tissue Fig. 4: Post operative photograph Fig. 4 & 5: Showing microscopic features of GIST DISCUSSION: In this case report, a gastrointestinal stromal tumor of the jejunum is reported in which the tumor was spontaneously ruptured into peritoneal space and presented with the acute abdomen. The etiology and pathogenesis of these tumors are unknown. Their incidence increases between 60 to 70 years of age and they are predominant in males. The most common signs and symptoms of GISTs include abdominal pain, abdominal mass, GI hemorrhage, partial or complete Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 51/ December 23, 2013 Page 9891 CASE REPORT small bowel obstruction, weight loss, and fever or abscess (7). For the diagnosis of GISTs, several radiologic modalities such as CT, barium studies and/or angiography are used; however, none of these modalities can establish the correct diagnosis with 100% certainty (5, 6). Preoperative fine needle aspiration biopsy is not indicated because of the risk of tumor rupture and intraperitoneal seeding. Small sized tumors (<2 cm) are usually asymptomatic, and are discovered incidentally, while larger lesions present as large abdominal masses, with or without clinical manifestations. The symptoms and signs are not disease-specific and as a consequence about 50% of GISTs have already metastases at the time of diagnosis, usually to the liver or the peritoneum. Recently, several studies pointed out the significance of endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of GIST with a reported accuracy of 89%. On the other hand, positron-emission tomography (PET) with 18F-fluoro-2-deoxy-D-glucose is a very useful tool for the postoperative follow-up of patients receiving imatinib (8, 9) GISTs can be categorized as low or high-risk tumors by taking into account the possibility of metastasis or recurrence. However, the main prognostic factor is the mitotic count. A prognostic classification was defined by Fletcher et al and is widely accepted and used today. (10) Risk of malignancy Size of Very low low intermediate High tumor (cm) Mitotic counts (/50HPF) <2 <5/50 2 -5 <5 <5 6-10 5-10 <5 >5 >5 >10 Any count Any size >10 Table 1: GISTs classification by Fletcher et al (10) Immunohistochemical examination of GISTs is always positive for KIT protein (CD117 antigen), while the positivity regarding other markers varies (Table II). Marker Positivity KIT (CD117 antigen) 100% CD34 70% SMA 20-30% S100 10% Desmin <5% Table 2: Proportion of GISTs positivity for various immuno-histochemical marker The treatment of choice for GISTs is the surgical excision of the tumor. All tumors must be completely resected (R0 resection), where possible, including the tissues that are infiltrated, while systemic lymph node dissection is not recommended by many authors. The prognosis is dismal when the tumor presents with symptoms or signs such as perforation, multifocal location or metastatic Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 51/ December 23, 2013 Page 9892 CASE REPORT lesions (11). Perforation of the tumor lowers the five-year survival to 24%, probably due to peritoneal dissemination. GIST response to conventional chemotherapy is very poor (<10%), while radiotherapy is only used in cases of intraperitoneal hemorrhage, when the precise location of the tumor is known, or for analgesic purposes. (7) The substance STI571, which has been named imatinib, was found to act as a powerful selective inhibitor of tyrosine kinases (c-ABL, BCR-ABL), of PDGFR receptor (platelet derived growth factor receptor) and of c-kit receptor. Imatinib is well tolerated by oral administration, and the suggested efficient dose must be >300 mg per day to achieve curative results. (12) REVIEW OF LITERATURE: An extensive review of the English-language literature regarding GISTs revealed only few reports about perforation of the tumor. In our case, the perforated tumor was transmural growth, and there were specific intraluminal mucosal changes in the jejunum. The perforated tumor communicated with the jejunum, and then the GI contents effused via the hole of the tumor causing acute diffuse peritonitis. GISTs are usually associated with abdominal pain, palpable mass, or GI bleeding, accompanied by fever, anorexia, weight loss, or anemia. Approximately 10-30% of patients with GISTs may be asymptomatic. However, GISTs originating from the jejunum rarely cause perforation, and also rarely cause acute diffuse peritonitis. These atypical clinical symptoms are extremely rare, and have been reported in very few literatures previously. It was difficult to diagnose a GIST because of the extremely rare clinical symptoms above, and it was also difficult to differentiate the tumor on images. The mechanism of bowel perforation secondary to GIST is unclear. In the review of Miettinen and Lasota, the most common presentation of GIST is reported as GI bleeding. The tumors smaller than 2 cm in size are generally asymptomatic and larger tumors may present with upper abdominal pain, palpable intra abdominal mass, vomiting, weight loss, and perforation or rupture. In current case the patient has admitted with the acute abdomen due to rupture of a GIST of small bowel. Tumor rupture in small bowel presenting as acute abdomen is the rarest clinical presentation of GIST and the mechanism is unclear. Karagulle et al., suggested that the reason of the perforation or rupture of GIST is the replacement of the bowel wall by tumor cells followed by necrosis, ischemia of the intestine due to tumor embolization, and increased intraluminal pressure caused by obstruction. CONCLUSION: Patients with GISTs have limited treatment options due to difficulty in preoperative and intraoperative diagnosis. Patient with complication such as perforated tumour or metastatic tumour have worst outcome. Since in our case, the preoperative as well as intraoperative diagnosis was not confirmed and patient presented with tumour in the small bowel with perforation, GIST should be kept in mind. REFERENCES: 1. Connolly EM, Gaffney E, Reynolds JV. Gastrointestinal stromal tumors. Br J Surg 2003; 90:1178-1186. 2. Joensuu H, Kindblom LG. Gastrointestinal tumors - a review. Acta Orthop Scand Suppl 2004; 75:62-71. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 51/ December 23, 2013 Page 9893 CASE REPORT 3. Miettinen M, Lasota J. Gastrointestinal stromal tumors definition, clinical, histological, immunohistochemical and molecular genetic features and differential diagnosis. Virchows Arch 2001; 438: 1-12. 4. Velasco S, Millin S, Murel C, et al. Scanographic features of gastrointestinal stromal tumors. Gastroenterol Clin Biol 2008; 32: 1001-13. 5. Bucher P, Villiger P, Egger JF et al. Management of gastrointestinal stromal tumours: from diagnosis to treatment. Swiss Med Wkly 2004; 134:145-153. 6. Fang SH, Dong DJ, Zhang SZ, Jin M. Angiographic findings of gastrointestinal stromal tumor. World J Gastroenterol2004; 10:2905-2907. 7. Crosby JA, Catton CN, Davis A, et al. Malignant gastrointestinal stromal tumors of the small intestine: a review of 50 cases from a prospective database. Ann Surg Oncol 2001; 8: 50-9. 8. VanderNoot MR 3rd, Eloubeidi MA, Chen VK et al. Diagnosis of gastrointestinal tract lesions by endoscopic ultrasound-guided fine-needle aspiration biopsy. Cancer 2004; 102:157-163. 9. Gelibter A, Milella M, Ceribelli A et al. PET scanning evaluation of response to imatinib mesylate therapy in gastrointestinal stromal tumor (GIST) patients. Anticancer Res 2004; 24:3147-3151. 10. Chen TW, Liu HD, Shyu RY et al. Giant malignant gastrointestinal stromal tumors: recurrence and effects of treatment with STI-571. World J Gastroenterology 2005; 11:260-263. 11. Aparicio T, Boige V, Sabourin JC et al. Prognostic factors after surgery of primary resectable gastrointestinal stromal tumors. Eur J Surg Oncol 2004; 30:1098-1103. 12. Verweij J, Casali PG, Zalcberg J et al. Progression-free survival in gastrointestinal stromal tumors with high-dose imatinib: randomised trial. Lancet 2004; 364:1127-1134. AUTHORS: 1. R.D. Jaykar 2. P. Kasabe 3. S.C. Jadhav 4. R.R. Ghule PARTICULARS OF CONTRIBUTORS: 1. Associate Professor, Department of General Surgery, V.M. GMC, Sholapur, Maharashtra, India. 2. Assistant Professor, Department of General Surgery, V.M. GMC, Sholapur, Maharashtra, India. 3. Assistant Professor, Department of General Surgery, V.M. GMC, Sholapur, Maharashtra, India. 4. Resident, Department of General Surgery, V.M. GMC, Sholapur, Maharashtra, India. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rahul R. Ghule, Vilegaon Post, Karanja Lad Tq, Washim Dist, Maharashtra – 444110. Email- ghulerahul1234@rediffmail.com Date of Submission: 04/06/2013. Date of Peer Review: 05/06/2013. Date of Acceptance: 14/09/2013. Date of Publishing: 17/12/2013 Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 51/ December 23, 2013 Page 9894