Question 1 - The College of Anaesthetists of Ireland
advertisement

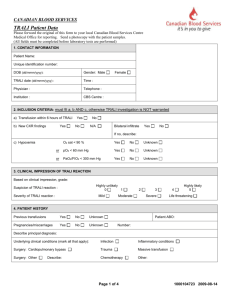
DIPLOMA OF FELLOW OF THE COLLEGE OF ANAESTHETISTS Royal College of Surgeons in Ireland Final Examination – Model Written Paper – XXXXX 2012 Answers to Sections A and B to be written in separate answer book and clearly marked Time allowed for this paper – 3 hours All questions must be attempted SECTION A Question 1 A 58 year old woman admitted following a road traffic accident has an epidural haematoma from the 1st to 5th thoracic vertebral spaces and a sensory level at T2. She is scheduled for emergency spinal surgery (prone position). Outline your Anaesthetic management and subsequent Intensive Care management of this patient in the first 72 hours after injury. Question 2 Write short notes on: a) Transfusion-related acute lung injury (TRALI). b) peripheral nerve injuries arising in the perioperative period. Question 6 Write short notes on: a) Gabapentin b) the effect of anaesthetic drugs given during labour or at delivery on fetal outcome. c) the causes and investigation of muscle weakness in long term critically ill patients. Question 1 1. Introduction Spinal chord injury should be suspected in patients with:a. Major trauma, b. Minor trauma who report spinal pain or have sensory-motor symptoms, impaired level of consciousness. Management goals are, if possible, to reduce the result of neurological deficit and to prevent any additional loss of neurological function. The cervical region is the most mobile portion of the spine, as well as the most common site of spinal cord injury. 5% of major trauma patients have unstable cervical spine, two thirds of which have no neurological deficits. The thoracic spine vertebrae, T1 to T10, have considerable intrinsic stability due to the rib cage and are relatively immobile. Injuries to this region are relatively uncommon and the spine usually remains mechanically stable unless multiple rib fractures are present. 2. Resuscitation and Initial Evaluation Standard resuscitation should have occurred with stable haemodynamics. Standard biochemical and haematological investigations particularly including coagulation status should have been performed and corrected. Standard trauma workup with evaluation of CNS, Chest, Abdominal, Orthopaedic injuries should have been completed. Before the injured patient is moved, rigid cervical collar should be put in place, without moving the patient’s neck. Sandbags are placed on either side of the head which further immobilise cervical spine movement. More effective immobilisation is accompanied by “log rolling” the patient on to a rigid transportation board in which the head is secured by straps or tapes. 3. Airway Management Hypoxaemia, secondary to hypoventilation or aspiration of gastric contents are major potential consequences of upper thoracic spine injury. Hypoventilation may be treated initially with supplemental oxygen via face mask or nasal prongs if the patient is conscious and alert. 4. Cardiovascular resuscitation. Sympathetic innovation of the heart is derived from the cardio accelerator nerves T1 to T4. Extrinsic compression of the spinal cord at T1 to T5 level may produce vasomotor paralysis below the lesion resulting in vasodilatation, increased venous capacity and hypotension. The associated bradycardia may distinguish this response from hypovolaemic shock. Intravenous crystalloid colloid solution should be administered to correct the relative hypovolaemia. Vasopressors, phenylephrine or metaraminol may be used to treat hypotension due to vasodilatation that persists after adequate volume replacement. 5. Pharmacological Treatment 30mg/kg methylprednisolone intravenously has been advocated within 8 hours of spinal cord injury followed by continuous infusion of 5.4mg/kg per hour for 24 hours. Data suggests improved maximum motor function. 6. Ancillary Treatment Foley catheter to prevent bladder distension and allow continuous assessment of urine output 7. Neurological Evaluation A detailed and accurate initial neurological evaluation is essential to establish baseline status and plan for further investigation and treatment. Assessment of major muscle groups of the upper and lower extremities should be systematically graded using 6-point scale to serve as a baseline for further neurological assessment. Diaphragmatic function should be normal because of its C3 – C5 innervation. Extrinsic compression below the level of C5 should not affect diaphragmatic function. Innervation of intercostal muscle may be associated with hypoventilation and subsequent hypoxaemia. Sensory function assessment includes proprioception and response to light, touch and pin prick. Spinal neurogenic shock may be seen in the period immediately following complete injury at T6 level comprising areflexia, loss of sensation and flaccid paralysis below the level of the lesion, flaccid bladder with retention of urine and lax anal sphincters. Cardiovascular manifestations include bradycardia and hypotension. Anaesthetic Management for Prone Position Thoracic Epidural Decompression Combined use of a semi-rigid collar, sandbags placed on both sides of the head, neck and backboard provides the most reliable immobilisation. For airway management manual in-line stabilisation with assistant holding the head and torso of the patient is a practical and safe method. Evaluation of the airway for induction of anaesthesia is mandatory. Assuming no airway management difficulties, monitoring consisting of standard ECG, non-invasive blood pressure, pulse oximetry, large bore intravenous access. Depending on the duration of such injury and fasting state, a rapid sequence induction comprising thiopentone dose sufficient to render anaesthesia, suxamethonium1mg/kg following pre-oxygenation with cricoid pressure. Reinforced armoured endotracheal tube and subsequent insertion of nasogastric tube and oesophageal stethoscope. Tape padding eyes. Direct arterial cannulation for blood gas analysis and anticipation of potential for significant blood loss. Group and cross match four units pack cells. Temperature monitoring and active measures to prevent hypothermia. Careful patient log rolling to the prone position. Careful positioning with regard to potential peripheral nerve damage. End of Surgery Position from prone to supine. Application of cervical collar. Reversal of neuromuscular blockade. Assessment of upper and lower limb neurological function. If satisfactory, reversal of neuromuscular function head lift, grip strength and adequate upper and lower limb motor function, consider awake extubation. Postoperative Care Initiate referral to ICU/HDU area early. Consider postoperative management to include supplemental oxygen therapy, humidification with oxygen saturation and haemodynamic monitoring. Frequent arterial blood gas monitoring and close observation of respiratory function and effort. Be wary of rising pCO2, acidosis, tachypnoea, tachycardia, sweating. Prophylaxis with proton pump inhibitors and H-2 receptor blockers diminish gastric acid secretion. Active measures to reduce the incidence of pulmonary emboli include use of pneumatic compression devices as well as subcutaneous administration of low molecular weight heparin beginning as soon as possible after injury. Question 2a Transfusion related acute lung injury. TRALI occurs shortly after transfusion of blood/blood products but especially products containing plasma. It can occur within 1-2 hours but also up to 6 hours after transfusion. It is characterised by hypoxemia, dyspnoea, fever, cough and shadowing in the perihilar and lower lung fields on chest radiograph often associated with non-cardiogenic pulmonary oedema. It is probably often unrecognised and misdiagnosed (as aspiration pneumonia or cardiogenic pulmonary oedema). Its (estimated) incidence is 1:5,000 plasma-containing products transfused. An overview of the initial 252 cases received by the Serious Hazards Of Transfusion (SHOT) scheme reported that TRALI accounted for 16 (6%) of them. The principal mechanism involves the reaction of donor (especially multiparous women) plasma antibodies, agglutinins with recipient neutrophil antigens resulting in increased pulmonary capillary permeability. Complement is activated and C5a promotes neutrophil aggregation and sequestration in pulmonary microcirculation. Reactive lipid products from donor cell membranes also play a role in the pathophysiology of TRALI. These “primed” neutrophils worsen the injury to pulmonary capillary endothelium, especially in the setting of sepsis. More recently, the term TRALI has been used to refer to other causes of post-transfusion ARDS (platelet reactions, DIC and anaphylactic reactions). There are no specific laboratory tests available for diagnosing TRALI; initial diagnosis depends on awareness of the problem and a high degree of suspicion. No specific therapy exists – therefore management is supportive and the same as for any cause of ARDS. In contrast to ARDS, most patients appear to improve within 48 hours if well resuscitated and thereafter make a full recovery. This widely accepted view of the prognosis of TRALI may be overly optimistic as a result of under-reporting of TRALI associated deaths. If a case of TRALI is suspected, it is important that the local blood centre and/or haematologist is informed, so that donors of potentially dangerous plasma can be retired from the donor list and the case can be reported to SHOT. Females who have been immunized against leucocyte antigens during multiple pregnancies are largely responsible for the majority of implicated donors; many blood services initially only investigate female donors. Avoiding TRALI can be helped by avoiding unnecessary transfusion, particularly of plasma containing products. Question 2b Peripheral nerve injuries arising in the perioperative period. Nerve injury is an important source of patient morbidity and professional liability. True incidence is unknown due to significant under-reporting. Statistics taken from ASA closed claim project indicate that nerve injury is the second most common in database (16%). Specific Nerve Injury: Ulnar Nerve 28% Brachial Plexus 20% Lumbo sacral root 16% Spinal Cord 13% Less commonly affected: Sciatic Median Radial Femoral Aetiology 1. Direct Trauma – needle, sutures, instruments. 2. Injection of neurotoxic material. 3. Mechanical factors i.e. stretch, compression, positioning. 4. Ischaemia likely to be contributing to all these cases. Classification Degree of damage will determine level of intervention required and likely recovery. a. Neuropraxia – myelin damaged, axon intact recovery weeks to months, good prognosis. b. Axonotmesis – axonal disruption, prognosis and recovery variable. c. Neurotmesis – nerve completely severed, ± surgery required, poor prognosis. Predisposing Factors 1. Medical Conditions: i. Pre-existing generalised neuropathy. ii. Systemic factors – hypothermia, hypotension, hypoxia, electrolyte disturbances, uraemia, diabetes, Vit B12 and foliate deficiency. 2. Surgery itself. 3. Anaesthesia factors – direct needle damage, (short levelled needles less nerve fascicle perforation), good anatomical knowledge, and careful techniques – “awake” blocks. Symptoms Can occur within 24 hours, but may not present for 2 – 3 weeks. Intensity and duration vary with severity of injury – numbness, mild paraesthesia to painful paraesthesia, sensory loss, motor loss developing into reflex sympathetic dystrophy. Ulnar Neuropathy M: F 3:1 increases with extremes of weight, 85% occurs with G.A. superficial condylar groove of the elbow very vulnerable. Preferable supinate arm than pronate. Groove less direct contact with arm board. Men – less fat at groove level hence increase % of injury. Brachial Plexus Excessive stretching especially if head is rotated opposite direction. Arm board less than 90 deg abduction preferably only one arm out. Lumbo Sacral Root Injury (Radiculopathy) > 90% associated with regional technique 55% Spinal 37% Epidural Paraesthesia or pain during needle insertion or injection of drug with multiple unsuccessful attempts increases likelihood of damage. Positioning of Patient Lithotomy – lateral popliteal nerve must be outside stirrups. Prone – care with arms during the turn, Brachial Plexus and Orbits Prevention 1. Awareness of complications and common causes of injury e.g. careful positioning. 2. Thorough history, examination and good documentation of pre-operative nerve lesions. 3. Good anaesthetic record of procedure. 4. Awake or lightly sedated blocks. 5. Avoid regional blocks in an unwilling patient. 6. Always stop injecting if there is pain or paraesthesia. Question 3a Gabapentin Gabapentin is an anticonvulsant that is also licensed for the treatment of all types of neuropathic pain. The mechanism of action is not well understood but is thought to involve binding to voltage dependent calcium channels which inhibit the calcium currents that are central to neuropathic pain. It is thought to achieve its analgesic effects through an increase in GABA, a reduction in glutamate and monoamine neurotransmitters and modulation of NMDA receptors. Although Gabapentin is an analogue of GABA it does not possess any GABA-ergic activity. The usual dose is 1800mg/day having been titrated upwards over a few days or weeks. The common adverse effects are somnolence, dizziness, nausea and weight gain. Gabapentin is eliminated entirely by renal excretion and the dose should be adjusted according to creatinine clearance. Clinical trials have shown it to be effective in diabetic neuropathy, post herpetic neuralgia and in neuropathic pain of mixed aetiology. Question 3b Effect of anaesthetic drugs given during labour or at delivery on fetal outcome. Drugs given to the parturient during labour or at delivery may affect the fetus or newborn by a direct pharmacological effect following placental drug transfer or indirectly by affecting maternal physiology, placental perfusion, maternal acid-base balance or the progress of labour. Drug transfer depends upon: Lipid Solubility Placental permeability Concentration gradient for the unbound diffusible drug which in turn depends upon a) pH gradient b) blood flow and c) plasma protein binding. Neonatal drug elimination Hepatic and renal mechanisms are poorly developed in the new born. Hence many drugs which pass into the fetus before delivery have a more prolonged elimination half-life than in the mother and the drug effect persists for a longer duration. Anaesthetic Drugs used for Pain Management during Labour and Delivery Nitrous Oxide (N20) - Entonox combined with systemic pethidine may exacerbate the episodes of maternal hypoxaemia but rarely have been shown to be harmful to the baby. Isoflurane and Sevoflurane - cross the placenta freely but in the concentration used for analgesia have no depressant effect on the new born. Pethidine exhibits “flow dependent placental transfer”. In the presence of hypoxia, the fetus becomes more acidic hence more opioid passes from mother to fetus. Fetal concentration of the drug rises. This may result in a decrease in fetal heart rate within minutes lasting for 30 minutes simulating foetal distress. Pethidine has been associated with neonatal respiratory depression maximum when delivery occurs 1-3 hours after administration. Morphine - this is less lipid soluble, has a slow transfer and has no advantage over pethidine. Diamorphine - is more lipid soluble but has no significantly different effect than pethidine. Fentanyl’s - fentanyl, alfentanil and sufentanil following systemic administration cross placenta more rapidly due to higher lipid solubility than pethidine. They also exhibit higher albumin binding hence more concentration in the fetus- a potential for prolonged fetal depression. Remifentanil - has a short half life in the fetus/newborn hence is less depressant than fentanyl which exhibits a much greater half life. Drugs for Regional Analgesia Local Anaesthetics (LA) (a) In Utero Direct effect on the fetal heart causes deceleration within 30 mins of epidural injection; more so with high concentration of Bupivacaine. LA’s may by indirect effect cause fetal bradycardia secondary to maternal hypotension and uterine hypoperfusion. (b) In the New born Neurobehavioural effects have been associated more with lignocaine than bupivacaine described as “floppy but alert” baby. Vasopressors. In a high risk baby ephedrine seems to be better than phenyephrine as it avoids uterine blood vessel vasoconstriction. Neuroaxial opioids - all epidural opioids administered during labour have a potential to produce neonatal depression by direct effect. As the dose is generally small the effects are much less than after systemic administration. General anaesthetic drugs for caesarean section Thiopentone is the most commonly used intravenous induction agent in pregnancy for caesarean section. It is highly liquid soluble and free, unionised drug passes into the brain and placenta in one-arm organ circulation time. Thiopentone has similar effects on the fetus as on the mother and the extent depends upon the dose delivered to the fetus hence on the induction – to – delivery time. Quicker the delivery less will be the effect. Propofol is not licensed for use in obstetric anaesthesia. It seems to have a more depressant effect on the baby than thiopentone. Profound neonatal depression and sedation for more than an hour after delivery have been reported after induction with propofol. Volatile agents In the concentration used (end tidal 0.5% and 1% respectively for isoflurane and sevoflurane) do not have any clinically significant effect on the neonatal cardiac, respiratory or renal function. Opioids- Fentanyl in doses of 50 – 100 mcg if used for c/section has not been shown to have any adverse effect on the fetus. Neuromuscular blocking drugs - these are fully ionised drugs and cross the placenta slowly. In clinical doses they do not have any effect on the new born. Question 3c Causes and investigation of muscle weakness in long term critically ill patients. There are many causes of weakness in such patients. For many years it was thought that this was due to their having been immobile for a prolonged period (disuse atrophy) and because their metabolic requirements (often substantially raised due to sepsis) were unlikely to have been fully met. Muscle wasting was therefore considered likely and nearly inevitable. The patients were also likely to have received pharmacological agents, particularly muscle relaxants, to aid management of ventilation and other drugs such as steroids and aminoglycosides whose side effects were known to include muscle weakness. Electrolyte abnormalities such as hypokalaemia and hyponatraemia could also contribute to the clinical picture. However, a significant number of patients existed in which the condition could not be reversed by nutritional support and physiotherapy alone, and in whom the weakness persisted long after relevant drugs had been stopped. Two clinical entities could be detected in such patients – myopathy and polyneuropathy, which could be diagnosed by neurophysiological investigations, and histological examination of muscle biopsies. Myopathy This was initially recognised in patients who had received ventilation for acute asthma, often with high dose steroids who were found to have a distal weakness but normal nerve conduction velocities and low amplitude motor potentials. Muscle biopsy confirmed a myopathy and actual rhabdomyolysis has been found. Evidence of associated renal failure has also been found with raised creatine kinase and the picture is particularly associated with sepsis and drug overdose. The main differential diagnosis is ischaemia and reperfusion injury. Neuropathy Some patients exhibit a proximal muscle weakness with decreased or absent reflexes but without sensory or cranial nerve deficit. EMG suggests muscle denervation but with normal motor conduction velocities - an acute axonal neuropathy. Some patients who have suffered severe hypotension exhibit a peripheral motor and sensory polyneuropathy of variable severity. The condition is known as Critical illness neuropathy (CIN). In patients who are found to have significant weakness after an episode of critical illness (and who may have been difficult to wean from ventilation) it is necessary to consider whether the problem pre-existed or caused the episode requiring ICU admission. Such conditions would include previous nerve and particularly spinal damage, CVA, meningoencephalitis, myasthenia gravis, and conditions such as the Guillian Barre Syndrome (GBS). A thorough clinical neurological examination is mandatory with EMGs and nerve conduction studies as necessary. Examination of cerebro-spinal fluid will rule out GBS as fluid protein is normal in CIN. Muscle fibrillation suggests neuropathic damage. A muscle biopsy may be used to confirm a myopathy and creatine kinase will usually be raised. Severity of the initial illness is associated with the incidence of CIN. Steroids in high doses are associated with the myopathy. Persistent neuromuscular blockade has been associated with muscle relaxants, particularly pancuronium and vecuronium (and its metabolite 3-des-acetylvecuronium) if used for over 2 days especially in patients with renal failure and in females. It is reported that the blockade may persist for months. Most patients who survive the initial critical episode will recover reasonable function eventually.