Introduction
advertisement

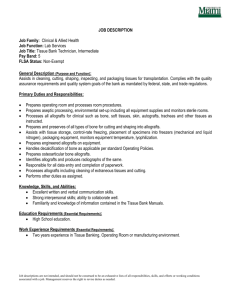
CD40 Costimulation Blockade in Limb and Nerve Transplantation Thomas H. Tung, MD, Susan E. Mackinnon, MD. Introduction: Hand and other nonvital transplantation procedures are controversial because of the risks associated with long-term immunosuppression and the likelihood of chronic allograft rejection. Recent investigation has focused on antibody-based therapies such as CD40 costimulation blockade that can reliably induce tolerance in experimental models of organ transplantation. This strategy has not been previously applied to composite tissue transplantation and may facilitate the universal acceptance of nonvital transplantation. This essay summarizes the current understanding of costimulation theory and our study of the efficacy of CD40 pathway blockade in composite tissue transplantation. Methods: Whole limb transplants were performed in genetically disparate mice. Balb/c mice (H2Kd) (Jackson Laboratory, Bar Harbour, ME) were recipients of limb allografts from C57Bl/6 mice (H-2Kb)inset in a heterotopic subcutaneous position in the groin. Recipients received no treatment or 500 μg MR1 (hamster anti-mouse anti-CD40L mAb; Bio Express, Inc., West Lebanon, NH) administered by intra-peritoneal (IP) injection on days 0, 2, 4, 6, 14, 28 and 60. Another group received vascularized myocutaneous allografts consisting of gracilis muscle and groin skin, and received the same MR1 therapy. The purpose of this group was to study the role of the bone marrow component of the limb allograft. The efficacy of anti-CD40L mAb was also studied in the murine nerve allograft model. C3H and C57BL/6 mice were chosen for full MHC-disparity. The study groups were composed of C3H recipients of nerve allografts from C57BL donors. The animals received either no treatment or anti-CD40L antibody (MR1, TSD Bioservices, Newark, DE) both topically to the graft and by IP injection on days 1, 3, 10, 18, and 28. Half of the animals in each group were randomly selected for sacrifice at three weeks post-engraftment, and the remaining animals were sacrificed at six weeks post-engraftment. Four genetically mismatched pairs of monkeys (Macaca fascicularis) received fivecentimeter ulnar nerve allografts. Treated animals received 10mg/kg of anti-CD40L mAb [IDEC Pharmaceuticals Corp., San Diego, CA] directly applied to the graft, and subsequent intravenous injections of 20mg/kg on post-op days 0, 1, 3, 10, 18, and 28, and monthly thereafter for a total of 6 months. Untreated allografts served as negative controls and autografts served as positive controls. Two of the treated and both untreated animals received 1cm2 skin auto-and allografts (SG) to allow monitoring of the rejection response. Electrophysiologic testing of the nerve grafts was performed at 6 months postoperatively, and the specimens were then harvested for histomorphometric analysis. Results: The transplantation of whole limb and nerve allografts was performed in experimental models across a major histocompatibity barrier. In a newly developed model of heterotopic limb transplantation in the mouse, therapy with anti-CD40 ligand (L) antibody produced long-term survival (>300 days) of whole limb allografts with differential rejection of the skin component. The bone marrow component appeared to play a significant role in prolonging allograft survival.. In the murine and non-human primate models of nerve allotransplantation, anti-CD40L antibody allowed axonal regeneration through nerve allografts across a long gap comparable to that seen in iso- and autografts. Conclusions: These findings suggest that CD40 blockade may significantly reduce the morbidity associated with immune modulation for successful composite tissue allotransplantation. This strategy has significant potential as the basis of combined regimens for the induction of donorspecific tolerance and could eliminate the possibility of chronic rejection in the long term. As single-agent therapy, CD40 blockade produces immune unresponsiveness that is well suited to the temporary immunosuppression required for nerve allograft transplantation. Table 1. Murine Limb Allograft Study Group 1. Allogeneic Limb Transplant Treatment Survival None 8, 9, 9, 10, 11 days 2. Allogeneic Limb Transplant MR1 500 g IP on days 0,2,4,6,14,28,60 3. Allogeneic Skin/Muscle Transplant MR1 500 g IP on days 0,2,4,6,14,28,60 Skin component: 90, 102, 82, 59, 40 days Musculoskeletal component: >300, >300, 240, 150, 120 days 15, 18, 19 days Fiber Count Fiber Width (m.) 2000 1500 1000 500 0 4 3 2 1 0 21 days 42 days 21 days 2 Neural Density (fibers/mm ) Percent Nerve 20 30000 15 20000 10 10000 5 0 42 days 0 21 days Isograft 42 days Anti-CD40L-treated Allograft 21 days 42 days Untreated Allograft Figure 1. Murine Nerve Allograft Study: Histomorphometric data including nerve fiber count, fiber width, neural density and percent nerve, demonstrate axonal regeneration in anti-CD40L mAb-treated allografts comparable to isografts. No regeneration seen in untreated allografts at 21-day timepoint. Primate Nerve Allograft Study: Nerve Graft Fiber Count # mAb SG Prox. auto Mid auto Prox. allo Mid allo 1 (+) (-) 13722 22762 2642 362 2 (+) (-) 13324 15665 9920 1051 3 (+) (-) 7200 6300 7526 9417 4 (+) (-) 9105 9584 8034 6212 5 (+) (+) 6328 4783 0 0 6 (-) (+) 1429 322 0 0 7 (-) (-) 4553 2217 n/a n/a 8 (-) (-) 7402 7231 n/a n/a 9 (+) (+) n/a n/a 0 0 10 (-) (+) n/a n/a 0 0 Table 2. Primate Nerve Allograft Study: Summary of histomorphometric data (fiber count) demonstrating good axonal regeneration in anti-CD40L mAb-treated allografts (without concomitant skin allograft) versus no regeneration in allograft recipients that were either untreated or treated but received a skin allograft.