Instructions for IRB submissions
advertisement

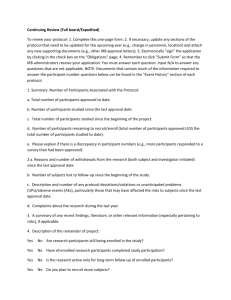
IRB APPLICATION INSTRUCTIONS The Mount Auburn Hospital Institutional Review Board (IRB) reviews protocols according to the level of risk to research subjects involved and categories of research as defined by federal regulations 45 CFR Part 46 and 21 CFR Part 50. The proposed research may present more than minimal risk to subjects (full board review), minimal risk (expedited review), or the research may qualify as exempt under specific categories 46.101(b)(1-6), 46.201(b), 46.301(a), 46.401(b), 21 CFR 50.104. The type of review will determine the research application requirements. For all protocols that involve any contact with human subjects whether through procedures, questionnaires, surveys, interviews, focus groups, sample tissue, cell lines or any material or data that may or may not be linked to human subjects, a determination must be made through the IRB office whether the proposal meets the definition of research with human subjects and whether subsequent IRB review is required. The IRB Administrator pre-reviews all application submissions and determines whether the research project meets the definition of research involving human subjects. The IRB Administrator is available to consult informally in preparation of a protocol. However, if an investigator would like to consult with the Administrator to determine whether a research project fits a specific category of research, a detailed protocol with all relevant attachments will be required. The IRB Administrator may request additional documents as necessary to make an appropriate recommendation. Please review the categories of research, expedited, full board, exempt, to determine the level of review and application submission requirements. EXPEDITED REVIEW ONLY protocols that satisfy the federal requirements for expedited review may be reviewed in a pre-meeting of the IRB as an expedited study. Expedited reviews are conducted by the IRB Co-Chairs in accordance with 45 CFR 46.110(b), the reviewer “may exercise all of the authorities of the IRB except that the reviewer may not disapprove research.” The Co-Chair may approve the application, require modifications to the application, or defer the study to the convened board for review. Expedited procedures may be used for initial and continuing review of research, and amendments to previously approved research under 45 CFR 46.110 and 21 CFR 56.110. Research activities that: 1. present no more than minimal risk to human subjects, and 2. involve only procedures listed in one or more of seven specific categories permitted by the federal regulations are eligible for expedited review. “minimal risk” is defined as the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance or routine physical or psychological examinations or tests.” Risks to subjects may include physical or psychological risks, risks associated with breach of privacy and confidentiality, risk of criminal or civil liability, or negative impact to subject’s financial standing, employability, insurability, or reputation. An expedited review application may require an informed consent form and authorization. The investigator may request a waiver of consent and waiver of authorization provided the criteria for waiver are met. LINK – Section M, Expedited Review Instructions revising expedited review form Forms required for Expedited Review: Section A - Research Application; Section B – Study Description; Section C – Medical Records Review (if not applicable do not submit); Section D – Informed Consent Form; If requesting a waiver of consent requirement, please complete Section A-12 of the application. If requesting a waiver of authorization, please complete Section A-12 of the application and submit a Waiver of Authorization Form FULL BOARD REVIEW The convened IRB may approve research only after it has determined that all of the following requirements are satisfied: 1. Risks to subjects are minimized by using procedures that are consistent with sound research design, and that do not unnecessarily expose subjects to risk. Whenever appropriate, researchers should employ procedures that are being performed on subjects for diagnostic or treatment purposes. 2. Risks to subjects are reasonable relative to 1. anticipated benefits, if any, to subjects, and 2. the importance of the knowledge that may reasonably be expected to result. 3. The selection of subjects is equitable. In making this assessment the IRB must take into account the purposes of the research and the setting in which it will be conducted. The IRB must be particularly attentive to the special problems that may arise when research involves vulnerable populations, such as children, pregnant women, prisoners, mentally disabled persons, or economically or educationally disadvantaged persons. If any of the subjects is likely to be susceptible to undue influence or coercion, the IRB may require additional safeguards in the study to protect such subjects. 4. Informed consent will be sought from each prospective subject, or the subject's legally authorized representative, generally by means of a written consent document. The IRB will carefully review these documents to assure that they contain the required elements of informed consent (see 45 CFR 46.116) and that they are understandable to a lay person. 5. The research plan makes adequate provisions for ensuring the safety of subjects. 6. There are adequate provisions to protect the privacy of subjects and to maintain the confidentiality of data. Forms required for Full Board Review: Section A - Research Application; Section B – Study Description; Section C – Medical Records Review if applicable; Section D – Informed Consent Form; If requesting a waiver of consent requirement, please complete section A-12 of the application. If requesting a waiver of authorization please complete section A-12 of the application and submit a Waiver of Authorization Form EXEMPT RESEARCH The six categories of research that qualify for exemption from ongoing IRB review are: 1. research conducted in established or commonly accepted educational settings, involving normal educational practices 2. research involving the use of educational tests, (cognitive, diagnostic, aptitude, achievement), survey procedures, interview procedures or observation of public behavior, unless: (i) information obtained is recorded in such a manner that human subjects can be identified, directly or through identifiers linked to the subjects; and (ii) any disclosure of the human subjects' responses outside the research could reasonably place the subjects at risk of criminal or civil liability or be damaging to the subjects' financial standing, employability, or reputation. 3. behavioral and social science studies that present little or no risk to participants; 4. research involving the collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available 5. research and demonstration projects which are conducted by or subject to the approval of department or agency heads, and which are designed to study, evaluate, or otherwise examine: (i) Public benefit or service programs; (ii) procedures for obtaining benefits or services under those programs; (iii) possible changes in or alternatives to those programs or procedures; or (iv) possible changes in methods or levels of payment for benefits or services under those programs. 6. taste and food quality evaluation and consumer acceptance studies Exempt research must have little, if any, associated risk. In rare circumstances, the IRB may review periodic reports on an exempt study. Forms required for Exempt Review: revising the exempt review form. The research may not begin until the IRB has issued an approval. AMENDMENTS Amendments are changes to the currently approved research application. The Mount Auburn Hospital IRB also processes and reviews as amendments recruitment materials, information sheets, advertisements, surveys/questionnaires, investigator brochures, changes to informed consent forms, partial waiver of consent requirements, and changes to study status prior to annual review. Some amendments or changes may be minor. Studies deemed to be minimal risk amendments may be reviewed by an IRB Co-Chair using the expedited review process. The IRB determines that the information or activity described in an amendment could place subjects at increased risk and, it will require that the amendment go to the full board for review. INVESTIGATORS MAY NOT INCLUDE UNAPPROVED AMENDMENT INFORMATION OR ACTIVITIES IN THE PROTOCOL OR INFORMED CONSENT FORM WITHOUT PRIOR IRB APPROVAL. If you believe that an amendment is necessary to eliminate immediate potential harm to subjects contact the IRB Co-Chair for emergency approval The PI is responsible for submitting the amendment to the IRB office with all supporting revisions and any additional information related to the amendment. The Research Administrator is responsible for reviewing and determining whether the risks to subjects is minor and, therefore can be approved through expedited review procedure. Forms required: Amendment form; if amending the informed consent form (ICF), please include a copy of the IRB approved ICF along with the revised copy; if amending any other forms, please include the original with the amended copy. CONTINUING REVIEW The timeframe for IRB continuing review is based on the level of risks to subjects [45 CFR 46.103(b)(4) and 46.109(e)] and will occur at least annually. Investigators who do not submit a continuing review before the study expiration date must stop all research activities until the IRB receives and approves the continuing review. In circumstances where risks to subjects may be compromised by halting study procedures, the investigator is required to contact the IRB Co-Chair and inform him of the reasons why the study can not be stopped, provide a written explanation to the IRB, and submit a continuing review form. Forms required for continuing review: Continuing Review Form; a copy of the IRB approved informed consent form. THIS SECTION, ADVERSE EVENTS, IS STILL UNDER REVIEW ADVERSE EVENTS & UNANTICIPATED PROBLEMS INSTRUCTIONS AND REPORTING GUIDE RELEVANT DEFINITIONS: LINK THRU TO “END OF DEFINITIONS” Serious adverse event: Any adverse event temporally associated with the subject’s participation in research that meets any of the following criteria: 1. results in death; 2. is life-threatening (places the subject at immediate risk of death from the event as it occurred); 3. requires inpatient hospitalization or prolongation of existing hospitalization; 4. results in a persistent or significant disability/incapacity; 5. results in a congenital anomaly/birth defect; or 6. any other adverse event that, based upon appropriate medical judgment, may jeopardize the subject’s health and may require medical or surgical intervention to prevent one of the other outcomes listed in this definition (examples of such events include allergic bronchospasm requiring intensive treatment in the emergency room or at home, blood dyscrasias or convulsions that do not result in inpatient hospitalization, or the development of drug dependency or drug abuse). UNEXPECTED ADVERSE EVENTS: Any adverse event occurring in one or more subjects participating in a research protocol, the nature, severity, or frequency of which is not consistent with either: The known or foreseeable risk of adverse events associated with the procedures involved in the research that are described in (a) the protocol related documents, such as the IRB-approved research protocol, any investigator brochure, and the current IRB-approved informed consent document, and (b) other relevant sources of information, such as product labeling and package inserts; or The expected natural progression of any underlying disease, disorder, or condition of the subject(s) experiencing the adverse event and the subject’s predisposing risk factor profile for the adverse event. (Modified from the definition of unexpected adverse drug experience in FDA regulations at 21 CFR 312.32(a)). External Adverse events: From the perspective of one particular institution engaged in a multi-center clinical trial, external adverse events are those adverse events experienced by subjects enrolled by investigators at other institutions engaged in the clinical trial. Internal Adverse events: From the perspective of one particular institution engaged in a multi-center clinical trial, internal adverse events are those adverse events experienced by subjects enrolled by the investigator at that institution. In the context of a single-center clinical trial, all adverse events would be considered internal adverse events. Possibly related to the research: There is a reasonable possibility that the adverse event, incident, experience or outcome may have been caused by the procedure involved in the research (modified from the definition of associated with use of the drug in FDA regulations at 21 CFR 312.32(a). END OF DEFINITIONS. WHAT ARE ADVERSE EVENTS? The term adverse event is used very broadly and includes any event meeting the following definition: Any untoward or unfavorable medical occurrence in a human subject, including any abnormal sign (for example, abnormal physical exam or laboratory finding), symptom, or disease, temporally associated with the subject’s participation in the research, whether or not considered related to the subject’s participation in the research. Adverse events may be caused by one or more of the following: 1. the procedures involved in the research; 2. an underlying disease, disorder, or condition of the subject; or 3. other circumstances unrelated to either the research or any underlying disease, disorder, or condition of the subject. WHAT ARE UNANTICIPATED PROBLEMS? Office of Human Research Protection (OHRP) considers unanticipated problems, in general, to include any incident, experience, or outcome that meets all of the following criteria: 1. unexpected (in terms of nature, severity, or frequency) given (a) the research procedures that are described in the protocolrelated documents, such as the IRB-approved research protocol and informed consent document; and (b) the characteristics of the subject population being studied; 2. related or possibly related to participation in the research (in this guidance document, possibly related means there is a reasonable possibility that the incident, experience, or outcome may have been caused by the procedures involved in the research); and 3. suggests that the research places subjects or others at a greater risk of harm (including physical, psychological, economic, or social harm) than was previously known or recognized. An incident, experience, or outcome that meets the three criteria above generally will warrant consideration of substantive changes in the research protocol or informed consent process/document or other corrective actions in order to protect the safety, welfare, or rights of subjects or others. Examples of corrective actions that might need to be considered in response to an unanticipated problem include: changes to the research protocol initiated by the investigator prior to obtaining IRB approval to eliminate apparent immediate hazards to subjects modification of inclusion or exclusion criteria to mitigate the newly identified risks; implementation of additional procedures for monitoring subjects; suspension of enrollment of new subjects; suspension of research procedures in currently enrolled subjects; modification of informed consent documents to include a description of newly recognized risks; and provision of additional information about newly recognized risks to previously enrolled subjects. EXAMPLES OF UNANTICIPATED PROBLEMS THAT DO NOT INVOLVE ADVERSE EVENTS AND NEED TO BE REPORTED TO THE IRB 1. As a result of a processing error by a pharmacy technician, a subject enrolled in a multi-center clinical trial receives a dose of an experimental agent that is 10-times higher than the dose dictated by the IRB-approved protocol. While the dosing error increased the risk of toxic manifestations of the experimental agent, the subject experienced o detectable harm or adverse effect after an appropriate period of careful observation. Nevertheless, this constitutes an unanticipated problem for the institution where the dosing error occurred that must be reported to the IRB, appropriate institutional officials, and OHRP because the incident was (a) unexpected; (b) related to participation in the research; and (c) placed subject at a greater risk of physical harm than was previously known or recognized. 2. Subjects with cancer are enrolled in a phase 2 clinical trial evaluating an investigational biologic product derived from human sera. After several subjects are enrolled and receive the investigational product, a study audit reveals that the investigational product administered to subjects was obtained from donors who were not appropriately screened and tested for several potential viral contaminants, including the human immunodeficiency virus and the hepatitis B virus. This constitutes an unanticipated problem that must be reported because the incident was (a) unexpected; (b) related to participation in the research; and (c) placed subjects and others at a greater risk of physical harm than was previously known or recognized. This unanticipated problem example may have presented unanticipated risks to others (e.g., the sexual partners of the subjects) in addition to the subjects and should be promptly reported to the IRB, appropriate institutional officials, and the OHRP in accordance with HHS regulations at 45 CFR 46.103(a) and 46.103(b)(5). 3. An investigator conducting behavioral research collects individually identifiable sensitive information about illicit drug use and other illegal behaviors by surveying college students. The data are stored on a laptop computer without encryption, and the laptop computer is stolen from the investigator’s car on the way home from work. This is an unanticipated problem that must be reported to the IRB, appropriate institutional officials, and the OHRP in accordance with HHS regulations at 45 CFR 46.103(a) and 46.103(b)(5) because the incident was (a) unexpected (i.e., the investigators did not anticipate the theft); (b) related to participation in the research; and (c) placed the subjects at a greater risk of psychological and social harm from the breach of confidentiality of the study data than was previously known or recognized. UNANTICIPATED PROBLEMS MAY REQUIRE SUBSTANTIVE CHANGES IN THE RESEARCH PROTOCOL OR INFORMED CONSENT PROCESS/DOCUMENT OR OTHER CORRECTIVE ACTIONS IN ORDER TO PROTECT THE SAFETY, WELFARE, OR RIGHTS OF SUBJECTS. END OF LINK #1 EXAMPLES OF UNANTICIPATED PROBLEMS LOCAL ADVERSE EVENT REPORTS - SUBMISSION INSTRUCTIONS: Complete the ADVERSE EVENT REPORT FORM with original PI signature Signature of responsible treating physician, if different from the PI Include supporting Medical reports Discharge summary, if applicable If revising informed consent form, include: o Revised ICF with changes highlighted o 1 clean copy of revised ICF EXAMPLES OF ADVERSE EVENTS THAT REPRESENT UNANTICIPATED PROBLEMS AND NEED TO BE REPORTED UNDER THE HHS REGULATIONS AT 45 CFR PART 46 1. A behavioral researcher conducts a study in college students that involves completion of a detailed survey asking questions about early childhood experiences. The research was judged to involve no more than minimal risk and was approved by the IRB chairperson under an expedited review procedure. During the completion of the survey, one student subject has a transient psychological reaction manifested by intense sadness and depressed mood that resolved without intervention after a few hours. The protocol and informed consent document did not describe any risk of such negative psychological reactions. Upon further evaluation, the investigator determines that the subject’s negative psychological reaction resulted from certain survey questions that triggered repressed memories of physical abuse as a child. The investigator had not expected that such reactions would be triggered by the survey questions. This is an example of an unanticipated problem that must be reported in the context of social and behavioral research because, though not serious, the adverse event was (a) unexpected; (b) related to participation in the research; and (c) suggested that the research places subjects at a greater risk of psychological harm than was previously known or recognized. 2. Subjects with essential hypertension are enrolled in a phase 2, non-randomized clinical trial testing a new investigational antihypertensive drug. At the time the clinical trial is initiated, there is no documented evidence of gastroesophageal reflux disease (GERD) associated with the investigational drug, and the IRB approved protocol and informed consent document do not describe GERD as a risk of the research. Three of the first ten subjects are noted by the investigator to have severe GERD symptoms that began within one week of starting the investigational drug and resolved a few days after the drug was discontinued. The investigator determines that the GERD symptoms were most likely caused by the investigational drug and warrant modification of the informed consent document to include a description of GERD as a risk of the research. This is an example of an adverse event that, although not serious, represents an unanticipated problem that must be reported because it was (a) unexpected in nature; (b) possibly related to participation in the research; and (c) suggested that the research placed subjects at a greater risk of physical harm than was previously known or recognized. 3. The fifth subject enrolled in a phase 2, open label, uncontrolled clinical study evaluating the safety and efficacy of a new oral agent administered daily for treatment of severe psoriasis unresponsive to FDA-approved treatments, develops severe hepatic failure complicated by encephalopathy one month after starting the oral agent. The known risk profile of the new oral agent prior to this event included mild elevation of serum liver enzymes in 10% of subjects receiving the agent during previous clinical studies, but there was no other history of subjects developing clinically significant liver disease. The IRB-approved protocol and informed consent document for the study identifies mild liver injury as a risk of the research. The investigators identify no other etiology for the liver failure in this subject and attribute it to the study agent. This is an example of an unanticipated problem that must be reported because although the risk of mild liver injury was foreseen, severe liver injury resulting in hepatic failure was (a) unexpected in severity; (b) possibly related to participation in the research; and (c) serious. EXAMPLES OF ADVERSE EVENTS THAT DO NOT REPRESENT UNANTICIPATED PROBLEMS AND DO NOT NEED TO BE REPORTED UNDER THE HHS REGUALTIONS AT 45 CFR PART 46. 1. A subject enrolled in a phase 3, randomized, double-blind, placebo-controlled clinical trial evaluating the safety and efficacy of a new investigational anti-inflammatory agent for management of osteoarthritis develops severe abdominal pain and nausea one month after randomization . Subsequent medical evaluation reveals gastric ulcers. The IRB-approved protocol and informed consent document for the study indicated that there was a 10% chance of developing mild to moderate gastritis and a 2% chance of developing gastric ulcers for subjects assigned to the active investigational agent. The investigator concludes that the subject’s gastric ulcers are within the expected frequency. This example is not an unanticipated problem because the occurrence of gastric ulcers – in terms of nature, severity, and frequency – was expected. 2. A subject is enrolled in a phase 3, randomized clinical trial evaluating the relative safety and efficacy of vascular stent placement versus carotid endarterectomy for the treatment of patients with severe carotid artery stenosis and recent transient ischemic attacks. The patient is assigned to the stent placement study group and undergoes stent placement in the right carotid artery. Immediately following the procedure, the patient suffers a severe ischemic stroke resulting in complete left-sided paralysis. The IRB-approved protocol and informed consent document for the study indicated that there was a 5-10% chance of stroke for both study groups. To date, 25 subjects have been enrolled in the clinical trial, and 2 have suffered a stroke shortly after undergoing the study intervention, including the current subject. The DSMB responsible for monitoring the study concludes that the subject’s stroke resulted from the research intervention. This example is not an unanticipated problem because the occurrence of stroke was expected and the frequency at which strokes were occurring in subjects enrolled so far was at the expected level. 3. An investigator is conducting a psychological study evaluating the factors that affect reaction times in response to auditory stimuli. In order to perform the reaction time measurements, subjects are placed in a small, windowless soundproof booth and asked to wear headphones. The IRB-approved protocol and informed consent document describe claustrophobic reactions as one of the risks of the research. The twentieth subject enrolled in the research experiences significant claustrophobia, resulting in the subject withdrawing from the research. This example is not an unanticipated problem because the occurrence of the claustrophobic reaction – in terms of nature, severity, and frequency – was expected.