Heparin Induced Thrombocytopenia (HIT) Guideline
advertisement

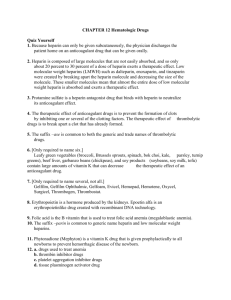
Heparin Induced Thrombocytopenia (HIT) Guideline This document is intended as a guideline only and should not replace sound clinical judgment Please refer providers to the HIT Powerplan for questions regarding HIT and HIT antibodies as it will walk the provider through the 4T scoring and HIT treatment options. Also, the Anticoagulation Pharmacist can serve as a resource and should be notified of potential HIT patients via Quantifi and/or a phone call. I. Evaluation of HIT A. Patients should be evaluated via the Warkentin’s (modified) 4T’s scoring system1 4 T’s Thrombocytopenia 2 points platelet count fall >50% 1 point platelet count fall 30-50% Timing CLEAR onset on days 5-10 platelet fall <1 day with prior heparin exposure <30 days Thrombosis new confirmed thrombosis skin necrosis at heparin injection sites acute systemic reaction following heparin administration none UNCLEAR onset on days 510, OR > 10days Platelet fall < 1day with prior heparin exposure 30100 days progressive thrombosis non-necrotizing skin lesions at heparin injection sites unconfirmed thrombosis other causes of Thrombocytopenia possible reason No points platelet count fall <30% Onset <day 4 without previous exposure to heparin none definite UNMH risk strata: 0-3 = low, 4-5 = intermediate, 6-8 = high i. Low risk patients (score = 0-3) a. Change to fondaparinux if possible (CrCl >30 ml/min, no epidural, etc) b. If fondaparinux is not feasible, continue UFH or LMWH and continue to monitor platelets ii. Moderate risk patients (score = 4-5) a. If no evidence of thrombosis: (a) Give fondaparinux treatment dose x 1 dose (will provide 24 hrs of anticoagulation while awaiting heme consult) b. Evidence of new thrombosis (a) Start fondaparinux or bivalirudin (b) Obtain baseline aPTT/INR, CBC, chem7 iii. High risk patients (score=6-8): start fondaparinux or bivalirudin iv. For all moderate and high risk patients: a. Discontinue all heparin, low molecular weight heparins, and warfarin products. (including flushes and coated catheters) b. Obtain Hematology/Oncology consult c. Document adverse reaction to heparin in patient’s medical chart. (remove allergy if results are negative) d. Avoid any intramuscular injections e. Order ELISA Heparin PF-4 test f. Obtain baseline aPTT/INR, CBC, chem7 g. B. Other possible HIT scoring schemes can be found in Appendix I UNMH Inpatient Pharmacy Anticoagulation Services Last updated July 2012 II. Laboratory evaluation of HIT A. ELISA i. Available at TriCore, run Monday, Wednesday and Friday afternoons with results available late afternoon ii. Test is very sensitive but non-specific – If positive, patient may have HIT but test cannot confirm diagnosis. B. SRA (Serotonin Release Assay) i. Send out test, returns in approximately 7-10 days ii. Test is very specific for HIT – if positive it will confirm diagnosis, if negative patient unlikely to have HIT III. Drug therapy for HIT A. Do not wait for HIT panel confirmation prior to starting therapy B. Orders for patients with suspected HIT should be entered under the HIT Powerplan C. Fondaparinux i. Considerations: a. Will not break down active clots, therefore patients with active clots may need to be switched to bivalirudin. This determination should be made by hematology b. Contraindicated if CrCl<30 ml/min (beyond 1x dose) or if spinal or epidural anesthesia ii. Treatment dosing: ≤ 50 kg use 5 mg SubQ daily 75-100 kg use 7.5 mg SubQ daily ≥ 100 kg use 10 mg SubQ daily Prophylactic dosing: 2.5 mg SubQ daily iii. Monitoring: Chem7 daily, CBC D. Bivalirudin (***Only formulary direct thrombin inhibitor***) i. Considerations: a. Shortest elimination half-life of DTI’s (a) Eliminated via blood proteases, thus less dependent on renal or hepatic elimination (b) Mainly renally cleared, but can be dose adjusted (i) t½ of bivalirudin increases as CrCl decreases b. Least expensive DTI c. If patient has had epidural/intrathecal/spinal procedure, consult with anesthesia prior to starting anticoagulation ii. Initial dosing: a. CrCl >60 ml/min: 0.15 mg/kg/hr b. CrCl 30-60 ml/min: 0.08 mg/kg/hr c. CrCl < 30 ml/min: 0.05 mg/kg/hr d. Dialysis: 0.02 mg/kg/hr iii. Monitoring: a. aPTT (a) 2 hours after initiation or resumption of infusion (b) 2 hours after any dose or rate change (c) Once 2 consecutive aPTTs in range, change to qam aPTT b. Labs: daily CBC, chem7 UNMH Inpatient Pharmacy Anticoagulation Services Last updated July 2012 iv. Titration of dose: aPTT (seconds) <45 45-75 (1.5-2.5x mean normal) >75 Dose adjustment Increase rate by 20% Calculation New rate= current rate x 1.2 AT GOAL= NO CHANGE Hold infusion for 1 hour then restart at 50% less than previous rate New rate= current rate x 0.5 IV. Long-term anticoagulation A. Warfarin should not be Initiated until platelets recover to baseline or after platelets are >150,000 B. Recommended treatment duration (not based on strong evidence, usually recommended by Hematology) i. If no thrombotic event: 1-3 months ii. If thrombotic event: 3-6 months C. Collaborative practice with Hematology i. Hematology should write at least 1 clinical note delineating duration and appropriateness of therapy ii. Thereafter, they may choose to sign off and turn dosing of medications over the anticoagulation service. Please direct providers to use the HIT Powerplan in Powerchart. Educational inservice may be required. Document originated by: Pree Sarangarm, PharmD Reviewed by: David Garcia, MD; Richard D’Angio, PharmD; Allison Burnett, PharmD References: 1. Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost 2006; 4: 759– 65. 2. Lillo-Le Louët A, Boutouyrie P, Alhenc-Gelas M, Le Beller C, Gautier I, Aiach M, Lasne D. Diagnostic score for heparin-induced thrombocytopenia after cardiopulmonary bypass. J Thromb Haemost 2004; 2: 1882–8. 3. Cuker A, Arepally G, Crowther MA, Rice L, Datko F, Hook K, Propert KJ, Kuter DJ, Ortel TL, Konkle BA, Cines DB. The HIT Expert Probability (HEP): Score: a novel pre-test probability model for heparin-induced thrombocytopenia based on broad expert opinion. J Thromb Haemost 2010; 8:2642-50. UNMH Inpatient Pharmacy Anticoagulation Services Last updated July 2012 Appendix I: Other HIT Scoring Schemes: I. HIT Expert Probability (HEP) Score3 A. Has not been prospectively validated and is not yet recommended for clinical use Clinical Feature Presentation Score Magnitude of fall in platelet count < 30% -1 (measured from peak to nadir since 30-50% +1 heparin exposure) >50% +3 Timing of fall in platelet count For patients in whom typical onset HIT is suspected: Fall begins < 4 days after heparin exposure -2 Fall begins 4 days after heparin exposure +2 Fall begins 5-10 days after heparin exposure +3 Fall begins 11-14 days after heparin exposure +2 Fall begins > 14 days after heparin exposure -1 For patients with previous heparin exposure in the last 100 days in whom rapid onset HIT is suspected: Fall begins < 48 hours after heparin exposure +2 Fall begins > 48 hours after heparin exposure -1 Nadir platelet count ≤ 20 × 109 L−1 -2 9 −1 > 20 × 10 L +2 Thrombosis For patients in whom typical onset HIT is suspected: (select no more than one) New VTE or ATE > 4 days after heparin exposure +3 Progression of pre-existing VTE/ATE while +2 receiving heparin For patients in whom rapid onset HIT is suspected: New VTE or ATE after heparin exposure +3 Progression of pre-existing VTE /ATE while +2 receiving heparin Skin necrosis Skin necrosis at subcutaneous heparin injection +3 sites Acute systemic reaction Acute systemic reaction after intravenous heparin +2 bolus Bleeding Presence of bleeding, petechiae, or extensive -1 bruising Other causes of thrombocytopenia Presence of a chronic thrombocytopenic disorder -1 (select all that apply) Newly initiation non-heparin med known to cause -2 thrombocytopenia Severe infection -2 Severe DIC (fibrinogen < 100 mg/dL and D-dimer > -2 5 mcg/ml) Indwelling intra-arterial device (IABP, VAD, ECMO) -2 Cardiopulmonary bypass within previous 96 hrs -1 No other apparent cause +3 VTE=venous thromboembolism; ATE=arterial thromboembolism; DIC=disseminated intravascular coagulation A. Score interpretation: i. Score may be interpreted 2 ways, however this will change the specificity and sensitivity. ii. > 2 = positive for HIT; < 2 = negative for HIT (Sensitivity 1.00 [0.56 – 1.00], Specificity 0.60 [0.45 - 0.75]) iii. > 5 = positive for HIT; < 5 = negative for HIT (Sensitivity 0.86 [0.42 – 0.99], Specificity 0.88 [0.74-0.96]) UNMH Inpatient Pharmacy Anticoagulation Services Last updated July 2012 II. Score for HIT in Cardiopulmonary Bypass2 Variables Clinical Scenario Platelet count time Pattern A ((Platelet count begins to recover after CPB, but then course begins to fall again > 4 days after CPB) Pattern B (Thrombocytopenia occurs immediately after CPB and persists for > 4 days without recovery) Time from CPB to index ≥5 days date <5 days CBP Duration <118 minutes ≥118 minutes A. Score interpretation: i. < 2 = low probability of HIT ii. > 2 = high probability of HIT UNMH Inpatient Pharmacy Anticoagulation Services Last updated July 2012 Points 2 1 2 0 1 0