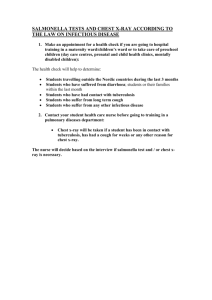
Case report
advertisement

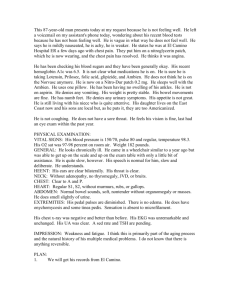
Chief complaint: palpitation and chest tightness this morning Present illness: This 54 y/o female suffered from palpitation and chest tightness this morning. She felt chest pain around the sternum without radiating to back or other areas. The chest discomfort persisted for more than 30 mins . She denied shortness of breath but felt she couldn’t take a deep breath ; felt better if she sat down and take a rest. At this time, she also felt headache, and headlightness , dizziness, general weakness but wouldn’t feel nausea and vomiting. .She had past medical history of hypertension about three years and she was regularly followed up on our OPD. She had past medical history of hyperlipidemia for three years but denied smoking and DM history. Malaise and sleepy as well as anorexia occurred from three years ago. Sometimes she felt chest uncomfortable but these symptoms could get better when she took a rest. Her discomfort became worsen this morning, so she visited our OPD where EKG was performed and the data showed slow VT. She was then admitted to our CCU for further evaluation and management. She had borderline positive Treadmill test on 2002-6-17. Dr Buttrey’s rewrite: CC: 54 y/o female c/o chest tightness for > 30 min PI: The patient c/o chest tightness and palpitation [?description] persisting for >30 min the morning of admission. The chest discomfort was around the sternum [?sub- or retrosternal] but did not radiate elsewhere. She denied SOB but felt she couldn’t take a deep breath. The symptoms were improved by rest. She also noted headache, lightheadedness and general weakness but no nausea or vomiting. She presented to the ER where an EKG showed slow VT, so she was admitted to the CCU. She had noted mild chest discomfort [?with exercise] relieved by rest for [How long? Frequency?]. She had a borderline positive treadmill test on 2002-6-17. [Further evaluation and/or treatment?]. She has a 3-year history of HTN with [? treatment, ?degree of control] and hyperlipidemia [? treatment, ?degree of control]. She denies DM, smoking [?or FH of heart disease]. She c/o malaise, sleepiness, and anorexia for the past 3 years. Missing data: What sort of palpitation did the patient experience—fast, irregular, etc.? The location of the chest pain needs to be described a little more accurately, because some patients have chest wall pain, e.g., from costochondritis. Substernal (=retrosternal) describes pain inside the chest. What was she doing when the discomfort began? How long ago did she first start having chest discomfort, what was its usual duration, and how frequent was it? Have any of these parameters been worsening lately? Why and where was the treadmill done and what recommendations were made then? What medication is she on for her HTN and lipids and how well controlled are these problems? A FH of early MI or cardiac death is another risk factor to note, as well as a sedentary lifestyle. If she’s been anorexic, has she lost weight? Comments Content: This is generally a good history. It’s certainly adequate to direct our attention to her heart, even if she hadn’t had VT in the ER. (We don’t need a description of her palpitation to make the diagnosis in this case, but in cases that are less clear, it’s good to ask the patient to describe what they felt, how long the episodes lasted if intermittent, did they take their pulse, etc.) One important point to note is that phrases like “this morning” are not specific enough. We need to know the exact duration of the symptoms and whether they were still present when the patient arrived in the ER. While the acute episode is fairly clear, more detail about her past history would be helpful. It sounds as if she’s been having episodes of angina for some time, but the onset, duration, and frequency are important to ask about. (Again, for this acute episode, we don’t need that information because we know she has VT and therefore something not very good is going on!) But we should routinely be asking patients with chronic angina about their symptoms because, if they become worse, we need to do something about it. It’s better to find that out in the OPD and do something about it electively rather than have the patient present in the ER with and acute coronary syndrome.) Details about the interpretation and response to the treadmill should be included. Was she given any medication as a result of that test, and if so, with what effect? Were other studies recommended? Hypertension and hyperlipidemia are clearly important in this history, since they are modifiable risk factors for CAD. Were we successfully modifying them? Stating that the patient was regularly followed does not tell us if she was adequately treated. ( A recent study in the US showed that only about 25% of hypertensive patients regularly followed by a physician had adequate control of their BP. Even though the doctors were recording consistently elevated BPs in the chart, they apparently weren’t responding appropriately to this data.) The old chart should be reviewed to see what medications she was on and what her usual BP and lipids were. She should also be asked about her compliance in taking the medications. The malaise, sleepiness and anorexia probably need more investigation. It’s not clear if they relate to the PI or not, but sometimes we include such information because it might relate. I wonder specifically if they are related to medications for the HTN and lipids, since the symptoms apparently began about the same time these illnesses were diagnosed. English: without radiating to back: “without radiation to the back” It’s better to use a noun here, and a noun form of the word already exists. Don’t use a gerund (i.e., the nominal form of a verb made by adding “ing”) unless there is no noun form. and take a rest: “and rested” or “and took a rest” Use the past tense to describe past events. You don’t need the extra words “took a.” They are grammatically correct but unnecessary. “Rest” is a verb as well as a noun. but wouldn’t feel nausea and vomiting: “but didn’t have nausea and vomiting” Again, use the simple past tense. While it’s true that nausea is a sensation, vomiting isn’t, so the very “feel” isn’t appropriate. If you’re describing a sensation only, you can use either “feel” or “have.” headlightness , dizziness: “lightheadedness” In the sentence you wrote, these words are equivalent, so only use one. “Dizzy” is used in 2 ways in English: 1) for the specific sensation of vertigo and 2) as a generic term that may denote either vertigo or lightheadedness (i.e., near-syncope). If an English-speaking patient tells me she is dizzy, I have to ask for more details to differentiate the 2 meanings. However, when a patient denies any such symptom, it’s fine just to use “dizziness” in the generic sense. That’s the word I would use here. malaise and sleepy as well as anorexia: Malaise and anorexia are nouns, so you must use the noun “sleepiness” rather than the adjective. Chief Complaint: Foreign body miss swallowed yesterday Present Illness: • This 52 y/o female p‘t has a past history of Hypertension,seizure with regularly followed up and well control. • Food impaction(bezoar) was noted last night ,so she was brought to LMD for help by her daughter and then transfered to our ER. At ER, dysphagia, spit sputum without blood and food impaction was noted ,but p’t denied dyspnea, short of breath, palpitation or chest tightness. • She felt nausea and vomited with some mucous sputum. Chest X-ray was performed and foreign body was noted in esophagus of the neck. • And then, foreign body was removed from esophageoscopy by ENT doctor. After the procedure, persisting, progressive periumbicial pain without radiating to other areas was noted and then NG tube was setting. • Unfortunately, flash blood from NG tube was noted. P’t denied gastric ulcer, gastroesophagial reflux history. She denied liver cirrhosis and esophageal varices history. • She denied tarry stool, change of appetide or bowel habit recently and she was never food impaction like this time before. Then, she was admitted to our ward for further evaluation and treatment. Dr Buttrey’s rewrite: CC: 52 y/o female c/o swallowing a foreign body PI: The patient had the sensation of food impacted in her esophagus while eating [What was she eating? How long after the incident did she see the first doctor? Did she vomit and/or retch a lot?]. She went to an LMD and then was transferred to the MMH ER, where she complained of dysphagia and nausea and was regurgitating mucous without blood. She denied dyspnea, palpitation, or chest tightness. On CXR there was a foreign body of the esophagus in the cervical area. [What was actually seen?] An ENT doctor removed the foreign body using esophagoscopy. [What was it?!!!!] After the procedure, she complained of periumbilical pain without radiation. An NG tube was placed which suddenly began to drain blood [?initial material]. The patient denied a history of PUD, GERD, liver disease, melena, recent change in appetite or bowel habits and had never previously had an episode of food impaction. [Any previous history of dysphagia of any type?] She had a history of seizures well-controlled on medication. [Any recent seizures or any loss of consciousness and/or seizure activity at the time of the incident.] Missing data: What she was eating, whether she has dentures, how quickly she sought medical care, what was actually seen on CXR (Some foreign bodies are radio-opaque, others are not. Describe what was actually seen.), and what the foreign body was. Was the initial NG aspirate clear, with the bleeding only beginning later? Any change in the vital signs when the bleeding began? Is she completely seizure-free? Comments Content: This was a very frustrating history to read because I wanted to know what was taken out of her esophagus! In fact, it’s unclear if at was truly a foreign body (i.e., something that normally would not be in the body) or if it was simply a bolus of food that got stuck. (It would not have been a bezoar—a concretion of swallowed hair, fruit or vegetable fibers, or similar substances found in the alimentary canal—unless she had one in her stomach which she regurgitated. That’s not what the story sounds like.) The fact that something was seen on in the esophagus on CXR makes food less likely, unless she’d swallowed a bone, which could show up if it were large enough. Metallic foreign bodies are usually opaque and can sometimes be identified by their shape. But even harder to understand is why the thing retrieved on endoscopy isn’t described. Don’t leave the reader guessing. The HPI is intended to inform those caring for a patient. It’s not a mystery story that only you know the answer to. (It’s quite possible that you only got the history from the ER record and they were the ones who failed to describe things clearly. In that case, you need to call them up or go talk with them. The record must be clarified.) The statement about the absence of dyspnea, etc., is very good, since we want to be sure she didn’t aspirate. Don’t write the PMH in the first sentence. Her HTN has nothing to do with this problem, so it shouldn’t even be mentioned here. That’s what the PMH is for. The seizure history is possibly relevant, since she might have choked while having a seizure. That’s why I included it at the end. The degree of control is based on the presence or absence of seizures, not whether she comes to the clinic regularly, so that information should be noted, as well as whether there was any evidence of seizure activity. The sudden bleeding sounds as if it might have been due to trauma from the foreign body and or the therapeutic procedure. Periumbilical pain is fairly non-specific sign of visceral pain, but I don’t know that it would be caused by damage to the esophagus. Esophageal perforation usually causes immediate, severe pain, which isn’t mentioned here. Another possibility is a Mallory-Weiss tear, particularly if she had a lot of retching before the impaction was relieved. According to Sleisenger & Fordtran's Gastrointestinal and Liver Disease, “Violent vomiting can even tear the short gastric arteries and result in shock with hemoperitoneum.” (p 128) English: miss swallowed: This term does not exist in English. It is a direct translation from Chinese but should not be used in English. Instead, say “mistakenly” or “accidentally” if it was accidental. If intentional, e.g., a suicide attempt, we’d simply say “swallowed.” regularly followed up and well control: “was regularly followed with good control” You don’t need the preposition “up” when using “follow” as a verb. “Well” is an adverb that should modify verbs, not nouns. The correct phrase is “good control.” (Note, however, as mentioned above, that you shouldn’t use this phrase at all unless you know that the control really was good, e.g., normal BP and no seizures.) dyspnea, short of breath: dyspnea = shortness of breath. These are exactly equivalent terms, so use one or the other, not both. Also, note that “short of breath” is an adjective that would be used to describe a patient. “Shortness of breath” is a noun, the name of the symptom. esophagus of the neck. This is usually called the “cervical esophagus” and is a common site of impaction. NG tube was setting: “an NG tube was inserted” or “placed” We don’t use the verb “set” for things that are inserted. flash blood from NG tube: I assume you mean there was the sudden appearance of blood in the NG tube, but the phrase “flash blood” is not used and it really doesn’t communicate clearly.