Policy and Procedure: Opioid Pain Management-
advertisement
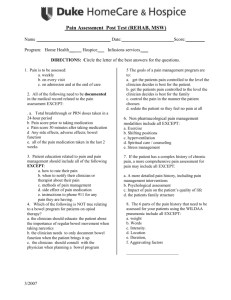
SHASTA COMMUNITY HEALTH CENTER Policy: Opioid Pain Management Procedures Effective Date: November 22, 2005 Number of Pages: 3 JCAHO Standards (if applicable): Standard RI.2.160 Standard PC 8.10 Reviewed/Approved By: Medical Directors SCHC Board of Directors I. Manual: Medical Staff Revision Date: Number of Forms: 2 Saved As: Opioid Pain Management Procedures 12.07.doc Reviewed/Approved Date: Policy: It is the policy of Shasta Community Health Center to assure appropriate clinical management of patients with chronic pain on opioid drug therapy. This policy shall apply to those utilizing opioids a majority of days in a 3 month period. II. Purpose/Goal: The purpose of this policy is to delineate clinician responsibilities, approved tools and standard documents for managing patients with chronic pain on opioid drug therapy. III. Procedure: A. Organization 1. The Pain Management Committee shall be a standing committee of the medical staff, meeting monthly, composed of up to six clinicians from various departments and the Director of Quality Improvement. 2. At least one member of the Pain Management Committee shall be from the Primary Care Neuropsychiatry Department, and at least one shall be from a satellite clinic. 3. The Pain Management Committee is charged with the following responsibilities: a. Develop clinic-wide policies regarding chronic pain management. b. Recommend, review and revise clinical tools, documentation forms and standard letters for the management of chronic pain. c. Act as a clinical resource group for clinicians in the management of chronic pain. d. Periodic audits to measure compliance, uniformity and adherence to policy 1 B. Basic Pain Management processes for clinicians: 1. At the time of the initial visit, the clinician shall see and assess the patient for chronic pain issues. A full assessment includes an appropriate systembased physical exam, appropriate diagnostic testing as indicated, a review of the past medical history, and completion of the “Brief Pain Inventory” filed in left side of chart progress notes. Other resources such as a check of the California Department of Justice CURES Program for past medication history or contacting the patient’s previous clinician may also be utilized. 2. After the assessment has been completed, the clinician shall make a decision regarding treatment of the patient based on the assessment and his/her best clinical judgment. 3. If the decision is to provide primary care and to begin or continue management of chronic pain using controlled substances, the clinician shall educate the patient regarding the practices and policies of Shasta Community Health Center, and the patient will be expected to sign a “Medication Management Agreement”. 4. In some cases, and always based on the assessment and review of documentation, the clinician may agree to provide primary care but not controlled substances, and will notify the patient of that limitation. 5. Ongoing management of chronic pain: a. At each visit, the clinician should assess the patient response to treatment, with attention to severity of pain, response to treatment, quality of sleep and potential medication side effects. b. At least once each year, the patient will be asked to provide a urine specimen for toxicology screening purposes. If the clinician has any concerns about the possibility of adulteration of the urine sample, s/he may request that a member of the nursing staff supervise while the specimen is obtained; if the patient is unable to void a catheterized specimen may be obtained with patient permission. If patient fails to comply with requested urine sample, the clinician may decline to provide opioid medication. c. Bi-annually or more frequently at clinician discretion, Brief Pain Inventory to be completed. C. Problems during the pain management process: 1. Toxicology screens positive for illegal substances or for medications that the patient has not been prescribed – the clinician has the option to stop prescribing controlled substances. In that case, the findings of the toxicology screen shall be discussed with the patient and the rationale for not prescribing explained. A letter documenting the rationale for not prescribing shall be sent to the patient and a copy placed in the medical record. 2. Behavior issues – the clinician may ask the patient to sign a behavior agreement or make a referral to the Case Review Committee. 3. Clinical management of chronic pain – the clinician may present the patient’s case to the Pain Management Committee for advice. 2 4. In all cases in which it seems the most appropriate action is to discharge the patient from SCHC, the case must be referred to Case Review Committee using the normal referral process unless the clinician believes there is a high potential risk to employees or other patients; in the latter case, a request for an expedited discharge may be requested by communicating with the chair of the Case Review Committee. IV. Forms A. Shasta Community Health Center Brief Pain Inventory B. Letter notification, “SCHC Will No Longer Prescribe You With Controlled Substance Medications.” V. VI. Written by: SCHC Pain Management Committee 11/7/05 References: A. Medical Boards of California Guidelines for Prescribing Controlled Substances for Pain. B. California Academy of Family Physicians C. Patient Activity Report (PAR) California Department of Justice form BNE 1177 (07/2003) 3