Amendments Date Page(s) Comments Approved by 20/04/12 6
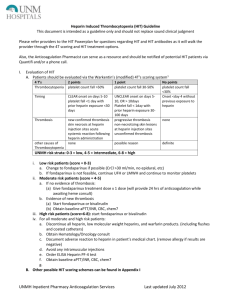
advertisement
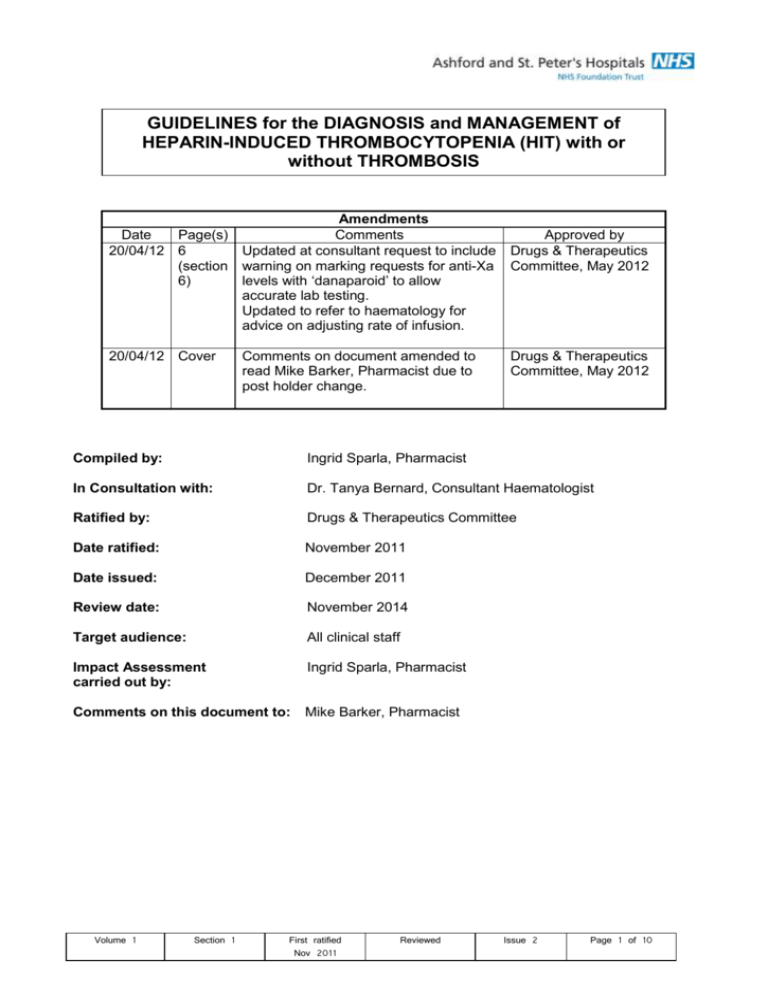
GUIDELINES for the DIAGNOSIS and MANAGEMENT of HEPARIN-INDUCED THROMBOCYTOPENIA (HIT) with or without THROMBOSIS Amendments Date Page(s) Comments 20/04/12 6 Updated at consultant request to include (section warning on marking requests for anti-Xa 6) levels with ‘danaparoid’ to allow accurate lab testing. Updated to refer to haematology for advice on adjusting rate of infusion. 20/04/12 Cover Comments on document amended to read Mike Barker, Pharmacist due to post holder change. Approved by Drugs & Therapeutics Committee, May 2012 Drugs & Therapeutics Committee, May 2012 Compiled by: Ingrid Sparla, Pharmacist In Consultation with: Dr. Tanya Bernard, Consultant Haematologist Ratified by: Drugs & Therapeutics Committee Date ratified: November 2011 Date issued: December 2011 Review date: November 2014 Target audience: All clinical staff Impact Assessment carried out by: Ingrid Sparla, Pharmacist Comments on this document to: Mike Barker, Pharmacist Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 1 of 10 INTRODUCTION Heparin induced thrombocytopenia (HIT) is an important complication of the use of heparins. HIT is an antibody-mediated adverse effect of heparin and associated with a prothrombotic state which presents with either asymptomatic thrombocytopenia, with venous or arterial thrombosis, skin lesions or rarely with a generalised systemic reaction which can be severe or even fatal. It is therefore important that HIT is recognised as early as possible and managed appropriately. PURPOSE These guidelines have been developed to assist clinical and nursing staff in the diagnosis and management of heparin induced thrombocytopenia (HIT). RESPONSIBILITIES The clinical team looking after a patient is responsible for ensuring that in consultation with the haematologists heparin-induced thrombocytopenia is diagnosed and managed appropriately and that they are familiar with these guidelines. Staff involved in the prescribing, preparation, storage and administration of danaparoid for the treatment of HIT are responsible for ensuring that they are familiar with these guidelines. In particular: - The clinical team is responsible for ensuring that no contraindications to danaparoid apply, that a valid and correct prescription for danaparoid is available for the duration of treatment, that a baseline coagulation screen and a full blood count have been sent prior to commencing danaparoid, and that plasma anti-Xa activity is monitored and the dose of danaparoid adjusted accordingly as outlined in these guidelines. - The nursing staff looking after a patient prescribed danaparoid is responsible for ensuring that danaparoid is ordered from pharmacy as soon as possible to avoid delay in treatment, and that loading dose and maintenance dose are prepared and administered as outlined in these guidelines. - Pharmacy is responsible for ensuring that danaparoid is made available to the patient as soon as possible to avoid delay in treatment. DISSEMINATION AND IMPLEMENTATION The guidelines are available on the trust intranet. PROCESS FOR MONITORING COMPLIANCE WITH THE EFFECTIVENESS OF POLICIES Through observation and audit CORE EQUALITY IMPACT ASSESSMENT See Appendix 1 ARCHIVING ARRANGEMENTS This is a trust-wide document and archiving arrangements are managed by Quality Department who can be contacted to request master/archived copies. Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 2 of 10 INCIDENCE OF HEPARIN-INDUCED THROMBOCYTOPENIA HIT may occur in any patient who is receiving Unfractionated Heparin (UFH) or Low Molecular Weight Heparin (LMWH). LMWH are associated with a lower incidence of HIT than UFH. The incidence of HIT is higher in surgical patients than it is in medical patients and obstetric patients. The highest incidence is in patients who have undergone major lower limb orthopaedic surgery and cardiac surgery. The highest risk of HIT is in days 5-10 of exposure. Occasionally, the onset can occur after more than 10 days of heparin exposure but it is rare after 15 days. Recently exposed patients (within previous 100 days) may develop HIT within the first 24 hours of re-exposure because of preexisting antibodies. 50% of patients who develop HIT will have associated thrombosis. However, in those presenting without thrombosis (isolated HIT) there is a high risk of subsequent thrombosis if heparin is not stopped and an alternative anticoagulant given. MONITORING OF PLATELET COUNT The following recommendations apply: All patients who are to receive heparin of any sort should have a platelet count on the day of starting treatment. For patients who have been exposed to heparin in the last 100 days, a baseline platelet count and a platelet count 24 hours after starting heparin should be obtained. For all patients receiving UFH, alternate day platelet counts should be performed from days 4 to 14. For surgical and medical patients receiving LMWH platelet counts should be performed every 2–4 days from days 4 to 14. Obstetric patients receiving treatment doses of LMWH should have platelet counts performed every 2–4 days from days 4 to 14. Obstetric patients receiving prophylactic LMWH are at low risk and do not need routine platelet monitoring. DIAGNOSIS OF HEPARIN-INDUCED THROMBOCYTOPENIA The diagnosis of HIT is based on the presence of a combination of clinical and laboratory features. If the platelet count falls by 50% or more, or falls below the laboratory normal range and/or the patient develops new thrombosis or skin allergy between days 4 and 14 of heparin administration HIT should be considered and a clinical assessment made to estimate the pretest probability of HIT using the scoring system below. Points (0,1 or 2 for each categories: maximum possible score = 8) ‘The 4T’s’ 2 Thrombocytopenia (NB: severe thrombocytopenia (platelet <15x109/l) is unusual in HIT) Timing of platelet count fall or other sequelae (first day of heparin exposure considered day 0) Volume 1 Section 1 1 >50% fall or platelet nadir 20-100x109/l Clear onset between days 5 and 10; or less than 1 day if heparin exposure within past 100 days First ratified Nov 2011 0 30-50% fall or platelet nadir 10-19x109/l Consistent with immunisation but not clear (e.g. missing platelet counts) or onset of thrombocytopenia after day 10 Reviewed Issue 2 <30% fall or platelet nadir <10x109/l Platelet count fall too early (without recent heparin exposure) Page 3 of 10 Thrombosis or other sequelae (e.g. skin lesions) Other causes for thrombocytopenia not evident New thrombosis; skin necrosis; post heparin bolus acute systemic reaction No other cause for platelet count fall evident Progressive or recurrent thrombosis; erythematous skin lesions, suspected thrombosis not yet proven None Possible other cause is evident Definite other cause is present Pretest probability score: 6-8 = high probability of HIT 4-5 = intermediate probability of HIT 0-3 = low probability of HIT If the pretest probability of HIT is intermediate or high, heparin should be stopped and an alternative anticoagulant started at therapeutic dosage (unless there are significant contraindications) while laboratory tests to detect the anti-heparin/anti-platelet factor 4 (PF4) antibodies are performed. Documentation of the occurrence of HIT in clinical records is essential and the diagnosis of HIT should be marked as a serious allergy. TREATMENT OF HEPARIN-INDUCED THROMBOCYTOPENIA In patients with HIT, alternative anticoagulation should be provided irrespective of whether or not there is evidence of a new thrombotic event unless the risk of haemorrhage is deemed excessive. For patients with strongly suspected or confirmed HIT, heparin should be stopped and full-dose anticoagulation with danaparoid (Orgaran®) commenced (in the absence of a significant contraindication). Platelet transfusion should generally be avoided in HIT as this can drive the thrombotic process and precipitate or exacerbate arteriovenous thromboemboli. Discuss with haematologist on call if severe/life-threatening bleeding occurs. IV DANAPAROID INFUSION REGIMEN 1. General aspects Danaparoid is given by intravenous injection followed by an intravenous infusion. Ensure that a valid IV danaparoid infusion prescription (loading and maintenance dose) is available for the duration of treatment. Ensure that a baseline coagulation screen and a full blood count have been sent prior to commencing IV danaparoid. Danaparoid is available in ampoules containing danaparoid 750 units in 0.6ml. 2. Contraindications to danaparoid As with heparins, in patients receiving danaparoid for treatment rather than for prophylaxis, spinal or epidural anaesthesia in elective surgical procedures is contra-indicated severe haemorrhagic diathesis, e.g. haemophilia and idiopathic thrombocytopenic purpura, unless the patient also has HIT and no alternative anti-thrombotic treatment is available haemorrhagic stroke in the acute phase uncontrollable active bleeding state Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 4 of 10 severe hypertension active gastroduodenal ulcer, unless it is the reason for operation diabetic retinopathy (relative contraindication) acute bacterial endocarditis hypersensitivity to danaparoid hypersensitivity to sulphite 3. Warnings and Precautions Danaparoid has been shown to have a low incidence (<10%) of (platelet) cross-reactivity with plasma from patients sensitised by heparin. Although the risk of antibody-induced thrombocytopenia is very small, it is advisable to check the number of platelets regularly. If antibody-induced thrombocytopenia occurs, one should stop the use of danaparoid and consider alternative treatment dependant on availability. For further or more detailed information please refer to the SPC of danaparoid (Orgaran®), www.medicines.org 4. Preparation of danaparoid IV bolus injection and IV infusion IV bolus injection (loading dose) The dose can be given neat or may be diluted with sodium chloride 0.9%, give over 15-30 seconds. IV infusion (maintenance dose) Make up a syringe with 4500 units (3.6ml) danaparoid (= six ampoules of 750 units/0.6ml) plus 41.4 ml of normal saline 0.9% or dextrose 5% to a total volume of 45ml. The final concentration is 100 units/ml. The syringe must be changed every 24 hours and infusion set every 72 hours. 5. Dosage and Administration Danaparoid is given by intravenous injection (loading dose) followed by an intravenous infusion (maintenance dose) as per table below: Renal function Normal to mildly impaired (CrCl 2050 ml/min) renal function Moderately (CrCl 10-20 ml/min) and severely impaired (CrCl <10 ml/min) renal function Volume 1 Loading dose (IV bolus over 15-30 sec) < 55kg: 1250 units (1ml) 55- 90kg: 2500 units (2ml) > 90kg: 3750 units (3ml) < 55kg: 1250 units (1ml) 55- 90kg: 2500 units (2ml) > 90kg: 3750 units (3ml) Section 1 First ratified Nov 2011 Maintenance dose (IV infusion) 400 units/hr for 2 hrs, then 300 units/hr for 2 hrs, followed by an initial maintenance infusion of 200 units/hr 400 units/hr for 2 hrs, then 300 units/hr for 2 hrs, followed by an initial maintenance infusion of 150 units/hr Reviewed Issue 2 Monitoring Monitoring of plasma anti-Xa activity not necessary unless patients are > 90kg Monitoring of plasma anti-Xa activity is advised for all patients, adjust maintenance dose according to anti-Xa levels (target level: 0.5-0.8 units/ml) Page 5 of 10 Patients on CVVH (Intensive Care Unit only) < 55kg: 2000 units (1.6ml) 400 units/hr for 4 hrs followed by a maintenance infusion of 150-400 units/hr to maintain plasma anti-Xa levels of 0.5-1.0 units/ml 55kg: 2500 units (2ml) 600 units/hr for 4 hrs, then 400 units/hr for 4 hrs, followed by a maintenance infusion of 200-600units/hr to maintain plasma anti-Xa levels of 0.5-1.0 units/ml Monitoring of plasma anti-Xa activity is advised for all patients, adjust maintenance dose according to anti-Xa levels 6. Monitoring of anti-Xa levels Anti-Xa levels should be monitored in the following patient groups: patients weighing > 90kg patients with moderate (CrCl 10-20ml/min) to severe (CrCl <10ml/min) renal impairment patients receiving continuous venous-venous haemofiltration (CVVH) However, lack of availability of anti-Xa monitoring is NOT a contraindication to use of danaparoid. NOTE: Anti-Xa levels for patients on danaparoid are measured in a different way to those corresponding to low-molecular weight heparins. *The request form MUST be marked ‘danaparoid anti-Xa’ for the laboratory to process the samples correctly* If it is unclear whether levels have been correctly ordered please confirm with the haematology laboratory (3038) before interpretation. Anti-Xa factor levels should be initially measured soon after completion of the accelerated infusion protocol, thereafter every 24 hours. Target plasma anti-Xa levels during the maintenance infusion are 0.5-0.8 units/ml. In patients on CVVH (Intensive Care Unit only) target plasma anti-Xa levels are 0.5-1.0 units/ml. Plasma anti-Xa levels are linearly related to the dose of danaparoid given, contact haematology for advice on adjusting the infusion rate if out of range. 7. Duration of danaparoid therapy and initiation of warfarin The duration of danaparoid therapy and the subsequent use of oral anticoagulants depend on whether the patient has had a thrombotic event. For patients with isolated thrombocytopenia, therapeutic doses of danaparoid are recommended until the platelet counts recover to a stable plateau, if not to baseline values. Warfarin can increase the risk of microvascular thrombosis in HIT and its introduction should be delayed until there has been substantial resolution of the thrombocytopenia. It should then be introduced at low dose and with overlap of danaparoid until the INR is therapeutic for two consecutive days. Please discuss with haematologist duration of therapy and potential initiation of oral anticoagulants. Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 6 of 10 REFERENCES 1. David Keeling, Simon Davidson and Henry Watson, on behalf of the Haemostasis and Thrombosis Task Force of the British Committee for Standards in Haematolgy: The management of heparininduced thrombocytopenia. British Society for Haematology, 133, 259–269, 2006 2. Warkentin TE, Greinacher A, Koster A, Lincoff AM. Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008 Jun;133 (6 Suppl): 340S-80S. 3. SIGN: Prevention and management of venous thromboembolism, Clinical guideline No 122, December 2010 4. JPJ Wester, on behalf of the NVIC Committee Nephrology and Intensive Care Medicine: Guidelines for anticoagulation with danaparoid sodium and lepirudin in continuous venovenus hemofiltration. Neth J Crit Care. 2001: 8(4): 293-301 5. Y. Sakr. Heparin-induced thrombocytopenia in the ICU: an overview. Critical Care 2011, 15:211 6. G. M. Arepally and T. L. Ortel. Heparin-Induced Thrombocytopenia. NEJM 2006; 355 (8): 809-819 7. BNF 62, September 2011 8. New Zealand data sheet of Orgaran, http://www.medsafe.govt.nz/profs/datasheet/o/Orgaraninj.pdf (accessed 11/10/11) 9. SPC of Orgaran, www.medicines.org.uk (accessed 12/10/11) 10. Medusa Injectable Medicines Guide, http://medusa.wales.nhs.uk/ (accessed 12/10/11) APPENDICES APPENDIX 1 Equality Impact Assessment Summary Name of author: Ingrid Sparla Policy/Service: Guidelines for the diagnosis and management of heparin-induced thrombocytopenia (HIT) with or without thrombosis Background Description of the aims of the policy Context in which the policy operates Who was involved in the Equality Impact Assessment The aim of these guidelines is to support and guide clinical staff (doctors, nurses and pharmacists) in the diagnosis and treatment of HIT in adult inpatients. They are intended to be used on advice/after discussion with the consultant haematologists. These guidelines should be accessible for clinical staff at any time on the intranet. This equality impact assessment has been carried out by me. Methodology A brief account of how the likely effects of the policy was assessed (to include race and ethnic origin, disability, gender, culture, religion or belief, sexual orientation, age) The data sources and any other information used The consultation that was carried out (who, why and how?) These guidelines are not discriminatory in any way but are for patients with heparin-induced thrombocytopenia irrelevant of race / gender / belief /age etc. The data sources are from national and international guidelines, medical journals and websites related to medicines (see references) Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 7 of 10 Consultation was carried out with Consultant Haematologist Tanya Bernard via email and in meetings. Key Findings Describe the results of the assessment Identify if there is adverse or a potentially adverse impacts for any equalities groups I do not feel that these guidelines have any discriminatory factors or potentially adverse outcomes for any equalities groups. Conclusion Provide a summary of the overall conclusions These guidelines are aimed at supplying summarised guidance to clinical staff involved in the management of patients with heparin-induced thrombocytopenia. No equality groups are adversely impacted as a result of these guidelines. Recommendations State recommended changes to the proposed policy as a result of the impact assessment Where it has not been possible to amend the policy, provide the detail of any actions that have been identified Describe the plans for reviewing the assessment No changes to guidelines required Guidance on Equalities Groups Race and Ethnic origin (includes gypsies and travellers) (consider communication, access to information on services and employment, and ease of access to services and employment) Religion or belief (include dress, individual care needs, family relationships, dietary requirements and spiritual needs for consideration) Disability (consider communication issues, access to employment and services, whether individual care needs are being met and whether the policy promotes the involvement of disabled people) Sexual orientation including lesbian, gay and bisexual people (consider whether the policy/service promotes a culture of openness and takes account of individual needs Gender (consider care needs and employment issues, identify and remove or justify terms which are gender specific) Age (consider any barriers to accessing services or employment, identify and remove or justify terms which could be ageist, for example, using titles of senior or junior) Social class (consider ability to access services and information, for example, is information provided in plain English?) Culture (consider dietary requirements, family relationships and individual care needs) Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 8 of 10 APPENDIX 2 PROFORMA FOR RATIFICATION OF POLICIES PROCEDURES and GUIDELINES BY RATIFYING COMMITTEE Name of Person completing form: Date: Guidelines for the diagnosis and management of heparin-induced thrombocytopenia (HIT) with or without thrombosis Ingrid Sparla 12/11/2011 Author(s) (Principle contact) Ingrid Sparla Name of author or sponsor to attend ratifying committee when policy/guideline is discussed Ingrid Sparla and Tanya Bernard Date of final draft 13/11/2011 Policy/Guidelines Name: Has this policy/guideline been thoroughly proofread to check for errors in spelling, typing, grammar and consistency? (delete as necessary) By whom: Is this a new or revised policy/guideline? (delete as necessary) Describe the development process used to generate this policy/guideline. Who was involved, which groups met, how often etc.? Who is the policy/guideline primarily for? Is this policy/guideline relevant across the Trust or in limited areas? How will the information be disseminated and how will you ensure that relevant staff are aware of this policy/guideline? Describe the process by which adherence to this policy/guideline will be monitored. (This needs to be explicit and documented for example audit, survey, questionnaire) Is there a NICE or other national guideline relevant to this topic? If so, which one and how does it relate to this policy/guideline? Has the policy been checked against minimum requirements for NHS LA Standards (if applicable) What (other) information sources have been used to produce this policy/guideline? Has the policy/guideline been impact assessed with regard to disability, race, gender, age, religion, sexual orientation? Other than the authors, which other groups or individuals have been given a draft for comment?(e.g. staff, unions, human resources, finance dept., external stakeholders and service users) Which groups or individuals submitted written or verbal comments on earlier drafts? Who considered those comments and to what extent have they been incorporated into the final draft? Have financial implications been considered? Proposed review date Volume 1 Section 1 First ratified Nov 2011 Yes Ingrid Sparla, Tanya Bernard New Peer discussion via UKCPA with pharmacists at other NHS Hospitals Local discussion with Consultant Haematologist Tanya Bernard. All clinical staff In all adult areas across the trust The guidelines will be available on the Intranet An announcement via Aspire will ensure that relevant staff are aware of them The haematologists will direct doctors to these guidelines when a HIT case is discussed. Through audit See reference 1. The national guidelines were used as a reference to compile these local guidelines N/A See ‘references’ for information sources used, also communication with pharmacists at other trusts Yes – see core EIA Consultant Haematologists Consultant Haematologist Tanya Bernard The author considered all previous comments, they all have been incorporated into the final draft Yes 3 years from ratification Reviewed Issue 2 Page 9 of 10 Volume 1 Section 1 First ratified Nov 2011 Reviewed Issue 2 Page 10 of 10