Minutes February 11
advertisement

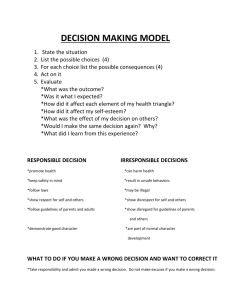
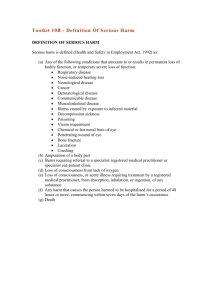
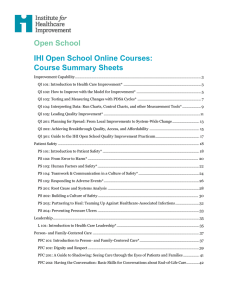
Glasgow Obstetrical & Gynaecological Society, 110th session www.gogs.org.uk Minutes of the Fourth Meeting of the 110th Session of the Glasgow Obstetrical and Gynaecological Society held in the Royal College of Physicians & Surgeons, St Vincent Street, Glasgow on 23rd February 2011 The President, Dr Elaine Melrose, was in the chair. Apologies were received from: Drs Lunan, McNay, Mackay, Kearney, Gemmell, Pringle, Perera Applications for membership were accepted for Dr Pamela Blair, proposed by Dr Jane Richmond, seconded by Dr Rita Panigrahy In attendance – 22 PRESENTATION Dr Melrose welcomed the speaker for the evening, Dr Jason Leitch, National Clinical Lead for Quality in the Scottish Government, who talked to the society on ‘What does quality mean in NHS Scotland?’. A dentist by trade, he is in the middle of a 5 year secondment to the Scottish Government. In Dr Leitch’s inspirational talk he started by encouraging us to read the Robert Francis report into Mid Staffordshire, particularly the raw testimony http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGui dance/DH_113018 He then encouraged us to realise that none of us is as good as we think we are, again recommending the writings of Atul Gawande, surgeon, author & writer for the New Yorker. In general, studies have shown that about 45% of patients get the appropriate care package, while 55% lack some aspect of care. About 25% of patients are harmed by coming into hospital eg by infection, drug error, wrong surgery etc. Systems for reporting have been archaic, relying on voluntary reporting. A scale of harm from A to I is used, with A-D being near misses, and I being death. Jason mentioned the reporting of maternal deaths and SCASSM which we are familiar with in obstetrics but admitted that this was not his area of expertise. He then compared ‘efficacy’ with ‘fidelity’ pointing out that much more money is spent on the former, which is based on research, compared with the latter which is much more important ie ‘getting information that is already known about out where it is needed’. About 90% of the harm caused in the health service is system based rather than because of bad medical practice. The example of the ‘Surgical Safety Checklist’ was given which has now been published by WHO. Its wide use has greatly reduced the harm caused to patients at the time of operation. The use of first names for staff was given as an example which reduced harm, encouraging a more open atmosphere in theatre. Many of the lessons we are learning now were learned by the airline industry 30 years ago. Another example was the use of checklists which again greatly reduced harm. Interestingly when asked if they would introduce a checklist, only 67% of surgeons said yes, but when asked if they would like one to be used if they were undergoing surgery, 99% said yes. One of the major ways to encourage reporting is to ensure a no blame culture. The aim is to see reporting rates rise significantly while actual events fall. Jason mentioned the Scottish Patient Safety Programme (http://www.patientsafetyalliance.scot.nhs.uk/programme) and the Institute for Healthcare Improvement (www.ihi.org) which he has been very involved with. The Scottish Safety Programme aims to reduce mortality in Scottish hospitals by 15% and adverse events by 30% between Jan 08 and Dec 12. The primary outcome is to develop and build a quality improvement and patient safety culture in our hospitals, with long term sustainability and capability to drive this approach at all levels. This will involve a culture change in staff. The model for improvement considers o What are we trying to accomplish o How will we know that a change is an improvement o What change can we make that will result in an improvement He described various interventions which have been studied eg ventilator acquired pneumonia bundle. This has led to a virtual eradication of VAP from ICU in Glasgow Royal Inf. The Hospital Standardised Mortality Rates (HSMR) in Scotland were then described showing various trends for different units. The fall is currently sitting at 5%. As the aim is a 15% reduction in hospital deaths, a significant amount of work needs to be done to achieve this. Jason assured us that it should be easier to achieve in 2011 than 2008 because of improved workforce (with SPSP fellows, improvement advisors, programme managers, infection control teams) along with an established ‘walkaround’ system, more non exec involvement and a higher profile of quality and safety at board level. The perinatal white paper published by ihi suggests drivers to reduce harm, providing woman centred care. http://www.ihi.org/IHI/topics/perinatalcare/perinatalcaregeneral http://www.ihi.org/IHI/Results/WhitePapers/IdealizedDesignofPerinatalCareWhitePaper.h tm Finally Jason mentioned the Healthcare Quality Strategy for NHSScotland which he said he would not have believed could have been produced when he first started. http://www.scotland.gov.uk/Resource/Doc/311667/0098354.pdf The 3 ambitions are to provide o Person centred care o Clinically effective care o Safe practice with no avoidable injury or harm to patients. At the end of his talk, Jason pointed out that while he had been speaking 27 patients would have been harmed while in hospital. There followed a lively question session at the end of which the vote of thanks was given by Dr Mathers. AOCB Dr Melrose thanked Hazel Newbigging of Hologic for their generous sponsorship. Members of the society were reminded that the next meeting is on 23rd March when Tim Overton, Consultant in Fetal Medicine Bristol will give the William Smellie Lecture “Expecting the Unexpected”. …………………………………………………President