1 The Eden Unit Operational Policy Contents Page 3 to 6 Aims of the
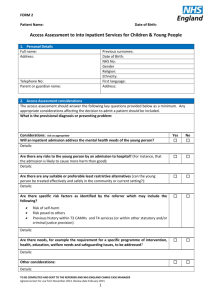
advertisement

1 The Eden Unit Operational Policy The Eden Unit Block C Clerkseat Building Royal Cornhill Hospital Cornhill Road ABERDEEN AB25 2ZH Tel: 01224 557769/557758 COMPLETED JUNE 2009 2 Contents Page 3 to 6 Aims of the Unit Criteria for Admission Page 6 On Admission Page 7 Refeeding Page 8 Therapeutic Programme Page 9 Pre-Discharge Page 10 Social Work Involvement Liaison with Local Eating Disorder Services Intermediate/Outreach Care Page 11 Communication Page 12 Out-of-Hours and Holiday Cover for Psychiatrists Review of Operational Policy Page 13/14 Appendix – Service Flowchart 3 North of Scotland Inpatient Unit for Eating Disorders The Eden Unit Operational Policy This is a 10 bed inpatient unit for the treatment of patients with eating disorders for the North of Scotland ie to take patients from Tayside, Grampian, Highland, Orkney, Shetland and the Western Isles. The Argyll and Bute area which is now part of Highland Health Board has not been included because they will continue to look to west central Scotland for provision of specialist services. The in-patient unit will operate alongside a 4 place day patient facility for Grampian patients, which will help facilitate rehabilitation and make re-admission less likely. This operational policy has been informed by the regular meeting of the Project Steering Group, and developed in conjunction with the Clinical Project Group for the unit. It will be reviewed by those groups and representatives of medical management bodies and informed by the MCN North of Scotland for Eating Disorders. 1. Aims of the Unit The unit will provide intensive inpatient treatment for patients with severe eating disorders. These will be predominately patients with severe anorexia nervosa who are dangerously underweight and/or have not responded to less intensive forms of treatment. The unit will aim to provide 1. A safe environment in which to manage severe eating disorders. 2. A broad range of expertise and therapeutic options for the treatment of severe eating disorders. 3. A detailed assessment of the physical, nutritional, psychological and social needs of the patient. 4. An individually tailored combination of nutritional, psychological, physical and social treatment of the eating disorder. 5. Smooth transitions between the unit and other treatment settings before and following admission to hospital. 2. Criteria for Admission The unit will primarily cater for adult patients aged 18 years and over. 4 Patients younger than 16 would be admitted to specialist inpatient units designed for adolescents or children. This will usually be the case for the 16-18 age group. In exceptional circumstances, where the patient’s maturity, circumstances, and emotional and physical needs would be best served by the Eden Unit, then admission will be considered for the 1618 age group. The unit is funded as an adult unit; hence admission out with this parameter will be uncommon. Likewise the unit does not have access to the correct range of resources that a children’s unit would have to provide usually. Prior to admission patients will have had a comprehensive assessment by local specialist services (local means from the service for the local health board i.e. Tayside, Highland, Grampian, Orkney, Shetland, Western Isles). Normally this would include assessment by a consultant psychiatrist with a special interest in eating disorders from the local specialist services in eating disorders, but where that is not possible then the psychiatric assessment will include detailed input from the consultant psychiatrist from the Eden Unit. Other members of the multidisciplinary team such as specialist nurses, dieticians, clinical psychologists and local general psychiatrists will contribute to the assessment as appropriate. The Eden Unit consultant will include the Nursing ward manager in discussions about the possible admission. This prior to admission assessment will include a full psychiatric history and mental state examination, physical assessment, assessment of the family and social situation and a summary risk assessment. This assessment will take account of all the special considerations relevant to the assessment of an eating disorder, including those outlined in the Quality Improvement Scotland guidance on the assessment and treatment of patients with eating disorders. The assessment will include a consideration of alternative options to admission to hospital. Agreement for admission will be between local specialists, or Multidisciplinary team and the Eden Unit representatives. Prior to admission there would be detailed liaison between the inpatient unit and the local specialist services to clarify the expectations and aims of the admission, including expected duration of the admission. A key worker will be allocated to each patient, on referral, prior to admission to hospital. The key worker will familiarise him/herself with the details of the patient’s problems prior to admission. 5 Transfer of patients into the regional inpatient unit will be the responsibility of the local health board service. Responsibility for the care and treatment of the patient following discharge from hospital will be clarified in advance of admission so that the transition from inpatient care to community care is not disrupted or delayed. See Appendix 1, figures 1 and 2 for clarification of Admission Process. The risk assessment will include a consideration of psychiatric risk such as suicide risk as well as physical risk. See Clinical protocol, information on risk management policies Admissions will be arranged for normal working hours to prevent difficulties in transfer, initial unit based assessment and treatment arising. Thus Emergency admissions will not be accepted. If a patient is considered to be at extreme physical risk, then local (to the patients home) admission to a medical ward is advisable for physical stabilisation. See Clinical Protocol for guidance on physical risk. If suicidality is considered to be the major risk factor out of hours, then emergency admission to a (local to the patient) general psychiatric ward for initial assessment and stabilisation will be most appropriate, obviously from there transfer to the Eden Unit can be facilitated if considered the best course of management. Not all patients with suicidal or impulsive self harm features, who have eating disorder symptomology or diagnoses, will be appropriate for the unit, which provides a service to those with severe eating disorders and their treatment. Urgent admissions, i.e. those needing admission in the next one to two weeks, should be managed by in normal working hour’s procedures. As previously indicated patients assessed at high physical risk will be considered for initial stabilisation in a local Health Board medical unit in consultation with the consultant physician with responsibilities for the regional inpatient unit. There will be cases where patients at physical high risk can be managed safely at the Eden unit with appropriate guidance. The consultant psychiatrist and other senior staff of the unit will be available to discuss and plan the admission with local specialist services, the patient and carers. Arrangements will be in place for informal visiting of patients and carers to meet staff, to see round the unit and to be given oral and written information about the programme. 6 Admissions under the terms of the Mental Health (Care and Treatment) (Scotland) Act 2003 will be accepted. Local councils will be responsible for providing a mental health officer for their patients. While the patient is in the inpatient unit their Responsible Medical Officer (RMO) will be the inpatient unit consultant and RMO responsibility will revert to the local consultant psychiatrist on discharge from hospital. There might be exceptions to this in the case of the under 18 age group, where RMO status might well be best retained by specialist Child and Adolescent psychiatrists. Special attention will be given to referrals coming from patients moving from the child and adolescent age range into the adult age range. These are often difficult transitions in service provision and there will be a careful negotiated overlap of care between child and adolescent services and the adult eating disorders services in these cases. The care pathway leading to admission is summarised in Figures 1 and 2. 3. On Admission All patients will be assessed by the inpatient team and an individual treatment programme designed for them. The assessment will take account of physical, psychological and social (including family) factors and will include a psychological formulation and risk assessment. This biopsychosocial approach will help inform all stages of management. Usual Psychiatric clerking will take place, which will be the remit often of the Speciality doctor (Staff Grade) in psychiatry (.5 WTE) appointed to the unit, or other junior staff with a remit on the ward at that time. There are no training placements currently available to the ward. When not available then the duty junior team will provide cover for this, with a full senior review of this being provided within the first 24 hours of admission. The on-call medical staff will be provided with clear guidance as to areas of particular importance in the initial clerking. The management plan will be built up from this and the initial nursing review. The Eden unit consultant psychiatrist will play a key role, especially since they will have knowledge from initial discussions and even review prior to admission. The consultant psychiatrist and records staff will review the legal status of patients and for those subject to procedures of the mental health act they will review the requirements for review and other documentation. 7 This programme will include expert implementation of a re-feeding programme in order to address the starvation state in the majority of the patients, see Clinical protocol. This could include the use of intravenous fluids and nasogastric feeding where appropriate. There will be close liaison and proximity to general medical services with the availability of a consultant physician with special responsibility for patients with severe eating disorders in the unit and the availability of transfer acutely to general medical services in extreme physical distress needing the close expert physical management of the Gastroenterology service in Aberdeen. Ideally patients will be manageable on the Eden Unit throughout their admission. See Clinical Protocol for further guidance. Direct involvement at initial assessment can be requested from the Gastroenterology team for examination and management advice. There will be the ability (where deemed necessary) to provide one to one psychiatric nursing cover for patients whether they are on the regional inpatient eating disorders unit or in a medical unit. On-going assessment will then follow the pathway as outlined in the Clinical Protocol. An integrated formulation will encompass the individual professional assessments involved, using a biopsychosocial emphasis as previously stated. See Appendix to the Clinical Protocol. 4. Re-Feeding The use of normal food would be the preferred option when re-feeding although the use of nutritional supplements and nasogastric feeding will be available when necessary. Close supervision will be provided at meal times in the early stages of re-feeding. The diet will be balanced and sufficient to ensure weight gain except in the first week or two when intake will be introduced gradually to avoid re-feeding syndrome. The food will be of high quality and appetising. Arrangements will be in place to restrict activity and reduce access to toilets where appropriate and this will be done with due respect of the dignity and privacy of the patient. 8 There will be close medical monitoring to avoid, or note early signs of, re-feeding syndrome. Re-feeding syndromes will be dealt with by reference to the in-patient units supporting physician. Risks are particularly high in the first week of re-feeding, necessitating twice weekly bloods and twice daily physical observations as a minimum. Greater observation, and daily bloods, than that maybe required in high risk patients. See Appendix on risk management, Clinical Protocol. The unit consultant physician will advise on the detailed management of re-feeding. On occasion feeding without consent of the patient will be required. This will be giving in accordance with Mental Health Act requirements and guidance provided by the Mental Welfare Commission. The treatment programme will be flexible and tailored to the individual needs of patients. This will include flexibility about the overall aims of admission. Some patients will aim to have weight restored to a healthy weight while others will have more limited aims to stabilise at a lower but safe weight. For those with a significant duration history of low weight or malnutrition, a DEXA bone scan will be considered. 5. Therapeutic programme All patients will have a key nurse who will meet regularly with them and who will have responsibility for overall implementation of the care plan. This maybe, when appropriate, the same individual who responded to the initial referral by helping organise the admission. On-going individual therapy is seen as an important part of the program. All patients will attend group based therapeutic programmes, as far as they are physically able. These will be designed to cater for patients at different stages in their recovery. Treatment approaches, where possible, will be used according to evidence based criteria and guidelines produced by NICE and QIS. Normal Weight restoration whilst an in-patient will not be seen as the only or even most necessary target in all cases. Many patients may benefit from a shorter admission with recovery of function and a period of more intense therapy being the primary goal. Aims of the treatment should be clear from the outset, but should be regularly reviewed. 9 The following therapeutic modalities will be available in group, family or individual settings. Cognitive Behaviour therapy Motivational enhancement therapy Body image work Eating skills development Attention to excess exercise, vomiting, laxative misuse and other abnormal behaviours associated with eating disorders Self-esteem work Mindfulness work Nutritional education Family work. This will depend on individual patient need and where appropriate will include formal family therapy. Art Psychotherapy Occupational therapy Social therapy Physiotherapy including Body Awareness therapy. Patients will be able to keep in touch with relatives and friends by videolink and telephone subject t an assessment of therapeutic benefit. Family work can also be done via videolink. Doing such work should be seen as expected, to help reduce transition issues back into the community. 6. Pre-discharge Patients will have opportunities independent living skills. These will include self preparation of food, eating out and eating with others, and other activities such as clothes shopping essential to good rehabilitation. There will be an ability to offer patients a trial period at home prior to discharge. There will be possible use of the day-patient (transitional care) facilities for Grampian patients at this stage, once this unit is staffed and opened. There will be close liaison and discussion with local specialist teams to ensure the setting up of a continuing therapeutic programme immediately on discharge. There will be full assessment of areas of social and family need prior to discharge (see social work involvement also). to develop age appropriate 10 7. Social Work Involvement Where the need for an assessment of social care needs is identified during the patients stay in hospital, and there is no existing social work involvement, this will be arranged at an early stage via the local specialist teams who will have the necessary knowledge of local social work services and referral mechanisms. Social work staff involved in the care of patients will be engaged in discharge planning via the local specialist services and attendance at discharge planning meetings. Where a patient has been admitted from one of the Island Health Boards, such social work involvement that is required will be arranged in collaboration with the referring clinician. Social work input will be vital in sustaining rehabilitative measure postdischarge. Where patients are subject to compulsion under the Mental Health (Care and Treatment) Act a designated Mental Health Officer shall be appointed by the Local Authority where the patient is normally resident. 8. Liaison with Local Eating Disorder Services There will be regular meetings with the local clinical team throughout the period of admission. This could include local clinicians attending ward meetings and if travel is a problem there will be video conferencing facilities available to enable the local specialist service to be involved. Continuing direct clinical contact between local clinicians and patients will be encouraged with the aid of video conferencing facilities if necessary. There will be prompt reporting to the local clinical team on significant developments e.g. urgent plans to discharge the patient or to have the patient taking timeout of the programme, serious self-harm or failure to progress. There will be facilities in place for local eating disorders and other specialist staff to visit and speak to the patient and staff. There will be progress summaries by letter at 1 month, full assessment reports and 3 months and discharge. These will contain information as collected by the clinical protocol. 9. Intermediate/Outreach Care The transition from inpatient to community care will be a crucial stage in the patient’s treatment. 11 There will be a specially designated group of staff who will have responsibility for ensuring good liaison and planning both before and after admission and for the provision of transitional care while patients move to a locally based outpatient programme. Individual key workers will also be involved. The transitional care arrangements will vary depending on where the patient lives and other local factors such as the intensity of service available from the local specialist service. In Grampian it is anticipated that most patients will make significant use of the transitional care service and will attend as day patients for a month or two following discharge from inpatient care. It is also expected that some patients from Tayside/Highland will be able to make use of day patient attendance. For the remainder of Tayside patients and the most of Highland patients it is expected that the transitional care will be provided more locally, but there will be the option of continuing appointments at the regional unit, telephone advice and video conferencing. The aim will be maximum flexibility to meet the very individual circumstances of each patient. 10. Communication Patients will not be considered for admission without a referral letter giving an adequate assessment of the patient’s history and setting out the reasons for requesting admission. Communication by telephone, e-mail and other means would be welcomed but would not substitute for a formal written referral letter. Initial communication needs to present a full picture of the physical status of the patient and any areas of other significant risk. See Clinical Protocol on pre-admission information. Liaison might need to include discussion with the in-patient unit’s attached physician to help draw up a safe plan for admission. The admitting team will write to the referrer confirming whether admission is to be offered and giving some idea when a bed would be available. By four weeks following admission there will be a detailed admission care plan a copy of which will be made available to the patient and to the referring clinician. This will have been prepared in consultation with the patient, carers where appropriate and with the referring team. 12 At three months of admission a detailed assessment report and progress update will be sent to the referring region, this may in some cases be a detailed discharge report. Prior to planned discharge the local eating disorders or other specialist team will be given at least two weeks notice in order to prepare appropriate follow up arrangement. If there is an acute unplanned discharge then information about this happening and the reasons will be conveyed urgently by telephone to the local service. On discharge a note of immediate treatment recommendations including medication will be sent to the local general practitioner and the local specialist service on the day of discharge. A full typed discharge summary (see above) will be sent to the local general practitioner within two weeks of discharge. All patients will be reviewed by the clinical team regularly ie at least weekly and any significant changes in the management plan will be discussed with the local specialist team. 11. Out-of-Hours and Holiday cover for Psychiatrists The out of hours doctors, including the Consultant rota, will provide cover for the unit for medical and Psychiatric situations that arise. They are likely to involve the need for usual medical and psychiatric assessment for situations that will usually involve predictable physical or psychiatric complications. These are covered in the Clinical Protocol. The expectation is that not taking emergency admissions and usual daytime practice will greatly reduce the need for out of hour’s involvement. 12. Review of Operational Policy Once agreed this policy will be fully reviewed after 12 months in conjunction with the involved regions, Project Steering group, Clinical project group and the MCN for Eating disorders. Date of Review: Appendix 1 1 Figure Inpatient Treatment for Severe Eating Disorders Under 16’s 16 – 18 year olds Full assessment & consideration of alternatives by area CAMHs’ Service 16 – 18 year olds Decision to admit Regional adolescent inpatient unit Decision of where to admit for 16 – 18 year olds to depend on maturity, educational needs, family situation geography, physical and psychological need. Exceptionally will be to the Eden Unit. Over 18’s Full assessment and consideration of alternatives by area eating disorder team and where appropriate local adult mental health service. Liaison when required with Eden unit Consultant. Eden Unit 14 Referral to IP Unit from Tertiary Services or Secondary Services (over 18 years of age) Comprehensive Assessment* by local specialist services (including assessment by Consultant Psychiatrist from local specialist service or Consultant from Regional ED Unit in liaison with local Consultant Psychiatrist and Multidisciplinary Team.) Consider alternative options to admission Decision to admit Discussion to plan admission between IP Unit & Local Specialist Services: Eden Unit Consultant and Ward manager Admission ** See Below Risk Assessment – both physical & psychiatric risk High Physical Risk – consider stabilisation in medical unit in the first instance. Liaison with Consultant Physician. Informal Visit by Patients/Carers to Unit. Supply Patient with oral & written information re unit. *To include full Psychiatric History and MSE, Physical Assessment, risk assessment & assessment of family situation ** Responsibility for care and treatment of the patient following admission to hospital will be clarified in advance of admission so that transition from IP Care to Community Care is not disrupted