UNIVERSITY OF SANTO TOMAS FACULTY OF MEDICINE AND
advertisement

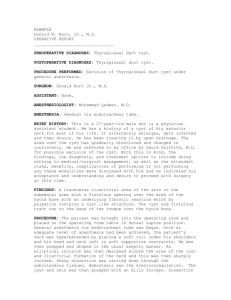
UNIVERSITY OF SANTO TOMAS FACULTY OF MEDICINE AND SURGERY DEPARTMENT OF CLINICAL EPIDEMIOLOGY AN EVIDENCE BASED MEDICINE APPROACH TO THYROGLOSSAL DUCT CYST Eugenio, Clarisse Marie Evangelista, Kristy Elleza Facton, Rosabelle Fajardo, Revie Anne Fang, Mark David Fontano, Michael Jeff Francisco, Therese Pauline Gabuat, Harry Gaffud, Prima Bianca Gagtan, Majelle Gallardo, Estee Lauren Heart Garan, Aileen Elizabeth Garcia, Cholson Banjo Garcia, Louise Fatima Garcia, Mark Jezreel February 11, 2010 1 CASE SCENARIO CA, 20, Female has an anterior cystic mass that started to grow in the area since she was 3 years old. The cystic mass is exactly at the midline at the level of the thyroid cartilage. This is smooth, well circumscribed, non tender and moves up when the tongue is protruded. Salient Features 20 y/o, female Anterior cystic mass; exactly at midline, level of thyroid cartilage Smooth, well circumscribed, non tender and moves up when the tongue is protruded Clinical Impression THYROGLOSSAL DUCT CYST Thyroglossal duct cysts often present as anterior midline masses in the 1st decade of life. More than 25% of thyroglossal duct cysts present before the age of 5, and 40% present by the age of 10. Thyroglossal duct cysts appear at a constant rate of almost 10% per decade in the ensuing years (Hechtman et al 2007). Embryology An appreciation of the embryology of the thyroid gland is important for an understanding of the surgical approach to excision of thyroglossal duct cysts. During the 3rd week of gestation, an epithelial thickening develops at the tuberculum impar on the anterior pharyngeal wall. This thickening, the median thyroid anlage, divides into a bilobed structure representing the developing thyroid gland. Rostral growth of the embryo results in caudal displacement of the median thyroid anlage with persistence of a median stalk stretching to the tuberculum impar. Canalization of the median stalk produces the thyroglossal duct, which typically courses ventral to the hyoid anlage, but can pass through or dorsal to it. In the 5th week of gestation, the duct degenerates and is resorbed. Secretion by epithelium – lined remnants of the duct can lead to thyroglossal duct cyst. The stimulus for secretion is unknown but can occur any time, accounting for the appearance of the cysts later in life. Clinical Presentation and Evaluation A thyroglossal duct cysts usually presents as a suddenly appearing, unsightly, or inflamed midline neck mass, or is discovered on routine physical examination. The cyst is located 2 within 2 cm of the midline and typically overlies the hyoid bone, although it may be found anywhere along course of the thyroglossal duct. Unless infected, the cyst is smooth and mobile without communication with the overlying skin. Diagnosis requires nothing more than a careful history and physical examination. A typically positioned mass that rises in the neck with swallowing or with protrusion of the tongue is diagnostic (Hechtman et al 2007). Confirmation of the thyroid in its normal location by palpation or demonstration by ultrasonography may be important to avoid incidental excision of a partially descended thyroid. Routine thyroid scintigraphy is advocated by some to identify this extremely rare phenomenon. In the typical patient with a recently identified upper midline neck mass, however the likelihood of this diagnosis is remote and routine testing is not indicated. Dermoid cysts are occasionally identified at the time of surgery or pathologically after excision of a presumed thyroglossal duct cyst. Dermoid cysts can usually be distinguished intraoperatively by the finding of thick, white sebaceous contents. Additional diagnoses to be considered include lymphadenitis, enlargement of the thyroid pyramidal lobe, and either locally occurring or metastatic neoplasia. An operation is scheduled at the earliest convenience to avoid the morbidity of intervening infection. If infection is present, the operation is deferred until the inflammatory process is fully resolved. Incision and drainage are rarely required. Surgical Technique The contemporary approach to excision of thyroglossal duct cysts is attributed to Sistrunk, for whom the procedure is named. He incorporated resection of central hyoid bone and the tract extending to the foramen cecum with excision of the cyst. This maneuver reduces the incidence of recurrence to less than 5% from 25% when cystectomy alone is performed (Hechtman et al 2007). Complications and Recurrence The most potentially dangerous complication after thyroglossal duct excision is postoperative wound hemorrhage with resultant airway compromise. Careful hemostasis, not routine drainage of the wound, is the optimal approach in avoiding this uncommon complication. Wound infections are infrequent and respond to treatment with oral antibiotics. Recurrence after thyroglossal duct excision occurs in approximately 5% of patients, typically within 1 year of the procedure (Hechtman et al 2007). Inflammation of the anterior neck associated with localized swelling or a draining sinus is the characteristic presentation. Drainage may or may not occur at the incision scar. Recurrence is usually attributed to inadequate excision of thyroglossal duct remnants. 3 Spectrum of Disease 5% 7% 20% Higher threshold Pre-test probability Lower threshold The pre – test probability was set in 7% for this reason: Thyroglossal tract remnant occurs in 7% (which is usually asymptomatic) of the total population and only 20% occur at ages 20-30 years age. TTR/TDC is more common on pediatric patients which occur at around 30%. The incidence of ectopic thyroid tissue, misdiagnosed as a thyroglossal tract remnant, is probably between 1 and 2%, according to a series by Radkowski et al which makes our pretest probability much lower Mostly thyroglossal duct cyst is diagnosed early and intervention is well established. Most adult patient at peak of around 4th decade has greater incidence for a malignancy. The lower threshold was set at 5 percent for this reason: The diagnosis of TDC can be established with good history and physical examination. Physical examination reveals a midline mass at or below the hyoid bone, firm, nontender, and mobile with protrusion of the tongue. This makes the diagnosis more cost efficient. TDR are the most common midline neck masses representing more than 75% so higher probability of diagnosing the disease in our patient. The higher threshold was set at 20 percent for this reason: Incidence of primary malignancy is estimated at only 1%. Since complication of not having treatment has a low chance of occurrence, we therefore place the high threshold father from the pre-test probability. Major complications of TDC surgery are rare. They include recurrence, abscess or hematoma requiring surgical drainage, entry into the airway, the need for tracheotomy, nerve paralysis, hypothyroidism, and death. Minor complications such as seroma, local wound infection and stitch abscesses were reported in 9 - 29% of the case. Recurrence rate after Sistrunk surgery is averaging of about 6.6%. 4 CLINICAL DECISION ON DIAGNOSIS CLINICAL QUESTION: Is there a role for ultrasonography in the pre-operative diagnosis of thyroglossal duct cyst? Population: thyroglossal duct cyst Intervention: ultrasonography Outcome: preoperative diagnosis Methodology: retrospective cohort Search: Finding the Evidence: 1. Visited http://www.ncbi.nlm.nih.gov/pubmed/ Search terms: Thyroglossal duct cyst, sonography, preoperative diagnosis. First search term is “thyroglossal duct cyst” and the result is a total of 1,038. 5 Second search term is “sonography” and the total result is 285,674. 6 Using MESH terms search we combined the result from thyroglossal duct cyst and sonography by typing #1 AND #2. The combined result of search #1 and #2 showed a total study of 81. Third search term is “preoperative diagnosis” and the total result is 102,718. 7 Using MESH terms we combined the result from thyroglossal duct cyst, sonography and preoperative diagnosis by typing #3 AND #4. The combined result of search #3 and #4 showed a total study of 17. 8 With the list of journals narrowed down and limited, the right journal was found. 9 ______________________________________________________________________________ CRITICAL APPRAISAL ON DIAGNOSIS Article: “Preoperative Sonography in Presumed Thyroglossal Duct Cysts” Gupta P., Maddalozzo J. RELEVANCE Is the objective of the study relevant to your clinical question? YES. To understand the role of the diagnostic tool, some things are to be considered. Most literature would suggest that the diagnosis of thyroglossal duct cyst in through a thorough history and physical exam: being it a midline cystic neck mass at the vicinity of the hyoid that moves with deglutition. This could however be problematic since a in a few number of cases there have been reports of the inadvertent removal of an ectopic thyroid gland that was mistaken for a TGD cyst. Thus there could be a need to truly characterize the midline neck mass through imaging. VALIDITY GUIDES Was there an independent and blind comparison with a reference standard? It was not stated in the article whether or not there was an independent comparison between sonography and the reference standard used, histopathology findings Did the patient sample include an appropriate spectrum of patients to whom the test will be used? YES. Although, there was no mention of the age range of the pediatric patients, all patients had cystic midline neck masses at the vicinity of the hyoid which is a characteristic of thyroglossal duct cysts. Was the reference standard done regardless of the result of the diagnostic test being evaluated? 10 YES. A pathologic examination was done post-operatively to characterize the midline neck mass lesion. Were the methods for performing the test described in sufficient detail to permit replication? YES. It was mentioned in the methods and ‘patients and methods box’ on page 2. OVERALL, IS THE STUDY VALID? Yes, the study met most of the criteria for a valid study. 11 WHAT ARE THE RESULTS? Diagnostic Test Ultrasonography Positive Negative Thyroglossal Duct Cyst (Histopathology) Present Absent 37 2 0.37 38 Based from the results tabulated in above table, the sensitivity and specificity of ultrasonography is 99% and 95%, respectively. What are the likelihood ratios for the different possible test results? Positive LR: 19.8, negative LR: 0.01. Since the positive LR is more than 10 (19.8), it is expected that there will be conclusive changes from the pre – to post test probability. A negative LR of 0.01, which is less than 0.05, it is expected to alter the probability to a small (and rarely important) degree. Shown below is how the group was able to compute for the post test probability: Pre test probability to pre test odds: (p/1-p) Pre test odds = 0.07 / (1 - 0.07) = 0.08 Post test odds: pretest odds x likelihood ratio If positive = 0.08 x 19.8 = 1.58 If negative = 0.08 x 0.01= 0.0008 Post test odd to post test probability: If positive = 1.58 / (1.58+1) = 60% If negative = 0.0008 / (0.0008+1) = 0% Spectrum of Disease 0% 5 % 7% 20% Higher threshold 60% Positive Post Test Probability Pre-test probability Lower threshold Negative Post Test Probability 12 CAN THE RESULTS HELP ME IN CARING FOR MY PATIENTS? Will the reproducibility of the test result and its interpretation be satisfactory in my setting? There was no clear way of how the results were actually interpreted and how they were able to come up with the sensitivity and specificity of the test. Are the results applicable to my patient? YES. Since the disease is actually very rare and the findings of ultrasonography are highly specific, then it may be applied to our patient and although the age range of the patients (pediatric) is different from our patient (20 years old- adult), their clinical presentation is similar. Will the results change my management? Generally, the management will be dependent on which part of the spectrum the computed post test probability will fall. If the post test probability falls beyond the set upper testing threshold, a diagnosis of rabies is made and immediate treatment will be initiated to prevent the further spread and development of the disease. But if the value will fall below the lower testing threshold, the probability of having rabies can be ruled out and the patient can be sent home. RESOLUTION OF THE PROBLEM IN THE SCENARIO Our patient, having all the classical findings of a thyroglossal duct cyst may therefore undergo surgical intervention without the necessity of an ultrasonography. CATMAKER Preoperative Sonography in Presumed Thyroglossal Duct Cyst Clinical Bottom Line: Ultrasound maybe used as a preoperative diagnostic tool for thyroglossal duct cyst however the clinical findings may already suffice. Citation/s: Gupta, Pankaj and Maddalozzo, John, Preoperative Sonography in Presumed Thyroglossal Duct Cyst. Arch Otolaryngolol Head Neck Surg/Vol 127, Feb 2001 Three-part Clinical Question: Is there a role for ultrasonography in the pre-operative diagnosis of thyroglossal duct cyst? Search Terms: thyroglosal duct cyst AND sonography AND preoperative diagnosis 13 The Study: The Study Patients: 20y/o, female, anterior midline neck mass at the level of thyroid cartilage, smooth, well circumscribed, cystic, non-tender, moves up when tongue is protruded Couldn't tell if there was an independent, blind comparison with a reference (gold) standard. There was an appropriate spectrum of patients. The gold standard was applied regardless of the test result. Target disorder and Gold Standard: Thyroglossal duct cyst confirmed by histopathology Diagnostic test: Ultrasonography The Evidence: TR> TR> Target Disorder: thyroglossal duct cyst Test: ultrasonography Present Absent Test Result Num Prop Num Prop Positive 37 a 2 b Negative .37 c 38 d Likelihood Ratios 5.13 to 19.80 76.48 0.00 to 0.01 0.26 Sensitivity: 99%; CI: 96 to 100 Specificity: 95%; CI: 88 to 100 Prevalence: 48%; CI: 37 to 59 Positive Predictive Value: 95%; CI: 88 to 100 Negative Predictive Value: 99%; CI: 96 to 100 Comments: Appraised by: Fajardo, RA; Fontamo, MJ; Gaffud, PB; Garcia, MJ, February 7, 2010. Kill or Update by Tuesday, February 09, 2010 Particular to my patient: Pre-test probability: 7% Test Result Post-test probability Positive 60% Negative 0% 14