Infant_with_SVT_F1
advertisement

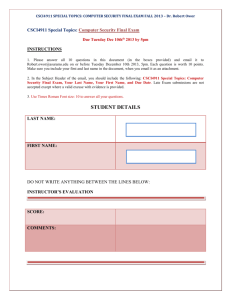
CSC Standardized Curriculum Specialty: Pediatrics Simulation: Infant with SVT Submitted by: COL Robert Puntel Target Audience: Pediatric and Family Medicine Residents, Pediatric and Family Medicine Staff ACGME Competencies Addressed: Medical Knowledge Patient Care Communication Professionalism RRC Requirements Addressed: Infant resuscitation, PALS skills, Medication delivery, IV start, IO start, synchronized cardioversion Version 1, 4/11/2008 Case Scenarios Primary: Emergency Room: 3 month old infant, previously healthy and history of term delivery, presents to the ED with parents. Chief complaint is fast breathing and poor feeding for approximately 6 to 8 hours. No history of fever, URI symptoms, cough, diarrhea or vomiting. No ill contacts. Received 2 month immunizations on time. Has been gaining weight and developing normally to date. No other medical problems. FHX is not contributory. No medications or unusual exposures. Alternate scenario: Pediatric Clinic: 3 year old, history of several similar episodes in the past, this is first time to care for this, says “heart is beeping” and has been breathing a bit fast and seems tired. This has been for about 30 minutes. No fever, cough or URI. No meds. Healthy with normal growth and development. PMHX, PSHX, ROS, FHX all noncontributory. Basic Instructions for participants: Please read the scenario and then enter the room when instructed by your staff. 1. You may ask questions if you have them, and please remember to: Treat the situation as realistically as possible. 2. Think out loud, vocalize abnormal/critical findings, state the doses of drugs, and declare differential diagnoses you are considering. Only with this behavior can we evaluate you and make sure you succeed. 3. If you have questions about the simulation or manikin ask the supervisor 4. If you need further patient information, ask; do not make assumptions; do not declare the answers/results to physical finding/labs without asking 5. Assume that you can request any resource you would have available in the hospital in which you are training Version 1, 4/11/2008 2 Simulation Setup: Simulators to be used: SimBaby or child mannequin Room Setup: SimBaby or child mannequin with monitor on table, crib or warmer, stethoscope, oxygen mask and infant and pediatric nasal canulae Additional Equipment needed 24 and 22 gauge IV catheters, IV extension tubing, 500 cc NS, tape, pediatric intraosseus needle, defibrillator/cardioverter, Infant and child size Zoll pads, monitor leads, 5cc syringe, 3 cc syringe, 1 cc syringe, 3 way stop cock, 23 gauge needle, Adenocard 6 mg vial (sham) Optional Equipment: Bag-valve mask, ET tubes infant sizes: 3.5 and 4.0, child sizes 4.5 and 5.0, laryngoscope, stylet, tape Personnel needed: SimBaby trained technician and scenario instructor, can be run with 1 instructor trained on SimBaby Basic Scenario Tips: Initial presentation in both scenarios is stable patient with normal BP. General appearance is moderately tachypneic, but no respiratory distress, and minimal if any decrease in capillary refill. Learners should progress through vagal maneuvers, then adenosine administration. If there is delay in management, patient should become progressively less well perfused and less interactive, decreasing BP and require synchronized cardioversion to terminate the arrhythmia. Version 1, 4/11/2008 3 Case Flow/Algorithm with branch point and completion criteria: Primary scenario: General Appearance: 3 month old, nondysmorphic, mildly fussy, mildly pale, consolable briefly Vital signs: Temp: 36.5. Resp rate: 70, no distress. O2 sat: 94%. Pulses: 274. BP (right arm): 70/54. Weight: 6 kg. Birth Weight: 3.5 kg Exam: AF flat Mucous membranes moist. Mild nasal flaring. No grunting. Mild suprasternal and subcostal retractions. Mild tachypnea without significant distress. Auscultation: Lungs are overall clear, no wheezing Cor: hyperdynamic, soft nonspecific 1/6 systolic murmur at LUSB Liver is 2 cm below the right costal margin Pulses in the brachial and femoral are all equal but mildly, too fast to count Capillary refill is 3 seconds Skin is cool without petechiae or rash Case Flow: Stable infant in SVT 1. Initial assessment: Airway and breathing are stable, O2 can be administered by NC or blow by Circulation: Stable SVT should be verbalized. Initial interventions: Vagal maneuvers (Ice bag to face and neck for 10 to 15 seconds, do not occlude airway) should be attempted. SVT persists, so adenosine is indicated. Secure IV access, preferably in a larger vein such as antecubital vein. Dose of adenosine should be verified in text or card. Adenosine 100 mcg/kg (About 0.5 mg) should be given IV push with 3 cc NS IV push flush following immediately. This will convert rhythm to normal rhythm. 2. Scenario can continue in SVT with no effect from adenosine: Patient vital signs now change: Pulse 274, patient appears lethargic and not interactive, BP 56/34. Capillary refill 4 to 5 seconds. Synchronized cardioversion must be given. Infant Zoll pads should be applied over sternum and back. Verify defibrillator is demonstrating EKG. Choose synchronization on the defibrillator and verify visually. Dial Joules as 0.5 per kg (about 3 Joules or lowest may be 5 Joules) “Clear” patient and press deliver shock button. Patient is converted to NSR with rate 160. 3. Post resuscitation care should include warming if needed, bedside d-stick, consider 10 to 20cc/kg of IVF if history of many hours of poor feeding, consultation with pediatric cardiologist. Alternate scenario: General Appearance: 3 year old, nondysmorphic, mildly fussy but attends Vital signs: Resp rate: 30, no distress. O2 sat: 94%. Pulse 230. BP (right arm): 82/54. Weight: 15 kg. Exam: Mucous membranes moist. Mild suprasternal and subcostal retractions. Mild tachypnea without significant distress. Auscultation: Lungs are overall clear, no wheezing Cor: hyperdynamic, soft nonspecific 1/6 systolic murmur at LUSB, HR about 200 Liver is 2 cm below the right costal margin Pulses in the brachial and femoral are all equal but mildly, too fast to count Version 1, 4/11/2008 4 Capillary refill is 3 seconds Skin is cool without petechiae or rash Case Flow: Stable child in SVT 1. Initial assessment: Airway and breathing are stable, O2 can be administered by NC or blow-by Circulation: Stable SVT should be verbalized. Initial interventions: Vagal maneuvers (Bearing down, blowing through an occluded straw) should be attempted. SVT persists, so adenosine is indicated. Secure IV access, preferably in a larger vein such as antecubital vein. Dose of adenosine should be verified in text or card. Adenosine 100 mcg/kg (About 1.5 mg) should be given IV push with 5 cc NS IV push flush following immediately. This will convert rhythm to normal rhythm. 2. Scenario can continue in SVT with no effect from adenosine: Patient vital signs now change: Pulse 192, patient appears lethargic and not interactive, BP 60/40. Capillary refill 4 to 5 seconds. Synchronized cardioversion must be given. Child Zoll pads should be applied over sternum and back. Verify defibrillator is demonstrating EKG. Choose synchronization on the defibrillator and verify visually. Dial Joules as 0.5 per kg About 10 Joules) “Clear” patient and press deliver shock button. Patient is converted to NSR with rate 120. 3. Post resuscitation care should include warming if needed, bedside d-stick, consider 10 to 20cc/kg of IVF if history of many hours of poor feeding, consultation with pediatric cardiologist. Common pitfalls to monitor for: Giving an IV fluid bolus is contraindicated in the presentation of SVT. Proper administration of adenosine with a rapid NS flush must be demonstrated. Version 1, 4/11/2008 5 Evaluation Form: Physician # / Name ____________________________ Date _______________________ Training Site __________________________________ Grader __________________ Training Level: (Circle One) Fellow Staff PGY-1 PGY-2 PGY-3 Completed Not Completed Indeterminate History (3 points) Obtains relevant history (1 point) Requests full vitals (1 point) Requests continuous monitoring (1 point) Physical Exam (7 points) Notes general appearance (1 points) Recognizes tachycardia (2 points) Recognizes tachypnea (2 points) Recognizes signs of poor perfusion (2 points) Diagnostic evaluation (6 points) Categorizes as stable or unstable/shock (3 points) Appropriately diagnoses rhythm/SVT (3 points) Version 1, 4/11/2008 6 Management (13 points) Completed Not completed Indeterminate Assesses Airway, Breathing And Circulation (2 points) IV/IO demonstrated (2 points) Appropriate vagal maneuvers discussed/demonstrated (3 points) Appropriate use of Adensoine and dosage discussed/demonstrated (3 points) Appropriate use of cardioversion discussed/demonstrated (3 points) Time goals (11 points) SVT diagnosed (1:00 minute) (2 points) Vagal maneuvers (2:00 scenario time) (3points) Adenosine used (4:00 scenario time) (3 points) Cardioversion discussed/used (6:00 minutes scenario time (3 points) Contraindicated Actions and Interventions Contraindicated IVF bolus given (-3 points) Sequence of vagal maneuvers, then adenosine, then cardioversion if unstable not followed (-3 points) Defibrillation instead of cardioversion used (-3 points) Version 1, 4/11/2008 7 Scenario score: Assign points for all items checked as ‘Completed’ or ‘Contraindicated”. No points are given for “Not completed” and ‘Indeterminate’ actions. (Maximum points possible for this scenario = 40) Correct action points = _____ Contraindicated action points = _____ Total scenario points = _____ Percent scenario score (Total scenario points /40) = _____ Overall scenario performance rating: 1 (poor) 2 (fair) Version 1, 4/11/2008 3 (good) 4 (Very good) 5 (Excellent) 8 Please answer the following questions about this provider’s performance: 1. Provider performed airway evaluation in timely fashion Strongly Disagree 0 1 2 Neither agree Or disagree 3 4 5 6 Strongly Agree 7 8 9 10 2. Respiratory status exam was accurate and complete Strongly Disagree 0 1 2 Neither agree Or disagree 3 4 5 6 Strongly Agree 7 8 9 10 3. Provider initiated appropriate diagnostic evaluation in a timely fashion Strongly Disagree 0 1 2 Neither agree Or disagree 3 4 5 6 Strongly Agree 7 8 9 10 4. Provider made appropriate therapeutic decision Extremely Poor 0 1 Average 2 3 4 5 6 Outstanding 7 8 9 10 4. How prepared do you feel the provider was to manage this scenario? Not prepared at all 0 1 Reasonably prepared 2 3 4 5 6 Very prepared 7 8 9 10 Perceived competency: Not competent to handle a similar scenario on a patient even with supervision* Competent to handle a similar scenario on a patient with supervision Competent to handle a similar scenario on a patient independently Competent to teach others about this scenario * If student not competent to perform procedure please refer for remedial simulation training Version 1, 4/11/2008 9 Key Teaching Points/Critical Actions to discuss in debriefing: IVF bolus contraindicated with patient in SVT (similar to CHF patients). Adenosine dose should be looked up and not determined from memory. Adenosine must be given with a rapid 3 to 5cc NS flush following. This is best accomplished with a 3 way stopcock. Learners should demonstrate proper placement of Zoll pads on patient and discuss age differences. Synchronized cardioversion at low joules/kg (0.5 to 1 J/kg) must be used if unstable, and not defibrillation. Learners should demonstrate the use of the defibrillator to appropriately give DC cardioversion that is synchronized and not defibrillation. Suggested time length for modules: Total time: 20 minutes. 3 minute introduction to Sim Baby if not already known, auscultation and pulse points on the mannequin, 2 minute introduction to scenario, 3 minute assessment and initial plans for vagal maneuvers, flow is unsuccessful with maneuvers, 3 minutes discussion of adenosine dose and demonstration of administration with IV flush with 3 way stopcock. Zoll pad placement and synchronized cardioversion as case progresses. (5 minutes) Brief Didactic: SVT is generally well tolerated by infants and children. Some infants can present after being in SVT for 1 to 2 days and appear relatively well. IVF boluses, especially usual 20cc/kg are contraindicated in SVT. Small peripheral vein adenosine administration may not work (hand or scalp IV), intraosseus administration is very unlikely to work due to diffusion of drug through bone marrow. ET tube administration is contraindicated. Other drugs can be discussed for use in SVT such as calcium channel blockers (example: verapamil or diltiazem) but these have the significant side effect of hypotension in children and are usually avoided. Synchronized cardioversion means that the joules are delivered to avoid the T wave which could initiate ventricular fibrillation. Some vagal maneuvers in children can be coughing, gently pressing on abdomen and asking them to push back on your hand with their abdomen (valsalva), blowing upn exam glove (do not leave a child unattended with a glove as the child could choke on a piece of glove) Supporting Literature and Suggested Readings: Moss and Adams, Fifth Edition, pp 1572 to 1584. Version 1, 4/11/2008 10